Abstract
Background:
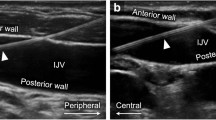
Real-time ultrasound (US) guidance for central venous catheter (CVC) insertion has been shown to increase cannulation success rates and reduce complications in adults. Literature regarding US-guided CVC placement in children remains limited and conflicting. This meta-analysis examines the efficacy and safety of US-guided CVC placement among pediatric patients.
Methods:
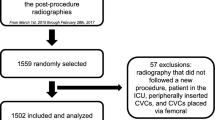
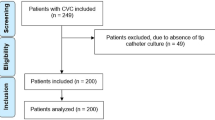
A comprehensive literature search of all published randomized control trials (RCTs) comparing the use of real-time US-guided CVC insertion with anatomic landmark (LM)-guided CVC insertion in pediatric patients <18 y of age was conducted. Outcomes analyzed were cannulation success rate, number of attempts required, incidence of accidental arterial puncture, and time to cannulation.
Results:
Eight RCTs involving 760 patients were analyzed. US-guided CVC insertion significantly increased success rates by 31.8% and decreased the mean number of attempts required. A trend toward a decrease in the risk of accidental arterial puncture with the use of US-guided CVC insertion was also observed. US-guided CVC insertion was not associated with a significant difference in time required for CVC placement.
Conclusion:
US-guided CVC placement is associated with significantly higher success rates and decreased mean number of attempts required for cannulation. US-guided CVC insertion improves success rates, and should be utilized in pediatric patients.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Randolph AG, Cook DJ, Gonzales CA, Pribble CG. Ultrasound guidance for placement of central venous catheters: a meta-analysis of the literature. Crit Care Med 1996;24:2053–8.
Palepu GB, Deven J, Subrahmanyam M, Mohan S. Impact of ultrasonography on central venous catheter insertion in intensive care. Indian J Radiol Imaging 2009;19:191–8.
Troianos CA, Hartman GS, Glas KE, et al.; Councils on Intraoperative Echocardiography and Vascular Ultrasound of the American Society of Echocardiography; Society of Cardiovascular Anesthesiologists. Special articles: guidelines for performing ultrasound guided vascular cannulation: recommendations of the American Society of Echocardiography and the Society Of Cardiovascular Anesthesiologists. Anesth Analg 2012;114:46–72.
McGee DC, Gould MK. Preventing complications of central venous catheterization. N Engl J Med 2003;348:1123–33.
National Institute for Clinical Excellence. Guidance on the use of ultrasound locating devices for placing central venous catheters. Technical Appraisal Guidance, 2002. https://www.nice.org.uk/guidance/ta49.
Grebenik CR, Boyce A, Sinclair ME, Evans RD, Mason DG, Martin B. NICE guidelines for central venous catheterization in children. Is the evidence base sufficient? Br J Anaesth 2004;92:827–30.
Wu SY, Ling Q, Cao LH, Wang J, Xu MX, Zeng WA. Real-time two-dimensional ultrasound guidance for central venous cannulation: a meta-analysis. Anesthesiology 2013;118:361–75.
Lee C, Chamberlain Ronald S. Ultrasound guided central venous catheter insertion: is safer, but in whose hands? A meta-analysis. 10th Annual Academic Surgical Congress 2015. (www.asc-abstracts.org).
Karimi-Sari H, Faraji M, Mohazzab Torabi S, Asjodi G. Success rate and complications of internal jugular vein catheterization with and without ultrasonography guide. Nurs Midwifery Stud 2014;3:e23204.
Aouad MT, Kanazi GE, Abdallah FW, et al. Femoral vein cannulation performed by residents: a comparison between ultrasound-guided and landmark technique in infants and children undergoing cardiac surgery. Anesth Analg 2010;111:724–8.
Bruzoni M, Slater BJ, Wall J, St Peter SD, Dutta S. A prospective randomized trial of ultrasound- vs landmark-guided central venous access in the pediatric population. J Am Coll Surg 2013;216:939–43.
Srisan P, Juhong S, Kanjanapatanakul W. Central venous catheterization related complications in Pediatric Intensive Care Unit at Queen Sirikit National Institute of Child Health. J Med Assoc Thai 2014;97 Suppl 6:S83–8.
Froehlich CD, Rigby MR, Rosenberg ES, et al. Ultrasound-guided central venous catheter placement decreases complications and decreases placement attempts compared with the landmark technique in patients in a pediatric intensive care unit. Crit Care Med 2009;37:1090–6.
Denys BG, Uretsky BF. Anatomical variations of internal jugular vein location: impact on central venous access. Crit Care Med 1991;19:1516–9.
Citak A, Karaböcüoğlu M, Uçsel R, Uzel N. Central venous catheters in pediatric patients–subclavian venous approach as the first choice. Pediatr Int 2002;44:83–6.
Casado-Flores J, Barja J, Martino R, Serrano A, Valdivielso A. Complications of central venous catheterization in critically ill children. Pediatr Crit Care Med 2001;2:57–62.
Mortensen JD, Talbot S, Burkart JA. Cross-sectional internal diameters of human cervical and femoral blood vessels: relationship to subject’s sex, age, body size. Anat Rec 1990;226:115–24.
Hayashi Y, Uchida O, Takaki O, et al. Internal jugular vein catheterization in infants undergoing cardiovascular surgery: an analysis of the factors influencing successful catheterization. Anesth Analg 1992;74:688–93.
Bosman M, Kavanagh RJ. Two dimensional ultrasound guidance in central venous catheter placement; a postal survey of the practice and opinions of consultant pediatric anesthetists in the United Kingdom. Paediatr Anaesth 2006;16:530–7.
Bailey PL, Glance LG, Eaton MP, Parshall B, McIntosh S. A survey of the use of ultrasound during central venous catheterization. Anesth Analg 2007;104:491–7.
McGrattan T, Duffty J, Green JS, O’Donnell N. A survey of the use of ultrasound guidance in internal jugular venous cannulation. Anaesthesia 2008;63:1222–5.
Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996;17:1–12.
Verghese ST, McGill WA, Patel RI, Sell JE, Midgley FM, Ruttimann UE . Ultrasound-guided internal jugular venous cannulation in infants: a prospective comparison with the traditional palpation method. Anesthesiology 1999;91:71–77.
Verghese ST, McGill WA, Patel RI, Sell JE, Midgley FM, Ruttimann UE . Comparison of three techniques for internal jugular vein cannulation in infants. Paediatr Anaesth 2000;10:505–11.
Chuan WX, Wei W, Yu L . A randomized-controlled study of ultrasound prelocation vs anatomical landmark-guided cannulation of the internal jugular vein in infants and children. Paediatr Anaesth 2005;15:733–38.
Ovezov A, Zakirov I, Vishnyakova M . Effectiveness and safety of the internal jugular vein catheterization in pediatrics: ultrasound navigation vs anatomical landmarks (a prospective, randomized, double-blind study). Int Care Med 2010;36:S275.
Author information
Authors and Affiliations
Corresponding author
Supplementary information
Supplementary Material
(DOC 108 kb)
Rights and permissions
About this article
Cite this article
Lau, C., Chamberlain, R. Ultrasound-guided central venous catheter placement increases success rates in pediatric patients: a meta-analysis. Pediatr Res 80, 178–184 (2016). https://doi.org/10.1038/pr.2016.74
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/pr.2016.74
This article is cited by
-
Impact of insertion site on complications in central venous access devices
Pediatric Surgery International (2023)
-
Intraoperative hypothermia in the neonate population: risk factors, outcomes, and typical patterns
Journal of Clinical Monitoring and Computing (2023)
-
Point-of-Care Ultrasound-Guided Procedures in the Pediatric Cardiac Intensive Care Unit
Current Treatment Options in Pediatrics (2022)
-
A randomized controlled trial of ultrasound-assisted technique versus conventional puncture method for saphenous venous cannulations in children with congenital heart disease
BMC Anesthesiology (2021)
-
Performing central venous catheters in neonates and small infants undergoing cardiac surgery using a wireless transducer for ultrasound guidance: a prospective, observational pilot study
BMC Pediatrics (2021)