Abstract
Background
Premature infants may lack mature cerebrovascular autoregulatory function and fail to adapt oxygen extraction to decreasing systemic perfusion.
Methods
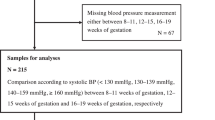
Infants ≤28 weeks of gestational age (GA) were recruited. Systemic oxygen saturation (SpO2), mean arterial blood pressure (MABP), and cerebral saturation (near-infrared spectroscopy, SctO2) were measured continuously over the first 72 h. Resulting data underwent error-processing. For each remaining 10 m window, the mean MABP and fractional tissue oxygen extraction (FTOE) were calculated. The infants were divided into two groups (23–25 and 26–28 weeks). The median FTOE at low, medium, and high MABP values (empirically defined within each group based on the 25th and 75th centile) were compared between estimated gestational age (EGA) groups.
Results
Sample n=68, mean±SD GA=25.5±1.3 weeks, and birthweight (BW)=823±195 g. The median FTOE in the more preterm group vs. more mature group was statistically different at lower value of MABP (P<0.01) and higher values of MABP (P=0.01), but not at medium values (P=0.55).
Conclusion
The more mature group (GA 26–28 weeks) displayed an appropriate increase in oxygen extraction during hypotension, steadily decreasing as MABP increased, suggesting mature autoregulation. An opposite response was noted in the more preterm group, suggesting an inability to mount a compensatory response when BP is outside of the physiologic range.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Chong SP, Merkle CW, Leahy C, Srinivasan VJ . Cerebral metabolic rate of oxygen (CMRO_2) assessed by combined Doppler and spectroscopic OCT. Biomed Opt Express 2015;6:3941.
St. Peter D, Gandy C, Hoffman SB . Hypotension and adverse outcomes in prematurity: comparing definitions. Neonatology 2017;111:228–33.
Miall-Allen VM, de Vries LS, Dubowitz LM, Whitelaw AG . Blood pressure fluctuation and intraventricular hemorrhage in the preterm infant of less than 31 weeks’ gestation. Pediatrics 1989;83:657–61.
Wilson-Costello D, Friedman H, Minich N, Fanaroff AA, Hack M . Improved survival rates with increased neurodevelopmental disability for extremely low birth weight infants in the 1990s. Pediatrics 2005;115:997–1003.
Mukerji A, Shah V, Shah PS . Periventricular/intraventricular hemorrhage and neurodevelopmental outcomes: a meta-analysis. Pediatrics 2015;136:1132–43.
Stoll BJ, Hansen NI, Bell EF et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics 2010;126:443–56.
Soul JS, Hammer PE, Tsuji M et al. Fluctuating pressure-passivity is common in the cerebral circulation of sick premature infants. Pediatr Res 2007;61:467–73.
Miall-Allen VM, de Vries LS, Whitelaw AG . Mean arterial blood pressure and neonatal cerebral lesions. Arch Dis Child 1987;62:1068–9.
Clark CE, Clyman RI, Roth RS, Sniderman SH, Lane B, Ballard RA . Risk factor analysis of intraventricular hemorrhagein low-birth-weight infants. J Pediatr 1981;99:625–8.
Goldberg RN, Chung D, Goldman SL, Bancalari E . The association of rapid volume expansion and intraventricular hemorrhage in the preterm infant. J Pediatr 1980;96:1060–3.
Köksal N, Baytan B, Bayram Y, Nacarküçük E . Risk factors for intraventricular haemorrhage in very low birth weight infants. Indian J Pediatr 2002;69:561–4.
Volpe JJ. Volpe JJ. Neurology of the Newborn. 5th edn, Philadelphia, PA, USA: Saunders/Elsevier, 2008.
Vesoulis ZA, Liao SM, Trivedi SB, Ters NE, Mathur AM . A novel method for assessing cerebral autoregulation in preterm infants using transfer function analysis. Pediatr Res 2016;79:453–9.
Bajwa N, Berner M, Worley S, Pfister R . Population based age stratified morbidities of premature infants in Switzerland. Swiss Med Wkly 2011;141:w13212.
Tioseco JA, Aly H, Essers J, Patel K, El-Mohandes AAE . Male sex and intraventricular hemorrhage. Pediatr Crit Care Med 2006;7:40–44.
Cipolla MJ. The Cerebral Circulation. San Rafael, CA: Morgan & Claypool Life Sciences, 2009.
Goadsby PJ. Autonomic nervous system control of the cerebral circulation. In: Robert FS, Karam M, Rami OA, eds. Handbook of Clinical Neurology. Elsevier, Amsterdam, The Netherlands, 2013, pp 193–201.
Paulson OB, Strandgaard S, Edvinsson L . Cerebral autoregulation. Cerebrovasc Brain Metab Rev 1990;2:161–92.
Parry G, Tucker J, Tarnow-Mordi W . CRIB II an update of the clinical risk index for babies score. Lancet 2003;361:1789–91.
Papile LA, Burstein J, Burstein R, Koffler H . Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr 1978;92:529–34.
Ayaz H, Izzetoglu M, Shewokis PA, Onaral B . Sliding-window motion artifact rejection for functional near-infrared spectroscopy. Conf Proc IEEE Eng Med Biol Soc 2010;2010:6567–70.
Alderliesten T, Dix L, Baerts W et al. Reference values of regional cerebral oxygen saturation during the first 3 days of life in preterm neonates. Pediatr Res 2015;79:55–64.
Vesoulis ZA, El Ters NM, Wallendorf M, Mathur AM . Empirical estimation of the normative blood pressure in infants <28 weeks gestation using a massive data approach. J Perinatol 2016;36:291–5.
Kent AL, Meskell S, Falk MC, Shadbolt B . Normative blood pressure data in non-ventilated premature neonates from 28-36 weeks gestation. Pediatr Nephrol 2009;24:141–6.
van de Bor M, Walther FJ . Cerebral blood flow velocity regulation in preterm infants. Biol Neonate 1991;59:329–35.
Greisen G . Autoregulation of cerebral blood flow in newborn babies. Early Hum Dev 2005;81:423–8.
Munro MJ, Walker AM, Barfield CP . Hypotensive extremely low birth weight infants have reduced cerebral blood flow. Pediatrics 2004;114:1591–6.
Ramaekers VT, Casaer P, Daniels H, Marchal G . Upper limits of brain blood flow autoregulation in stable infants of various conceptional age. Early Hum Dev 1990;24:249–58.
Tyszczuk L, Meek J, Elwell C, Wyatt JS . Cerebral blood flow is independent of mean arterial blood pressure in preterm infants undergoing intensive care. Pediatrics 1998;102:337–41.
Vavilala MS, Soriano SG. Anesthesia for neurosurgery. In: Peter JD, Franklyn PC, Etsuro KM, eds. Smith’s Anesthesia for Infants and Children. Elsevier, Amsterdam, The Netherland, 2011:713–44.
Mandalà M, Pedatella AL, Morales Palomares S, Cipolla MJ, Osol G . Maturation is associated with changes in rat cerebral artery structure, biomechanical properties and tone. Acta Physiol 2012;205:363–71.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Statement of Financial Support
This work was supported by the following grants: Washington University Institute of Clinical and Translational Sciences KL2 Training Program (NIH/NCATS KL2 TR000450) and The Barnes-Jewish Hospital Foundation and the Washington University Institute of Clinical and Translational Sciences Clinical and Translational Funding Program (NIH/NCATS UL1 TR000448).
Rights and permissions
About this article
Cite this article
Vesoulis, Z., Liao, S. & Mathur, A. Gestational age-dependent relationship between cerebral oxygen extraction and blood pressure. Pediatr Res 82, 934–939 (2017). https://doi.org/10.1038/pr.2017.196
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/pr.2017.196
This article is cited by
-
Early arterial pressure monitoring and term-equivalent age MRI findings in very preterm infants
Pediatric Research (2022)
-
Changes in cerebral tissue oxygenation and fractional oxygen extraction with gestational age and postnatal maturation in preterm infants
Journal of Perinatology (2021)
-
Regional tissue oxygenation monitoring in the neonatal intensive care unit: evidence for clinical strategies and future directions
Pediatric Research (2019)