Abstract
Background:
Only a few studies have systemically analyzed the association between neonatal jaundice and childhood-onset allergic diseases.
Methods:
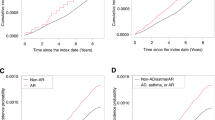
From 2000 to 2007, 27,693 neonates with newly diagnosed neonatal jaundice and 55,367 matched nonneonatal jaundice cohorts were identified. The incidences and hazard ratios (HRs) of five allergic diseases, namely allergic conjunctivitis (AC), allergic rhinitis (AR), atopic dermatitis (AD), asthma, and urticaria, by the end of 2008 were calculated.
Results:
The incidence density and HRs of the five allergic diseases were greater in the neonatal jaundice cohort than in the nonneonatal jaundice cohort, and the HRs declined modestly with age. The HRs for AR (HR = 2.51, 95% confidence interval (CI) = 2.43–2.59) and AD (HR = 2.51, 95% CI = 2.40–2.62) were the highest, and that for urticaria was the lowest (HR = 2.06, 95% CI = 1.94–2.19). The HRs of allergic diseases were substantially greater for boys and those requiring phototherapy. The HRs of the allergic diseases, except urticaria (HR = 2.49, 95% CI = 1.57–3.97), were not significantly different between the neonatal jaundice regardless of whether the patients received exchange transfusion.
Conclusion:
Neonatal jaundice is associated with the development of allergic diseases in early childhood.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Lauer BJ, Spector ND. Hyperbilirubinemia in the newborn. Pediatr Rev 2011;32:341–9.
Wennberg RP, Ahlfors CE, Bhutani VK, Johnson LH, Shapiro SM . Toward understanding kernicterus: a challenge to improve the management of jaundiced newborns. Pediatrics 2006:117:474–85.
Atkinson M, Budge H. Review of the NICE guidance on neonatal jaundice. Arch Dis Child Educ Pract Ed 2011;96:136–40.
Newman TB, Escobar GJ, Gonzales VM, Armstrong MA, Gardner MN, Folck BF. Frequency of neonatal bilirubin testing and hyperbilirubinemia in a large health maintenance organization. Pediatrics 1999;104(5 Pt 2):1198–203.
Bélanger S, Lavoie JC, Chessex P. Influence of bilirubin on the antioxidant capacity of plasma in newborn infants. Biol Neonate 1997;71:233–8.
Minetti M, Mallozzi C, Di Stasi AM, Pietraforte D. Bilirubin is an effective antioxidant of peroxynitrite-mediated protein oxidation in human blood plasma. Arch Biochem Biophys 1998;352:165–74.
Jangi S, Otterbein L, Robson S. The molecular basis for the immunomodulatory activities of unconjugated bilirubin. Int J Biochem Cell Biol 2013;45:2843–51.
Haga Y, Tempero MA, Kay D, Zetterman RK. Intracellular accumulation of unconjugated bilirubin inhibits phytohemagglutin-induced proliferation and interleukin-2 production of human lymphocytes. Dig Dis Sci 1996;41:1468–74.
Romagnani S. The Th1/Th2 paradigm. Immunol Today 1997;18:263–6.
Romagnani S. The role of lymphocytes in allergic disease. J Allergy Clin Immunol 2000;105:399–408.
Aspberg S, Dahlquist G, Kahan T, Källén B. Is neonatal phototherapy associated with an increased risk for hospitalized childhood bronchial asthma? Pediatr Allergy Immunol 2007;18:313–9.
Aspberg S, Dahlquist G, Kahan T, Källén B. Confirmed association between neonatal phototherapy or neonatal icterus and risk of childhood asthma. Pediatr Allergy Immunol 2010;21(4 Pt 2):e733–9.
Ku MS, Sun HL, Sheu JN, Lee HS, Yang SF, Lue KH. Neonatal jaundice is a risk factor for childhood asthma: a retrospective cohort study. Pediatr Allergy Immunol 2012;23:623–8.
Huang LS, Bao YX, Xu ZL, et al. Neonatal Bilirubin Levels and Childhood Asthma in the US Collaborative Perinatal Project, 1959–1965. Am J Epidemiol 2013;178:1691–7.
Sun HL, Lue KH, Ku MS. Neonatal jaundice is a risk factor for childhood allergic rhinitis: a retrospective cohort study. Am J Rhinol Allergy 2013;27:192–6.
Källén B, Finnström O, Nygren KG, Otterblad Olausson P. Association between preterm birth and intrauterine growth retardation and child asthma. Eur Respir J 2013;41:671–6.
Crump C, Winkleby MA, Sundquist J, Sundquist K. Risk of asthma in young adults who were born preterm: a Swedish national cohort study. Pediatrics 2011;127:e913–20.
Kurt A, Aygun AD, Kurt AN, Godekmerdan A, Akarsu S, Yilmaz E. Use of phototherapy for neonatal hyperbilirubinemia affects cytokine production and lymphocyte subsets. Neonatology 2009;95:262–6.
Procianoy RS, Silveira RC, Fonseca LT, Heidemann LA, Neto EC. The influence of phototherapy on serum cytokine concentrations in newborn infants. Am J Perinatol 2010;27:375–9.
Aycicek A, Kocyigit A, Erel O, Senturk H. Phototherapy causes DNA damage in peripheral mononuclear leukocytes in term infants. J Pediatr (Rio J) 2008;84:141–6.
Tatli MM, Minnet C, Kocyigit A, Karadag A. Phototherapy increases DNA damage in lymphocytes of hyperbilirubinemic neonates. Mutat Res 2008;654:93–5.
Maverakis E, Miyamura Y, Bowen MP, Correa G, Ono Y, Goodarzi H. Light, including ultraviolet. J Autoimmun 2010;34:J247–57.
Gloria-Bottini F, Bottini E. Is there a role of early neonatal events in susceptibility to allergy? Int J Biomed Sci 2010;6:8–12.
Ahlfors CE. Criteria for exchange transfusion in jaundiced newborns. Pediatrics 1994;93:488–94.
Johnson LH, Bhutani VK, Brown AK. System-based approach to management of neonatal jaundice and prevention of kernicterus. J Pediatr 2002;140:396–403.
La Rosa M, Romeo MG, Pratico G, Rizzo R, Mollica F. Serum IgE in newborns undergoing exchange transfusion. Ann Allergy 1986;57:259–62.
Gilliland FD, Li YF, Saxon A, Diaz-Sanchez D. Effect of glutathione-S-transferase M1 and P1 genotypes on xenobiotic enhancement of allergic responses: randomised, placebo-controlled crossover study. Lancet 2004;363:119–25.
Safronova OG, Vavilin VA, Lyapunova AA, et al. Relationship between glutathione S-transferase P1 polymorphism and bronchial asthma and atopic dermatitis. Bull Exp Biol Med 2003;136:73–5.
Abdel Ghany EA, Hussain NF, Botros SK. Glutathione S-transferase gene polymorphisms in neonatal hyperbilirubinemia. J Investig Med 2012;60:18–22.
Piacentini S, Polimanti R, Simonelli I, et al. Glutathione S-transferase polymorphisms, asthma susceptibility and confounding variables: a meta-analysis. Mol Biol Rep 2013;40:3299–313.
Raimondi F, Indrio F, Crivaro V, Araimo G, Capasso L, Paludetto R. Neonatal hyperbilirubinemia increases intestinal protein permeability and the prevalence of cow’s milk protein intolerance. Acta Paediatr 2008;97:751–3.
Setia S, Villaveces A, Dhillon P, Mueller BA. Neonatal jaundice in Asian, white, and mixed-race infants. Arch Pediatr Adolesc Med 2002;156:276–9.
Davis K, Huang AT. Learning from Taiwan: experience with universal health insurance. Ann Intern Med 2008;148:313–4.
Wei CC, Tsai JD, Lin CL, Shen TC, Li TC, Chung CJ. Increased risk of idiopathic nephrotic syndrome in children with atopic dermatitis. Pediatr Nephrol 2014;29:2157–63.
Wei CC, Lin CL, Shen TC, Tsai JD, Chung CJ, Li TC. Increased incidence of juvenile-onset systemic lupus erythematosus among children with asthma. Pediatr Allergy Immunol 2014;25:374–9.
Wei CC, Lin CL, Kao CH, et al. Increased risk of Kawasaki disease in children with common allergic diseases. Ann Epidemiol 2014;24:340–3.
Tsai JD, Lin CL, Shen TC, Li TC, Wei CC. Increased subsequent risk of myasthenia gravis in children with allergic diseases. J Neuroimmunol 2014;276:202–6.
Kao CC, Huang JL, Ou LS, See LC. The prevalence, severity and seasonal variations of asthma, rhinitis and eczema in Taiwanese schoolchildren. Pediatr Allergy Immunol 2005;16:408–15.
Liao PF, Sun HL, Lu KH, Lue KH. Prevalence of childhood allergic diseases in central Taiwan over the past 15 years. Pediatr Neonatol 2009;50:18–25.
Tsai YJ, Lin CH, Fu LS, Fu YC, Lin MC, Jan SL. The association between Kawasaki disease and allergic diseases, from infancy to school age. Allergy Asthma Proc 2013;34:467–72.
Acknowledgements
C.-C.W. and T.-C.S. conceptualized and designed the study, drafted the initial manuscript, and approved the final submitted manuscript. C.-L.L. and C.-H.K. conducted the initial analysis, reviewed and revised the manuscript, and approved the final submitted manuscript. C.-H.K. coordinated and supervised data collection, critically reviewed the manuscript, and approved the final submitted manuscript.
Author information
Authors and Affiliations
Corresponding author
PowerPoint slides
Rights and permissions
About this article
Cite this article
Wei, CC., Lin, CL., Shen, TC. et al. Neonatal jaundice and risks of childhood allergic diseases: a population-based cohort study. Pediatr Res 78, 223–230 (2015). https://doi.org/10.1038/pr.2015.89
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/pr.2015.89
This article is cited by
-
Urinary lumirubin excretion in jaundiced preterm neonates during phototherapy with blue light-emitting diode vs. green fluorescent lamp
Scientific Reports (2023)
-
Enhanced early prediction of clinically relevant neonatal hyperbilirubinemia with machine learning
Pediatric Research (2019)
-
Neuro-inflammatory effects of photodegradative products of bilirubin
Scientific Reports (2018)
-
Prevalence of suicide attempts and their risk factors in school-aged patients with epilepsy: a population-based study
European Child & Adolescent Psychiatry (2018)
-
Epidemiology and risk of juvenile idiopathic arthritis among children with allergic diseases: a nationwide population-based study
Pediatric Rheumatology (2016)