Abstract
Background:
Abnormal PCO2 is common in infants with hypoxic ischemic encephalopathy (HIE). The objective was to determine whether hypocapnia was independently associated with unfavorable outcome (death or severe neurodevelopmental disability at 18 mo) in infants with moderate-to-severe HIE.
Methods:
This was a post hoc analysis of the CoolCap Study in which infants were randomized to head cooling or standard care. Blood gases were measured at prespecified times after randomization. PCO2 and follow-up data were available for 196 of 234 infants. Analyses were performed to investigate the relationship between hypocapnia in the first 72 h after randomization and unfavorable outcome.
Results:
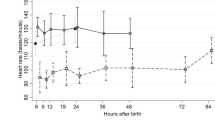
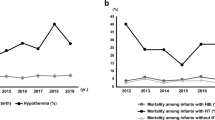
After adjusting for pH, amplitude-integrated electroencephalogram background and seizures, birth weight, Apgar score at 5 min, cooling status, and Sarnat stage, PCO2 was inversely associated with unfavorable outcome (P < 0.001). The probability of unfavorable outcome was 0.20 ± 0.1 (point estimate ± SE), 0.53 ± 0.23 and 0.89 ± 0.16 for a PCO2 of 40, 30, and 20 mm Hg respectively and was greater in infants with severe HIE than with moderate HIE.
Conclusions:
Hypocapnia in infants with moderate-to-severe HIE was independently associated with unfavorable outcome. Future studies of controlled normocapnia will be important.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Kety SS, Schmidt CF. Effects of alterations in the arterial tensions of carbon dioxide and oxygen on cerebral blood flow and cerebral oxygen consumption of normal young men. Fed Proc 1946;5(1 Pt 2):55.
Fritz KI, Ashraf QM, Mishra OP, Delivoria-Papadopoulos M. Effect of moderate hypocapnic ventilation on nuclear DNA fragmentation and energy metabolism in the cerebral cortex of newborn piglets. Pediatr Res 2001;50:586–9.
Giannakopoulou C, Korakaki E, Manoura A, et al. Significance of hypocarbia in the development of periventricular leukomalacia in preterm infants. Pediatr Int 2004;46:268–73.
Kubota M, Matsuda F, Hashizume M, Nakamura T, Nishida A. Periventricular leukomalacia associated with hypocarbia. Acta Paediatr Jpn 1996;38:57–60.
Liao SL, Lai SH, Chou YH, Kuo CY. Effect of hypocapnia in the first three days of life on the subsequent development of periventricular leukomalacia in premature infants. Acta Paediatr Taiwan 2001;42:90–3.
Murase M, Ishida A. Early hypocarbia of preterm infants: its relationship to periventricular leukomalacia and cerebral palsy, and its perinatal risk factors. Acta Paediatr 2005;94:85–91.
Okumura A, Toyota N, Hayakawa F, et al. Cerebral hemodynamics during early neonatal period in preterm infants with periventricular leukomalacia. Brain Dev 2002;24:693–7.
Okumura A, Hayakawa F, Kato T, et al. Hypocarbia in preterm infants with periventricular leukomalacia: the relation between hypocarbia and mechanical ventilation. Pediatrics 2001;107:469–75.
Shankaran S, Langer JC, Kazzi SN, Laptook AR, Walsh M ; National Institute of Child Health and Human Development Neonatal Research Network. Cumulative index of exposure to hypocarbia and hyperoxia as risk factors for periventricular leukomalacia in low birth weight infants. Pediatrics 2006;118:1654–9.
Wiswell TE, Graziani LJ, Kornhauser MS, et al. Effects of hypocarbia on the development of cystic periventricular leukomalacia in premature infants treated with high-frequency jet ventilation. Pediatrics 1996;98:918–24.
Fujimoto S, Togari H, Yamaguchi N, Mizutani F, Suzuki S, Sobajima H. Hypocarbia and cystic periventricular leukomalacia in premature infants. Arch Dis Child 1994;71:F107–10.
Klinger G, Beyene J, Shah P, Perlman M. Do hyperoxaemia and hypocapnia add to the risk of brain injury after intrapartum asphyxia? Arch Dis Child Fetal Neonatal Ed 2005;90:F49–52.
Pappas A, Shankaran S, Laptook AR, et al.; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Hypocarbia and adverse outcome in neonatal hypoxic-ischemic encephalopathy. J Pediatr 2011;158:752–758.e1.
Gluckman PD, Wyatt JS, Azzopardi D, et al. Selective head cooling with mild systemic hypothermia after neonatal encephalopathy: multicentre randomised trial. Lancet 2005;365:663–70.
Jensen EC, Bennet L, Hunter CJ, Power GC, Gunn AJ. Post-hypoxic hypoperfusion is associated with suppression of cerebral metabolism and increased tissue oxygenation in near-term fetal sheep. J Physiol 2006;572(Pt 1):131–9.
Sarnat HB, Sarnat MS. Neonatal encephalopathy following fetal distress. A clinical and electroencephalographic study. Arch Neurol 1976;33:696–705.
Mirro R, Lowery-Smith L, Armstead WM, Shibata M, Zuckerman SL, Leffler CW. Cerebral vasoconstriction in response to hypocapnia is maintained after ischemia/reperfusion injury in newborn pigs. Stroke 1992;23:1613–6.
Bisschops LL, Hoedemaekers CW, Simons KS, van der Hoeven JG. Preserved metabolic coupling and cerebrovascular reactivity during mild hypothermia after cardiac arrest. Crit Care Med 2010;38:1542–7.
Vannucci RC, Towfighi J, Heitjan DF, Brucklacher RM. Carbon dioxide protects the perinatal brain from hypoxic-ischemic damage: an experimental study in the immature rat. Pediatrics 1995;95:868–74.
Vannucci RC, Brucklacher RM, Vannucci SJ. Effect of carbon dioxide on cerebral metabolism during hypoxia-ischemia in the immature rat. Pediatr Res 1997;42:24–9.
Zhou Q, Cao B, Niu L, et al. Effects of permissive hypercapnia on transient global cerebral ischemia-reperfusion injury in rats. Anesthesiology 2010;112:288–97.
Tao T, Zhao M, Yang W, Bo Y, Li W. Neuroprotective effects of therapeutic hypercapnia on spatial memory and sensorimotor impairment via anti-apoptotic mechanisms after focal cerebral ischemia/reperfusion. Neurosci Lett 2014;573:1–6.
Sandroni C, D’Arrigo S. Management of oxygen and carbon dioxide pressure after cardiac arrest. Minerva Anestesiol 2014;80:1105–14.
Kofstad J. Blood gases and hypothermia: some theoretical and practical considerations. Scand J Clin Lab Invest Suppl 1996;224:21–6.
Acknowledgements
We thank the many technicians, nurses, physicians, and scientists in the participant sites who contributed to the development and implementation of the CoolCap Study, and the parents who consented to enrollment of their infants in the trial who trusted in us under conditions of great stress and anxiety. We thank the many charities and research funding agencies who supported the preliminary research necessary for the study. The original study was designed by and was the responsibility of the Scientific Advisory Committee (SAC), who had full access to the trial data, and after reading and editing this manuscript, approved the final draft for submission.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Lingappan, K., Kaiser, J., Srinivasan, C. et al. Relationship between PCO2 and unfavorable outcome in infants with moderate-to-severe hypoxic ischemic encephalopathy. Pediatr Res 80, 204–208 (2016). https://doi.org/10.1038/pr.2016.62
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/pr.2016.62
This article is cited by
-
Neuroprotective therapies in the NICU in term infants: present and future
Pediatric Research (2023)
-
Transcutaneous carbon dioxide monitoring during therapeutic hypothermia for neonatal encephalopathy
Pediatric Research (2022)
-
Carbon dioxide levels in neonates: what are safe parameters?
Pediatric Research (2022)
-
Hypocapnia in early hours of life is associated with brain injury in moderate to severe neonatal encephalopathy
Journal of Perinatology (2022)
-
Non-invasive carbon dioxide monitoring in neonates: methods, benefits, and pitfalls
Journal of Perinatology (2021)