Abstract
Background:
We evaluated the risk of attention-deficit hyperactivity disorder (ADHD) following childhood traumatic brain injury (TBI).
Methods:
Using Taiwan’s National Health Insurance Research Database, we included 10,416 newly diagnosed TBI children (aged ≤12 y) between 2001 and 2002 and 41,664 children without TBI, who were frequency matched by sex, age, and year of the index medical service with each TBI child, as controls. Children who had been diagnosed with ADHD prior to their medical service index were excluded. Each individual was followed for 9 y to identify ADHD diagnosis. We also compared the ADHD risk in children who were treated for fractures but not TBI as sensitivity analysis.
Results:
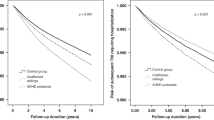
During the 9-y follow-up period, children with TBI had a higher ADHD risk (adjusted hazard ratio (AHR) = 1.32, 95% confidence interval (CI) = 1.19, 1.45) than did those without TBI. Furthermore, children with mild and severe TBI had higher AHRs for ADHD than did those without TBI (AHR = 1.30; 95% CI = 1.10, 1.53; and AHR = 1.37; 95% CI = 1.22, 1.55). However, no significant association was observed between fractures and ADHD.
Conclusion:
TBI in childhood is associated with a greater likelihood of developing ADHD.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Schwartz L, Taylor HG, Drotar D, Yeates KO, Wade SL, Stancin T. Long-term behavior problems following pediatric traumatic brain injury: prevalence, predictors, and correlates. J Pediatr Psychol 2003;28:251–63.
Yeates KO, Armstrong K, Janusz J, et al. Long-term attention problems in children with traumatic brain injury. J Am Acad Child Adolesc Psychiatry 2005;44:574–84.
Roman MJ, Delis DC, Willerman L, et al. Impact of pediatric traumatic brain injury on components of verbal memory. J Clin Exp Neuropsychol 1998;20:245–58.
Barkley RA. Attention-deficit/hyperactivity disorder, self-regulation, and time: toward a more comprehensive theory. J Dev Behav Pediatr 1997;18:271–9.
Fischer M, Barkley RA, Smallish L, Fletcher K. Hyperactive children as young adults: driving abilities, safe driving behavior, and adverse driving outcomes. Accid Anal Prev 2007;39:94–105.
Ramos Olazagasti MA, Klein RG, Mannuzza S, et al. Does childhood attention-deficit/hyperactivity disorder predict risk-taking and medical illnesses in adulthood? J Am Acad Child Adolesc Psychiatry 2013;52:153–162.e4.
Konrad K, Gauggel S, Manz A, Schöll M. Inhibitory control in children with traumatic brain injury (TBI) and children with attention deficit/hyperactivity disorder (ADHD). Brain Inj 2000;14:859–75.
Max JE, Lansing AE, Koele SL, et al. Attention deficit hyperactivity disorder in children and adolescents following traumatic brain injury. Dev Neuropsychol 2004;25:159–77.
Schachar R, Levin HS, Max JE, Purvis K, Chen S. Attention deficit hyperactivity disorder symptoms and response inhibition after closed head injury in children: do preinjury behavior and injury severity predict outcome? Dev Neuropsychol 2004;25:179–98.
Adeyemo BO, Biederman J, Zafonte R, et al. Mild traumatic brain injury and ADHD: a systematic review of the literature and meta-analysis. J Atten Disord 2014;18:576–84.
Andrews PJ, Piper IR, Dearden NM, Miller JD. Secondary insults during intrahospital transport of head-injured patients. Lancet 1990;335:327–30.
Babikian T, Asarnow R. Neurocognitive outcomes and recovery after pediatric TBI: meta-analytic review of the literature. Neuropsychol 2009;23:283–96.
Anderson V, Godfrey C, Rosenfeld JV, Catroppa C. Predictors of cognitive function and recovery 10 years after traumatic brain injury in young children. Pediatr 2012;129:e254–61.
Max JE, Arndt S, Castillo CS, et al. Attention-deficit hyperactivity symptomatology after traumatic brain injury: a prospective study. J Am Acad Child Adolesc Psychiatry 1998;37:841–7.
Max JE, Schachar RJ, Levin HS, et al. Predictors of attention-deficit/hyperactivity disorder within 6 months after pediatric traumatic brain injury. J Am Acad Child Adolesc Psychiatry 2005;44:1032–40.
Slomine BS, Salorio CF, Grados MA, Vasa RA, Christensen JR, Gerring JP. Differences in attention, executive functioning, and memory in children with and without ADHD after severe traumatic brain injury. J Int Neuropsychol Soc 2005;11:645–53.
Wassenberg R, Max JE, Lindgren SD, Schatz A. Sustained attention in children and adolescents after traumatic brain injury: relation to severity of injury, adaptive functioning, ADHD and social background. Brain Inj 2004;18:751–64.
McKinlay A, Grace R, Horwood J, Fergusson D, MacFarlane M. Adolescent psychiatric symptoms following preschool childhood mild traumatic brain injury: evidence from a birth cohort. J Head Trauma Rehabil 2009;24:221–7.
Petersen C, Scherwath A, Fink J, Koch U. Health-related quality of life and psychosocial consequences after mild traumatic brain injury in children and adolescents. Brain Inj 2008;22:215–21.
Massagli TL, Fann JR, Burington BE, Jaffe KM, Katon WJ, Thompson RS. Psychiatric illness after mild traumatic brain injury in children. Arch Phys Med Rehabil 2004;85:1428–34.
Chou IC, Lin CC, Sung FC, Kao CH. Attention-deficit-hyperactivity disorder increases risk of bone fracture: a population-based cohort study. Dev Med Child Neurol 2014;56:1111–6.
Thomas CR, Ayoub M, Rosenberg L, Robert RS, Meyer WJ. Attention deficit hyperactivity disorder & pediatric burn injury: a preliminary retrospective study. Burns 2004;30:221–3.
Allen DN, Leany BD, Thaler NS, Cross C, Sutton GP, Mayfield J. Memory and attention profiles in pediatric traumatic brain injury. Arch Clin Neuropsychol 2010;25:618–33.
Keenan HT, Hall GC, Marshall SW. Early head injury and attention deficit hyperactivity disorder: retrospective cohort study. BMJ 2008;337:a1984.
Glascoe FP. Early detection of developmental and behavioral problems. Pediatr Rev 2000;21:272–9; quiz 280.
Babikian T, Freier MC, Tong KA, et al. Susceptibility weighted imaging: neuropsychologic outcome and pediatric head injury. Pediatr Neurol 2005;33:184–94.
Ylvisaker M, Feeney T. Pediatric brain injury: social, behavioral, and communication disability. Phys Med Rehabil Clin N Am 2007;18:133–44, vii.
Lindström K, Lindblad F, Hjern A. Preterm birth and attention-deficit/hyperactivity disorder in schoolchildren. Pediatr 2011;127:858–65.
Halmøy A, Klungsøyr K, Skjærven R, Haavik J. Pre- and perinatal risk factors in adults with attention-deficit/hyperactivity disorder. Biol Psychiatry 2012;71:474–81.
Robison LM, Sclar DA, Skaer TL, Galin RS. Treatment modalities among US children diagnosed with attention-deficit hyperactivity disorder: 1995-99. Int Clin Psychopharmacol 2004;19:17–22.
Dunn DW, Austin JK, Harezlak J, Ambrosius WT. ADHD and epilepsy in childhood. Dev Med Child Neurol 2003;45:50–4.
Shank LK, Kaufman J, Leffard S, Warschausky S. Inspection time and attention-deficit/hyperactivity disorder symptoms in children with cerebral palsy. Rehabil Psychol 2010;55:188–93.
Bazarian JJ, Veazie P, Mookerjee S, Lerner EB. Accuracy of mild traumatic brain injury case ascertainment using ICD-9 codes. Acad Emerg Med 2006;13:31–8.
Yeh CC, Chen TL, Hu CJ, Chiu WT, Liao CC. Risk of epilepsy after traumatic brain injury: a retrospective population-based cohort study. J Neurol Neurosurg Psychiatry 2013;84:441–5.
Chen MH, Chen YS, Hsu JW, et al. Comorbidity of ADHD and subsequent bipolar disorder among adolescents and young adults with major depression: a nationwide longitudinal study. Bipolar Disord 2015;17:315–22.
Chou PH, Lin CC, Lin CH, Loh el-W, Chan CH, Lan TH. Prevalence of allergic rhinitis in patients with attention-deficit/hyperactivity disorder: a population-based study. Eur Child Adolesc Psychiatry 2013;22:301–7.
Shyu CS, Lin HK, Lin CH, Fu LS. Prevalence of attention-deficit/hyperactivity disorder in patients with pediatric allergic disorders: a nationwide, population-based study. J Microbiol Immunol Infect 2012;45:237–42.
Acknowledgements
The dataset was obtained from the National Health Insurance Research Database provided by the Bureau of National Health Insurance, Department of Health, Taiwan, and managed by the National Health Research Institutes. The interpretations and conclusions contained herein do not represent those of the Bureau of National Health Insurance, Department of Health, or the National Health Research Institutes.
Author information
Authors and Affiliations
Corresponding author
Supplementary information
Supplementary Figure
(TIFF 2038 kb)
Supplementary Tables
(DOC 77 kb)
PowerPoint slides
Rights and permissions
About this article
Cite this article
Yang, LY., Huang, CC., Chiu, WT. et al. Association of traumatic brain injury in childhood and attention-deficit/hyperactivity disorder: a population-based study. Pediatr Res 80, 356–362 (2016). https://doi.org/10.1038/pr.2016.85
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/pr.2016.85