Abstract
Background
Necrotizing enterocolitis (NEC) is a devastating neonatal disease characterized by intestinal necrosis. Hypoxia-inducible factor-1α (HIF-1α) has a critical role in cellular oxygen homeostasis. Here, we hypothesized that prolyl hydroxylase (PHD) inhibition, which stabilizes HIF-1α, protects against NEC by promoting intestinal endothelial cell proliferation and improving intestinal microvascular integrity via vascular endothelial growth factor (VEGF) signaling.
Methods
To assess the role of PHD inhibition in a neonatal mouse NEC model, we administered dimethyloxalylglycine (DMOG) or vehicle to pups before or during the NEC protocol, and determined mortality and incidence of severe intestinal injury. We assessed intestinal VEGF by western blot analysis and quantified endothelial cell and epithelial cell proliferation following immunofluorescence.
Results
DMOG decreased mortality and incidence of severe NEC, increased intestinal VEGF expression, and increased intestinal villus endothelial and epithelial cell proliferation in experimental NEC. Inhibiting VEGFR2 signaling eliminated DMOG’s protective effect on intestinal injury severity, survival, and endothelial cell proliferation while sparing DMOG’s protective effect on intestinal epithelial cell proliferation.
Conclusion
DMOG upregulates intestinal VEGF, promotes endothelial cell proliferation, and protects against intestinal injury and mortality in experimental NEC in a VEGFR2 dependent manner. DMOG’s protective effect on the neonatal intestinal mucosa may be mediated via VEGFR2 dependent improvement of the intestinal microvasculature.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Hopkins GB, Gould VE, Stevenson JK, Oliver TK Jr . Necrotizing enterocolitis in premature infants. A clinical and pathological evaluation of autopsy material. Am J Dis Child 1970;120:229–32.
De Plaen IG . Inflammatory signaling in necrotizing enterocolitis. Clin Perinatol 2013;40:109–24.
Lin PW, Nasr TR, Stoll BJ . Necrotising enterocolitis: recent scientific advances in pathophysiology and prevention. Semin Perinatol 2008;32:70–82.
Lin PW, Stoll BJ . Necrotizing enterocolitis. Lancet 2006;368:1271–83.
Caplan MS. Neonatal necrotizing enterocolitis: clinical observations, pathophysiology, and prevention. In: Martin RJ, Fanaroff AA, Walsh MC, eds. Fanaroff and Martin’s Neonatal-Perinatal Medicine. 9th edn. St Louis, MO: Elsevier, 2011:1431-42.
Sabnis A, Carrasco R, Liu SXL et al. Intestinal vascular endothelial growth factor is decreased in necrotizing enterocolitis. Neonatology 2015;107:191–8.
Yan X, Managlia E, Liu SXL et al. Lack of VEGFR2 signaling causes maldevelopment of the intestinal microvasculature and facilitates necrotizing enterocolitis in neonatal mice. Am J Physiol Gastrointest Liver Physiol 2016;310:G716–25.
Shah YM . The role of hypoxia in intestinal inflammation. Mol Cell Pediatr 2016;3:1.
Lee JW, Bae SH, Jeong JW, Kim SH, Kim KW . Hypoxia-inducible factor (HIF-1)alpha: its protein stability and biological functions. Exp Mol Med 2004;36:1–12.
Avraham-Davidi I, Yona S, Grunewald M et al. On-site education of VEGF-recruited monocytes improves their performance as angiogenic and arteriogenic accessory cells. J Exp Med 2013;210:2611–25.
Grunewald M, Avraham I, Dor Y et al. VEGF-induced adult neovascularization: recruitment, retention, and role of accessory cells. Cell 2006;124:175–89.
Colgan SP, Taylor CT . Hypoxia: an alarm signal during intestinal inflammation. Nat Rev Gastroenterol Hepatol 2010;7:281–7.
Schofield CJ, Ratcliffe PJ . Oxygen sensing by HIF hydroxylases. Nat Rev Mol Cell Biol 2004;5:343–54.
Baregamian N, Rychahou PG, Hawkins HK, Evers BM, Chung DH . Phosphatidylinositol 3-kinase pathway regulates hypoxia-inducible factor-1 to protect from intestinal injury during necrotizing enterocolitis. Surgery 2007;142:295–302.
Jaakkola P, Mole DR, Tian YM et al. Targeting of HIF-alpha to the von Hippel-Lindau ubiquitylation complex by O2-regulated prolyl hydroxylation. Science 2001;292:468–72.
Tian R, Liu SXL, Williams C et al. Characterization of a necrotizing enterocolitis model in newborn mice. Int J Clin Exp Med 2010;3:293–302.
Kubo K, Shimizu T, Ohyama S et al. Novel potent orally active selective VEGFR-2 tyrosine kinase inhibitors: synthesis, structure-activity relationships, and antitumor activities of N-phenyl-N=-{4-(4-quinolyloxy)phenyl} ureas. J Med Chem 2005;48:1359–66.
Nagel S, Papdakis M, Chen R et al. Neuroprotection by dimethyloxalylglycine following permanent and transient focal cerebral ischemia in rats. J Cereb Blood Flow Metab 2011;31:132–43.
Poynter JA, Manukyan MC, Wang Y et al. Systemic pretreatment with dimethyloxalylglycine increases myocardial HIF-1 alpha and VEGF production and improves functional recovery after acute ischemia/reperfusion. Surgery 2011;150:278–83.
Sisk PM, Lovelady CA, Dillard RG, Gruber KJ, O'Shea TM . Early human milk feeding is associated with a lower risk of necrotizing enterocolitis in very low birth weight infants. J Perinatol 2007;27:428–33.
Meinzen-Derr J, Poindexter B, Wrage L et al. Role of human milk in extremely low birth weight infants' risk of necrotizing enterocolitis or death. J Perinatol 2009;29:57–62.
Bauer CR, Morrison JC, Poole WK et al. A decreased incidence of necrotizing enterocolitis after prenatal glucocorticoid therapy. Pediatrics 1984;73:682–8.
Patel RM, Knezevic A, Shenvi N et al. Association of red blood cell transfusion, anemia, and necrotizing enterocolitis in very low-birth-weight infants. JAMA 2016;315:889.
Nowicki PT . Effects of sustained flow reduction on postnatal intestinal circulation. Am J Physiol 1998;275:G758–68.
Nankervis CA, Reber KM, Nowicki PT . Age-dependent changes in the postnatal intestinal microcirculation. Microcirculation 2001;8:377–87.
The BOOST II United Kingdom, Australia, and New Zealand Collaborative Groups. Oxygen saturation and outcomes in preterm infants. N Engl J Med 2013;368:2094–104.
Park AM, Sanders TA, Maltepe E . Hypoxia-inducible factor (HIF) and HIF-stabilization agents in neonatal care. Semin Fetal Neonatal Med 2010;15:196–202.
Gogat K, Le Gat L, Van Den Berghe L et al. VEGF and KDR gene expression during human embryonic and fetal eye development. Invest Ophthalmol Vis Sci 2004;45:7–14.
Gerber HP, Hillan KJ, Ryan AM et al. VEGF is required for growth and survival in neonatal mice. Development 1999;126:1149–59.
Feinman R, Deitch EA, Watkins AC et al. HIF-1 mediates pathogenic inflammatory responses to intestinal ischemia-reperfusion injury. Am J Physiol Gastrointest Liver Physiol 2010;299:G833–43.
Chan MC, Holt-Martyn JP, Schofield CJ et al. Pharmacological targeting of the HIF hydroxylases – a new field in medicine development. Mol Aspects Med 2016;47-48:54–75.
Elzschig H, Bratton DL, Colgan SP . Targeting hypoxia signaling for the treatment of ischaemic and inflammatory diseases. Nat Rev Drug Discov 2014;13:852–69.
Clambey ET, McNamee EN, Westrich JA et al. Hypoxia-inducible factor-1 alpha-dependent induction of FoxP3 drives regulatory T-cell abundance and function during inflammatory hypoxia of the mucosa. Proc Natl Acad Sci USA 2012;109:E2784–93.
Eltzschig HK, Carmeliet P . Hypoxia and inflammation. N Engl J Med 2011;364:656–665.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Statement of Financial Support
This study was supported by funding from Friend of Prentice (FOP) and National Institutes of Health grant R01HD060876 (I.D.P.), RO1DK064240, and RO1GM117628 (X.D.T.). Also, the study was supported in part by the Stanley Manne Children's Research Institute and the Ann & Robert H. Lurie Children's Hospital of Chicago.
Rights and permissions
About this article
Cite this article
Bowker, R., Yan, X., Managlia, E. et al. Dimethyloxalylglycine preserves the intestinal microvasculature and protects against intestinal injury in a neonatal mouse NEC model: role of VEGF signaling. Pediatr Res 83, 545–553 (2018). https://doi.org/10.1038/pr.2017.219
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/pr.2017.219
This article is cited by
-
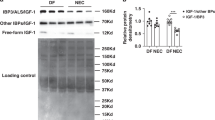
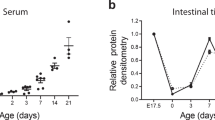
Recombinant IGF-1/BP3 protects against intestinal injury in a neonatal mouse NEC model
Pediatric Research (2024)
-
Necrotizing enterocolitis: recent advances in treatment with translational potential
Pediatric Surgery International (2023)
-
Advances in our understanding of the molecular pathogenesis of necrotizing enterocolitis
BMC Pediatrics (2022)
-
Macrophage-derived IGF-1 protects the neonatal intestine against necrotizing enterocolitis by promoting microvascular development
Communications Biology (2022)
-
Hope on the horizon: promising novel therapies for necrotizing enterocolitis
Pediatric Research (2020)