Abstract
Background:
Our aim was to investigate the relationship between metabolic syndrome (MetS) and energy-dense nutrient-poor solid snacks intakes during 3.6 y of follow-up among children and adolescents.
Method:
This population-based longitudinal study was conducted within the framework of the Tehran Lipid and Glucose Study, on 424 MetS free subjects, aged 6–18 y. Data on consumption of energy-dense nutrient-poor solid snacks, sweet and salty snacks, were collected at baseline (2006–2008). Logistic regression, adjusted for age, sex, total energy intake, physical activity, dietary fiber, family history of diabetes, and body mass index, was used to assess the relationship between snacks and incident MetS.
Results:
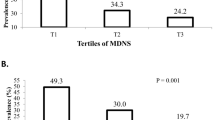
After adjustment for confounders, compared with the lowest quartile of total energy-dense nutrient-poor solid snacks, odds ratio of incident MetS in the highest quartile was 3.04 (95% confidence interval (CI): 1.11–8.49); for sweet snacks this was 2.88 (95% CI: 1.00–8.32), and for salty ones it was 2.85 (95% CI: 1.09–7.43). The risk of incident hypertension in the highest, compared with the lowest quartile of total and salty snacks, was 2.99 (95% CI: 1.00–8.93) and 3.35 (95% CI: 1.10–10.17), respectively.
Conclusion:
Energy-dense nutrient-poor solid snacks, both salty and sweet, may have undesirable effects on the incidence of MetS, with salty snacks having the potential to increase risk of incident hypertension in children and adolescents as well.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Cornier MA, Dabelea D, Hernandez TL, et al. The metabolic syndrome. Endocr Rev 2008;29:777–822.
Zimmet P, Alberti KG, Kaufman F, et al.; IDF Consensus Group. The metabolic syndrome in children and adolescents—an IDF consensus report. Pediatr Diabetes 2007;8:299–306.
Ghassemi H, Harrison G, Mohammad K. An accelerated nutrition transition in Iran. Public Health Nutr 2002;5:149–55.
Larson N, Story M. A review of snacking patterns among children and adolescents: what are the implications of snacking for weight status? Child Obes 2013;9:104–15.
Gregori D, Foltran F, Ghidina M, Berchialla P. Understanding the influence of the snack definition on the association between snacking and obesity: a review. Int J Food Sci Nutr 2011;62:270–5.
Gevers DW, Kremers SP, de Vries NK, van Assema P. Intake of energy-dense snack foods and drinks among Dutch children aged 7–12 years: how many, how much, when, where and which? Public Health Nutr 2015:1–10.
Bo S, De Carli L, Venco E, et al. Impact of snacking pattern on overweight and obesity risk in a cohort of 11- to 13-year-old adolescents. J Pediatr Gastroenterol Nutr 2014;59:465–71.
Vergetaki A, Linardakis M, Papadaki A, Kafatos A. Presence of metabolic syndrome and cardiovascular risk factors in adolescents and University students in Crete (Greece), according to different levels of snack consumption. Appetite 2011;57:278–85.
Keast DR, Nicklas TA, O’Neil CE. Snacking is associated with reduced risk of overweight and reduced abdominal obesity in adolescents: National Health and Nutrition Examination Survey (NHANES) 1999–2004. Am J Clin Nutr 2010;92:428–35.
Mirmiran P, Bahadoran Z, Delshad H, Azizi F. Effects of energy-dense nutrient-poor snacks on the incidence of metabolic syndrome: a prospective approach in Tehran Lipid and Glucose Study. Nutrition 2014;30:538–43.
Hosseinpour-Niazi S, Sohrab G, Asghari G, Mirmiran P, Moslehi N, Azizi F. Dietary glycemic index, glycemic load, and cardiovascular disease risk factors: Tehran Lipid and Glucose Study. Arch Iran Med 2013;16:401–7.
Patterson E, Wärnberg J, Kearney J, Sjöström M. Sources of saturated fat and sucrose in the diets of Swedish children and adolescents in the European Youth Heart Study: strategies for improving intakes. Public Health Nutr 2010;13:1955–64.
Ponzo V, Ganzit GP, Soldati L, et al. Blood pressure and sodium intake from snacks in adolescents. Eur J Clin Nutr 2015;69:681–6.
Ambrosini GL, Huang RC, Mori TA, et al. Dietary patterns and markers for the metabolic syndrome in Australian adolescents. Nutr Metab Cardiovasc Dis 2010;20:274–83.
He FJ, Marrero NM, Macgregor GA. Salt and blood pressure in children and adolescents. J Hum Hypertens 2008;22:4–11.
Kuipers RS, de Graaf DJ, Luxwolda MF, Muskiet MH, Dijck-Brouwer DA, Muskiet FA. Saturated fat, carbohydrates and cardiovascular disease. Neth J Med 2011;69:372–8.
Schwab U, Lauritzen L, Tholstrup T, et al. Effect of the amount and type of dietary fat on cardiometabolic risk factors and risk of developing type 2 diabetes, cardiovascular diseases, and cancer: a systematic review. Food Nutr Res 2014;58.
van der Horst K, Oenema A, Ferreira I, et al. A systematic review of environmental correlates of obesity-related dietary behaviors in youth. Health Educ Res 2007;22:203–26.
French SA, Story M, Jeffery RW. Environmental influences on eating and physical activity. Annu Rev Public Health 2001;22:309–35.
Swinburn BA, Caterson I, Seidell JC, James WP. Diet, nutrition and the prevention of excess weight gain and obesity. Public Health Nutr 2004;7:123–46.
Piernas C, Popkin BM. Trends in snacking among U.S. children. Health Aff (Millwood) 2010;29:398–404.
Weker H. [Simple obesity in children. A study on the role of nutritional factors]. Med Wieku Rozwoj 2006;10:3–191.
Kafatos A, Kouroumalis I, Vlachonikolis I, Theodorou C, Labadarios D. Coronary-heart-disease risk-factor status of the Cretan urban population in the 1980s. Am J Clin Nutr 1991;54:591–8.
Cohen DA, Sturm R, Scott M, Farley TA, Bluthenthal R. Not enough fruit and vegetables or too many cookies, candies, salty snacks, and soft drinks? Public Health Rep 2010;125:88–95.
Jenkins DJ, Wolever TM, Taylor RH, et al. Glycemic index of foods: a physiological basis for carbohydrate exchange. Am J Clin Nutr 1981;34:362–6.
Rouhani MH, Salehi-Abargouei A, Azadbakht L. Effect of glycemic index and glycemic load on energy intake in children. Nutrition 2013;29:1100–5.
Mozaffarian D, Pischon T, Hankinson SE, et al. Dietary intake of trans fatty acids and systemic inflammation in women. Am J Clin Nutr 2004;79:606–12.
Baer DJ, Judd JT, Clevidence BA, Tracy RP. Dietary fatty acids affect plasma markers of inflammation in healthy men fed controlled diets: a randomized crossover study. Am J Clin Nutr 2004;79:969–73.
Purkayastha S, Cai D. Neuroinflammatory basis of metabolic syndrome. Mol Metab 2013;2:356–63.
Andaki AC, Tinoco AL, Mendes EL, Andaki Júnior R, Hills AP, Amorim PR. Different waist circumference measurements and prediction of cardiovascular risk factors and metabolic syndrome in children. Obes Res Clin Pract 2012;6:e91–e174.
Koot BG, Westerhout R, Bohte AE, et al. Ultrasonography is not more reliable than anthropometry for assessing visceral fat in obese children. Pediatr Obes 2014;9:443–7.
Vance VA, Woodruff SJ, McCargar LJ, Husted J, Hanning RM. Self-reported dietary energy intake of normal weight, overweight and obese adolescents. Public Health Nutr 2009;12:222–7.
Johansson L, Solvoll K, Bjørneboe GE, Drevon CA. Under- and overreporting of energy intake related to weight status and lifestyle in a nationwide sample. Am J Clin Nutr 1998;68:266–74.
Olafsdottir AS, Thorsdottir I, Gunnarsdottir I, Thorgeirsdottir H, Steingrimsdottir L. Comparison of women’s diet assessed by FFQs and 24-hour recalls with and without underreporters: associations with biomarkers. Ann Nutr Metab 2006;50:450–60.
Azizi F, Ghanbarian A, Momenan AA, et al.; Tehran Lipid and Glucose Study Group. Prevention of non-communicable disease in a population in nutrition transition: Tehran Lipid and Glucose Study phase II. Trials 2009;10:5.
Panel on Macronutrients, Panel on the Definition of Dietary Fiber, Subcommittee on Upper Reference Levels of Nutrients, Subcommittee on Interpretation and Uses of Dietary Reference Intakes, and the Standing Committee on the Scientific Evaluation of Dietary Reference Intakes. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein and Amino Acids. Washington, DC: Institute of Medicine, Food and Nutrition Board. National Academies Press, 2005.
Delshad M, Ghanbarian A, Ghaleh NR, Amirshekari G, Askari S, Azizi F. Reliability and validity of the modifiable activity questionnaire for an Iranian urban adolescent population. Int J Prev Med 2015;6:3.
Mirmiran P, Esfahani FH, Mehrabi Y, Hedayati M, Azizi F. Reliability and relative validity of an FFQ for nutrients in the Tehran lipid and glucose study. Public Health Nutr 2010;13:654–62.
Esfahani FH, Asghari G, Mirmiran P, Azizi F. Reproducibility and relative validity of food group intake in a food frequency questionnaire developed for the Tehran Lipid and Glucose Study. J Epidemiol 2010;20:150–8.
Asghari G, Rezazadeh A, Hosseini-Esfahani F, Mehrabi Y, Mirmiran P, Azizi F. Reliability, comparative validity and stability of dietary patterns derived from an FFQ in the Tehran Lipid and Glucose Study. Br J Nutr 2012;108:1109–17.
Mirmiran P, Yuzbashian E, Asghari G, Hosseinpour-Niazi S, Azizi F. Consumption of sugar sweetened beverage is associated with incidence of metabolic syndrome in Tehranian children and adolescents. Nutr Metab (Lond) 2015;12:25.
Cook S, Weitzman M, Auinger P, Nguyen M, Dietz WH. Prevalence of a metabolic syndrome phenotype in adolescents: findings from the third National Health and Nutrition Examination Survey, 1988–1994. Arch Pediatr Adolesc Med 2003;157:821–7.
Kelishadi R, Gouya MM, Ardalan G, et al.; CASPIAN Study Group. First reference curves of waist and hip circumferences in an Asian population of youths: CASPIAN study. J Trop Pediatr 2007;53:158–64.
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 2004;114:555–76.
Genuth S, Alberti KG, Bennett P, et al.; Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care 2003;26:3160–7.
Alberti KG, Eckel RH, Grundy SM, et al.; International Diabetes Federation Task Force on Epidemiology and Prevention; Hational Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; International Association for the Study of Obesity. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009;120:1640–5.
Delavari A, Forouzanfar MH, Alikhani S, Sharifian A, Kelishadi R. First nationwide study of the prevalence of the metabolic syndrome and optimal cutoff points of waist circumference in the Middle East: the national survey of risk factors for noncommunicable diseases of Iran. Diabetes Care 2009;32:1092–7.
Acknowledgements
The authors thank the participants in the Tehran Lipid and Glucose Study for their enthusiastic support and the staff of the Tehran Lipid and Glucose Study Unit of the Research Institute for Endocrine Sciences for their valuable help. The authors also acknowledge Niloofar Shiva for critical editing of English grammar and syntax of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Asghari, G., Yuzbashian, E., Mirmiran, P. et al. Prediction of metabolic syndrome by a high intake of energy-dense nutrient-poor snacks in Iranian children and adolescents. Pediatr Res 79, 697–704 (2016). https://doi.org/10.1038/pr.2015.270
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/pr.2015.270
This article is cited by
-
Nutrient patterns in relation to metabolic health status in overweight and obese adolescents
Scientific Reports (2023)
-
Energy-dense nutrient-poor snacks and risk of non-alcoholic fattyliver disease: a case–control study in Iran
BMC Research Notes (2020)
-
The association of dietary patterns and adherence to WHO healthy diet with metabolic syndrome in children and adolescents: Tehran lipid and glucose study
BMC Public Health (2019)
-
Association of nuts and unhealthy snacks with subclinical atherosclerosis among children and adolescents with overweight and obesity
Nutrition & Metabolism (2019)