Abstract
Background:
Intrauterine growth restriction (IUGR) followed by postnatal accelerated growth (CG-IUGR) is associated with long-term adverse metabolic consequences, and an involvement of epigenetic dysregulation has been implicated. Peroxisome proliferator–activated receptor-γ coactivator-1α (PGC-1α) is a key orchestrator in energy homeostasis. We hypothesized that CG-IUGR programed an insulin-resistant phenotype through the alteration in DNA methylation and transcriptional activity of PGC-1α.
Methods:
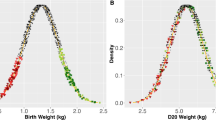
A CG-IUGR rat model was adopted using maternal gestational nutritional restriction followed by infantile overnutrition achieved by reducing the litter size. The DNA methylation was determined by pyrosequencing. The mRNA expression and mitochondrial content were assessed by real-time PCR. The insulin-signaling protein expression was evaluated by western blotting.
Results:
Compared with controls, the CG-IUGR rats showed an increase in the DNA methylation of specific CpG sites in PGC-1α, and a decrease in the transcriptional activity of PGC-1α, mitochondrial content, protein level of PI3K and phosphorylated-Akt2 in liver and muscle tissues. The methylation of specific CpG sites in PGC-1α was positively correlated with fasting insulin concentration.
Conclusion:
IUGR followed by infantile overnutrition programs an insulin-resistant phenotype, possibly through the alteration in DNA methylation and transcriptional activity of PGC-1α. The genetic and epigenetic modifications of PGC-1α provide a potential mechanism linking early-life nutrition insult to long-term metabolic disease susceptibilities.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Barker DJ, Hales CN, Fall CH, Osmond C, Phipps K, Clark PM. Type 2 (non-insulin-dependent) diabetes mellitus, hypertension and hyperlipidaemia (syndrome X): relation to reduced fetal growth. Diabetologia 1993;36:62–7.
Hales CN, Barker DJ, Clark PM, et al. Fetal and infant growth and impaired glucose tolerance at age 64. BMJ 1991;303:1019–22.
Bhuiyan AR, Chen W, Srinivasan SR, Azevedo MJ, Berenson GS. Relationship of low birth weight to pulsatile arterial function in asymptomatic younger adults: the Bogalusa Heart Study. Am J Hypertens 2010;23:168–73.
Hernández MI, Mericq V. Metabolic syndrome in children born small-for-gestational age. Arq Bras Endocrinol Metabol 2011;55:583–9.
Mericq V. Low birth weight and endocrine dysfunction in postnatal life. Pediatr Endocrinol Rev 2006;4:3–14.
Roghair RD, Aldape G. Naturally occurring perinatal growth restriction in mice programs cardiovascular and endocrine function in a sex- and strain-dependent manner. Pediatr Res 2007;62:399–404.
Lim JS, Lee JA, Hwang JS, Shin CH, Yang SW. Non-catch-up growth in intrauterine growth-retarded rats showed glucose intolerance and increased expression of PDX-1 mRNA. Pediatr Int 2011;53:181–6.
Ong KK. Catch-up growth in small for gestational age babies: good or bad? Curr Opin Endocrinol Diabetes Obes 2007;14:30–4.
Ehrenkranz RA, Dusick AM, Vohr BR, Wright LL, Wrage LA, Poole WK. Growth in the neonatal intensive care unit influences neurodevelopmental and growth outcomes of extremely low birth weight infants. Pediatrics 2006;117:1253–61.
Casey PH, Whiteside-Mansell L, Barrett K, Bradley RH, Gargus R. Impact of prenatal and/or postnatal growth problems in low birth weight preterm infants on school-age outcomes: an 8-year longitudinal evaluation. Pediatrics 2006;118:1078–86.
Faienza MF, Brunetti G, Ventura A, et al. Nonalcoholic fatty liver disease in prepubertal children born small for gestational age: influence of rapid weight catch-up growth. Horm Res Paediatr 2013;79:103–9.
Berends LM, Fernandez-Twinn DS, Martin-Gronert MS, Cripps RL, Ozanne SE. Catch-up growth following intra-uterine growth-restriction programmes an insulin-resistant phenotype in adipose tissue. Int J Obes (Lond) 2013;37:1051–7.
Hermann GM, Miller RL, Erkonen GE, et al. Neonatal catch up growth increases diabetes susceptibility but improves behavioral and cardiovascular outcomes of low birth weight male mice. Pediatr Res 2009;66:53–8.
Heijmans BT, Tobi EW, Stein AD, et al. Persistent epigenetic differences associated with prenatal exposure to famine in humans. Proc Natl Acad Sci USA 2008;105:17046–9.
Plagemann A, Roepke K, Harder T, et al. Epigenetic malprogramming of the insulin receptor promoter due to developmental overfeeding. J Perinat Med 2010;38:393–400.
Fernandez-Marcos PJ, Auwerx J. Regulation of PGC-1α, a nodal regulator of mitochondrial biogenesis. Am J Clin Nutr 2011;93:884S–90.
Ling C, Del Guerra S, Lupi R, et al. Epigenetic regulation of PPARGC1A in human type 2 diabetic islets and effect on insulin secretion. Diabetologia 2008;51:615–22.
Sookoian S, Rosselli MS, Gemma C, et al. Epigenetic regulation of insulin resistance in nonalcoholic fatty liver disease: impact of liver methylation of the peroxisome proliferator-activated receptor γ coactivator 1α promoter. Hepatology 2010;52:1992–2000.
Brøns C, Jacobsen S, Nilsson E, et al. Deoxyribonucleic acid methylation and gene expression of PPARGC1A in human muscle is influenced by high-fat overfeeding in a birth-weight-dependent manner. J Clin Endocrinol Metab 2010;95:3048–56.
Zheng RD, Liao LH, Ye J, et al. Effects of SOCS 1/3 gene silencing on the expression of C/EBPα and PPARγ during differentiation and maturation of rat preadipocytes. Pediatr Res 2013;73:263–7.
Ye J, Zheng R, Wang Q, et al. Downregulating SOCS3 with siRNA ameliorates insulin signaling and glucose metabolism in hepatocytes of IUGR rats with catch-up growth. Pediatr Res 2012;72:550–9.
Liao L, Zheng R, Wang C, et al. The influence of down-regulation of suppressor of cellular signaling proteins by RNAi on glucose transport of intrauterine growth retardation rats. Pediatr Res 2011;69:497–503.
Suzuki MM, Bird A. DNA methylation landscapes: provocative insights from epigenomics. Nat Rev Genet 2008;9:465–76.
Gemma C, Sookoian S, Alvariñas J, et al. Maternal pregestational BMI is associated with methylation of the PPARGC1A promoter in newborns. Obesity (Silver Spring) 2009;17:1032–9.
Zeng Y, Gu P, Liu K, Huang P. Maternal protein restriction in rats leads to reduced PGC-1α expression via altered DNA methylation in skeletal muscle. Mol Med Rep 2013;7:306–12.
Pooya S, Blaise S, Moreno Garcia M, et al. Methyl donor deficiency impairs fatty acid oxidation through PGC-1α hypomethylation and decreased ER-α, ERR-α, and HNF-4α in the rat liver. J Hepatol 2012;57:344–51.
Barrès R, Osler ME, Yan J, et al. Non-CpG methylation of the PGC-1alpha promoter through DNMT3B controls mitochondrial density. Cell Metab 2009;10:189–98.
Barrès R, Yan J, Egan B, et al. Acute exercise remodels promoter methylation in human skeletal muscle. Cell Metab 2012;15:405–11.
Gillberg L, Jacobsen SC, Jacobsen S, et al. Does DNA methylation of PPARGC1A influence insulin action in first degree relatives of patients with type 2 diabetes? PLoS One 2013;8:e58384.
Burgueño AL, Cabrerizo R, Gonzales Mansilla N, Sookoian S, Pirola CJ. Maternal high-fat intake during pregnancy programs metabolic-syndrome-related phenotypes through liver mitochondrial DNA copy number and transcriptional activity of liver PPARGC1A. J Nutr Biochem 2013;24:6–13.
Estall JL, Kahn M, Cooper MP, et al. Sensitivity of lipid metabolism and insulin signaling to genetic alterations in hepatic peroxisome proliferator-activated receptor-gamma coactivator-1alpha expression. Diabetes 2009;58:1499–508.
Burri L, Thoresen GH, Berge RK. The Role of PPARα Activation in Liver and Muscle. PPAR Res 2010;2010:.
Abbas A, Blandon J, Rude J, Elfar A, Mukherjee D. PPAR-γ agonist in treatment of diabetes: cardiovascular safety considerations. Cardiovasc Hematol Agents Med Chem 2012;10:124–34.
Heikens MJ, Gorbach AM, Eden HS, et al. Core body temperature in obesity. Am J Clin Nutr 2011;93:963–7.
Leites GT, Sehl PL, Cunha Gdos S, Detoni Filho A, Meyer F. Responses of obese and lean girls exercising under heat and thermoneutral conditions. J Pediatr 2013;162:1054–60.
Hynd PI, Czerwinski VH, McWhorter TJ. Is propensity to obesity associated with the diurnal pattern of core body temperature? Int J Obes (Lond) 2014;38:231–5.
Novak CM, Kotz CM, Levine JA. Central orexin sensitivity, physical activity, and obesity in diet-induced obese and diet-resistant rats. Am J Physiol Endocrinol Metab 2006;290:E396–403.
Zhu C, Zhang X, Qiao H, et al. The intrinsic PEDF is regulated by PPARγ in permanent focal cerebral ischemia of rat. Neurochem Res 2012;37:2099–107.
Qiu BY, Turner N, Li YY, et al. High-throughput assay for modulators of mitochondrial membrane potential identifies a novel compound with beneficial effects on db/db mice. Diabetes 2010;59:256–65.
Vanattou-Saïfoudine N, McNamara R, Harkin A. Mechanisms mediating the ability of caffeine to influence MDMA (‘Ecstasy’)-induced hyperthermia in rats. Br J Pharmacol 2010;160:860–77.
Acknowledgements
We thank Professors Kenneth McCormick and Gail Mick from the Department of Pediatrics, Endocrine Division, University of Alabama at Birmingham (UAB), Birmingham, AL, USA, for their assistance with the English language editing and manuscript composition.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Xie, X., Lin, T., Zhang, M. et al. IUGR with infantile overnutrition programs an insulin-resistant phenotype through DNA methylation of peroxisome proliferator–activated receptor-γ coactivator-1α in rats. Pediatr Res 77, 625–632 (2015). https://doi.org/10.1038/pr.2015.32
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/pr.2015.32
This article is cited by
-
LRP6 Bidirectionally Regulates Insulin Sensitivity through Insulin Receptor and S6K Signaling in Rats with CG-IUGR
Current Medical Science (2023)
-
Paternal eNOS deficiency in mice affects glucose homeostasis and liver glycogen in male offspring without inheritance of eNOS deficiency itself
Diabetologia (2022)