Abstract
Background:
We examined recent trends and interhospital variation in use of indomethacin, ibuprofen, and surgical ligation for patent ductus arteriosus (PDA) in very-low-birth-weight (VLBW) infants.
Methods:
Included in this retrospective study of the Pediatric Hospital Information System database were 13,853 VLBW infants from 19 US children’s hospitals, admitted at age < 3 d between 1 January 2005 and 31 December 2014. PDA management and in-hospital outcomes were examined for trends and variation.
Results:
PDA was diagnosed in 5,719 (42%) VLBW infants. Cyclooxygenase inhibitors and/or ligation were used in 74% of infants with PDA overall, however studied hospitals varied greatly in PDA management. Odds of any cyclooxygenase inhibitor or surgical treatment for PDA decreased 11% per year during the study period. This was temporally associated with improved survival but also with increasing bronchopulmonary dysplasia, periventricular leukomalacia, retinopathy of prematurity, and acute renal failure in unadjusted analyses. There was no detectable correlation between hospital-specific changes in PDA management and hospital-specific changes in outcomes of preterm birth during the study period.
Conclusion:
Use of cyclooxygenase inhibitors and ligation for PDA in VLBW infants decreased over a 10-y period at the studied hospitals. Further evidence is needed to assess the impact of this change in PDA management.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Vermont Oxford Network. Nightingale Database. Network Databases 2016; (https://nightingale.vtoxford.org/home.aspx).
Clyman RI, Couto J, Murphy GM. Patent ductus arteriosus: are current neonatal treatment options better or worse than no treatment at all? Semin Perinatol 2012;36:123–9.
Benitz WE. Learning to live with patency of the ductus arteriosus in preterm infants. J Perinatol 2011;31 Suppl 1:S42–8.
Benitz W. Patent ductus arteriosus: to treat or not to treat? Arch Dis Child Fetal Neonatal Ed 2012;97:F80–2.
Clyman RI, Chorne N. Patent ductus arteriosus: evidence for and against treatment. J Pediatr 2007;150:216–9.
Cotton RB, Stahlman MT, Bender HW, Graham TP, Catterton WZ, Kovar I. Randomized trial of early closure of symptomatic patent ductus arteriosus in small preterm infants. J Pediatr 1978;93:647–51.
Cotton RB, Stahlman MT, Kovar I, Catterton WZ. Medical management of small preterm infants with symptomatic patent ductus arteriosus. J Pediatr 1978;92:467–73.
Kitterman JA, Edmunds LH Jr, Gregory GA, Heymann MA, Tooley WH, Rudolph AM. Patent ducts arteriosus in premature infants. Incidence, relation to pulmonary disease and management. N Engl J Med 1972;287:473–7.
Madan JC, Kendrick D, Hagadorn JI, Frantz ID 3rd ; National Institute of Child Health and Human Development Neonatal Research Network. Patent ductus arteriosus therapy: impact on neonatal and 18-month outcome. Pediatrics 2009;123:674–81.
Chorne N, Leonard C, Piecuch R, Clyman RI. Patent ductus arteriosus and its treatment as risk factors for neonatal and neurodevelopmental morbidity. Pediatrics 2007;119:1165–74.
Jensen EA, Schmidt B. Epidemiology of bronchopulmonary dysplasia. Birth Defects Res A Clin Mol Teratol 2014;100:145–57.
Benitz WE. Treatment of persistent patent ductus arteriosus in preterm infants: time to accept the null hypothesis? J Perinatol 2010;30:241–52.
Sosenko IR, Fajardo MF, Claure N, Bancalari E. Timing of patent ductus arteriosus treatment and respiratory outcome in premature infants: a double-blind randomized controlled trial. J Pediatr 2012;160:929–35.e1.
Schmidt B, Roberts RS, Fanaroff A, et al.; TIPP Investigators. Indomethacin prophylaxis, patent ductus arteriosus, and the risk of bronchopulmonary dysplasia: further analyses from the Trial of Indomethacin Prophylaxis in Preterms (TIPP). J Pediatr 2006;148:730–4.
Bose CL, Laughon M. Treatment to prevent patency of the ductus arteriosus: beneficial or harmful? J Pediatr 2006;148:713–4.
Bose CL, Laughon M. Patent ductus arteriosus: lack of evidence for common treatments. Arch Dis Child Fetal Neonatal Ed 2007;92:F498–502.
Clyman RI. Surgical ligation of the patent ductus arteriosus: treatment or morbidity? J Pediatr 2012;161:583–4.
Jhaveri N, Moon-Grady A, Clyman RI. Early surgical ligation versus a conservative approach for management of patent ductus arteriosus that fails to close after indomethacin treatment. J Pediatr 2010;157:381–7, 387.e1.
Laughon MM, Simmons MA, Bose CL. Patency of the ductus arteriosus in the premature infant: is it pathologic? Should it be treated? Curr Opin Pediatr 2004;16:146–51.
Vanhaesebrouck S, Zonnenberg I, Vandervoort P, Bruneel E, Van Hoestenberghe M, Theyskens C. Conservative treatment for patent ductus arteriosus in the preterm. Arch Dis Child Fetal Neonatal Ed 2007;92:F244–7.
Petitti DB. Associations are not effects. Am J Epidemiol 1991;133:101–2.
Weinberg J, Evans F, Burns K, Pearson G, Kaltman J. Surgical ligation of patent ductus arteriosus in premature infants: trends and practice variation. Cardiol Young 2015:1–8.
Slaughter JL, Reagan PB, Bapat RV, Newman TB, Klebanoff MA. Nonsteroidal anti-inflammatory administration and patent ductus arteriosus ligation, a survey of practice preferences at US children’s hospitals. Eur J Pediatr 2016;175:775–83.
Horbar JD, Carpenter JH, Badger GJ, et al. Mortality and neonatal morbidity among infants 501 to 1500 grams from 2000 to 2009. Pediatrics 2012;129:1019–26.
Shah S, Ohlsson A. Ibuprofen for the prevention of patent ductus arteriosus in preterm and/or low birth weight infants. Cochrane Database Syst Rev 2006:CD004213.
Cooke L, Steer P, Woodgate P. Indomethacin for asymptomatic patent ductus arteriosus in preterm infants. Cochrane Database Syst Rev 2003:CD003745.
Le J, Gales MA, Gales BJ. Acetaminophen for patent ductus arteriosus. Ann Pharmacother 2015;49:241–6.
European Medicines Agency. The European Union Clinical Trials Register. 2016; (https://www.clinicaltrialsregister.eu).
US National Institutes of Health. ClinicalTrials.gov. 2016; (https://clinicaltrials.gov).
World Health Organization. International Clinical Trials Registry Platform (ICTRP). 2016; (http://www.who.int/ictrp/en).
Children’s Hospital Association. Pediatric Health Information System. Programs and Services: Data Analytics and Research 2015; (https://www.childrenshospitals.org/Programs-and-Services/Data-Analytics-and-Research/Pediatric-Health-Information-System).
Raudenbush S, Bryk A. Hierarchical Linear Models: Applications and Data Analysis Methods. 2nd edn. Thousand Oaks, CA: Sage Publications; 2002.
Glickman ME, Rao SR, Schultz MR. False discovery rate control is a recommended alternative to Bonferroni-type adjustments in health studies. J Clin Epidemiol 2014;67:850–7.
Author information
Authors and Affiliations
Corresponding author
Supplementary information
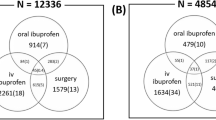
Supplementary Figure S1
(TIFF 1703 kb)
PowerPoint slides
Rights and permissions
About this article
Cite this article
Hagadorn, J., Brownell, E., Trzaski, J. et al. Trends and variation in management and outcomes of very low-birth-weight infants with patent ductus arteriosus. Pediatr Res 80, 785–792 (2016). https://doi.org/10.1038/pr.2016.166
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/pr.2016.166
This article is cited by
-
Patent ductus arteriosus treatment trends and associated morbidities in neonates
Scientific Reports (2021)
-
Is late treatment with acetaminophen safe and effective in avoiding surgical ligation among extremely preterm neonates with persistent patent ductus arteriosus?
Journal of Perinatology (2021)
-
Covariation of changing patent ductus arteriosus management and preterm infant outcomes in Pediatrix neonatal intensive care units
Journal of Perinatology (2021)
-
Outcomes in infants < 29 weeks of gestation following single-dose prophylactic indomethacin
Journal of Perinatology (2021)
-
Ductal ligation timing and neonatal outcomes: a 12-year bicentric comparison
European Journal of Pediatrics (2021)