Abstract
Background
Vagus nerve stimulation (VNS) is an Food and Drug Administration-approved method delivering electrical impulses for treatment of depression and epilepsy in adults. The vagus nerve innervates the majority of visceral organs and cervix, but potential impacts of VNS on the progress of pregnancy and the fetus are not well studied.
Methods
We tested the hypothesis that VNS in pregnant dams does not induce inflammatory changes in the cardio-respiratory control regions of the pups’ brainstem, potentially impacting the morbidity and mortality of offspring. Pregnant dams were implanted with stimulators providing intermittent low or high frequency electrical stimulation of the sub-diaphragmatic esophageal segment of the vagus nerve for 6–7 days until delivery. After birth, we collected pup brainstems that included cardio-respiratory control regions and counted the cells labeled for pro-inflammatory cytokines (interleukin (IL)-1β, IL-6, tumor necrosis factor-α) and high mobility group box 1.
Results
Neither pup viability nor number of cells labeled for pro-inflammatory cytokines in nucleus tractus solitarii or hypoglossal motor nucleus was impaired by VNS. We provide evidence suggesting that chronic VNS of pregnant mothers does not impede the progress or outcome of pregnancy.
Conclusion
VNS does not cause preterm birth, affect well-being of progeny, or impact central inflammatory processes that are critical for normal cardiovascular and respiratory function in newborns.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Chakravarthy K, Chaudhry H, Williams K, Christo PJ . Review of the uses of vagal nerve stimulation in chronic pain management. Curr Pain Headache Rep 2015;19:54.
Meneses G, Bautista M, Florentino A et al. Electric stimulation of the vagus nerve reduced mouse neuroinflammation induced by lipopolysaccharide. J Inflamm Lond Engl 2016;13:33.
Mihaylova S, Killian A, Mayer K, Pullamsetti SS, Schermuly R, Rosengarten B . Effects of anti-inflammatory vagus nerve stimulation on the cerebral microcirculation in endotoxinemic rats. J Neuroinflammation 2012;9:183.
Tracey KJ . The inflammatory reflex. Nature 2002;420:853–859.
Borovikova LV, Ivanova S, Zhang M et al. Vagus nerve stimulation attenuates the systemic inflammatory response to endotoxin. Nature 2000;405:458–462.
Husain MM, Stegman D, Trevino K . Pregnancy and delivery while receiving vagus nerve stimulation for the treatment of major depression: a case report. Ann Gen Psychiatry 2005;4:16.
Ben-Menachem E . Vagus nerve stimulation for treatment of seizures? Arch Neurol 1998;55:231–232.
Collins JJ, Lin CE, Berthoud HR, Papka RE . Vagal afferents from the uterus and cervix provide direct connections to the brainstem. Cell Tissue Res 1999;295:43–54.
Groves DA, Brown VJ . Vagal nerve stimulation: a review of its applications and potential mechanisms that mediate its clinical effects. Neurosci Biobehav Rev 2005;29:493–500.
Yellon SM . Contributions to the dynamics of cervix remodeling prior to term and preterm birth. Biol Reprod 2017;96:13–23.
Kirby LS, Kirby MA, Warren JW, Tran LT, Yellon SM . Increased innervation and ripening of the prepartum murine cervix. J Soc Gynecol Investig 2005;12:578–585.
Clyde LA, Lechuga TJ, Ebner CA, Burns AE, Kirby MA, Yellon SM . Transection of the pelvic or vagus nerve forestalls ripening of the cervix and delays birth in rats. Biol Reprod 2011;84:587–594.
Kallapur SG, Nitsos I, Moss TJM et al. IL-1 mediates pulmonary and systemic inflammatory responses to chorioamnionitis induced by lipopolysaccharide. Am J Respir Crit Care Med 2009;179:955–961.
Chau V, McFadden DE, Poskitt KJ, Miller SP . Chorioamnionitis in the pathogenesis of brain injury in preterm infants. Clin Perinatol 2014;41:83–103.
Perlman JM . White matter injury in the preterm infant: an important determination of abnormal neurodevelopment outcome. Early Hum Dev 1998;53:99–120.
Burd I, Balakrishnan B, Kannan S . Models of fetal brain injury, intrauterine inflammation, and preterm birth. Am J Reprod Immunol 2012;67:287–294.
Sanders TR, Kim DW, Glendining KA, Jasoni CL . Maternal obesity and IL-6 lead to aberrant developmental gene expression and deregulated neurite growth in the fetal arcuate nucleus. Endocrinology 2014;155:2566–2577.
Duncan JR, Cock ML, Scheerlinck J-PY et al. White matter injury after repeated endotoxin exposure in the preterm ovine fetus. Pediatr Res 2002;52:941–949.
Balan KV, Kc P, Mayer CA, Wilson CG, Belkadi A, Martin RJ . Intrapulmonary lipopolysaccharide exposure upregulates cytokine expression in the neonatal brainstem. Acta Paediatr 2012;101:466–471.
Jafri A, Belkadi A, Zaidi SIA, Getsy P, Wilson CG, Martin RJ . Lung inflammation induces IL-1β expression in hypoglossal neurons in rat brainstem. Respir Physiol Neurobiol 2013;188:21–28.
Patel YA, Butera RJ . Differential fiber-specific block of nerve conduction in mammalian peripheral nerves using kilohertz electrical stimulation. J Neurophysiol 2015;113:3923–3929.
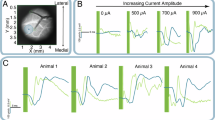
Johnson RL, Murray ST, Camacho DK, Wilson CG . Vagal nerve stimulation attenuates IL-6 and TNFα expression in respiratory regions of the developing rat brainstem. Respir Physiol Neurobiol 2016;229:1–4.
Antonelli MC, ed. Perinatal Programming of Neurodevelopment, 1st edn, 2015 edition. Springer Springer-Verlag, New York, NY, 2016.
Houser MV, Hennessy MD, Howard BC . Vagal nerve stimulator use during pregnancy for treatment of refractory seizure disorder. Obstet Gynecol 2010;115:417–419.
Fang D, Shi S-Q, Shi L et al. Direct electrical stimulation softens the cervix in pregnant and nonpregnant rats. Am J Obstet Gynecol 2015;212:786.e1–786.e9.
Patel YA, Saxena T, Bellamkonda RV, Butera RJ . Kilohertz frequency nerve block enhances anti-inflammatory effects of vagus nerve stimulation. Sci Rep 2017;7:39810.
Levy G, Fishman JE, Xu D et al. Vagal nerve stimulation modulates gut injury and lung permeability in trauma-hemorrhagic shock. J Trauma Acute Care Surg 2012;73:338–342 discussion 342.
Bajbouj M, Merkl A, Schlaepfer TE et al. Two-year outcome of vagus nerve stimulation in treatment-resistant depression. J Clin Psychopharmacol 2010;30:273–281.
Martin RJ, Wilson CG . What to do about apnea of prematurity? J Appl Physiol 2009;107:1015–1016.
Moorman JR, Lake DE, Ivanov PC . Early detection of sepsis—a role for network physiology? Crit Care Med 2016;44:e312–e313.
Doyle SL, O’Neill LAJ . Toll-like receptors: from the discovery of NFkappaB to new insights into transcriptional regulations in innate immunity. Biochem Pharmacol 2006;72:1102–1113.
Reys LG, Ortiz-Pomales YT, Lopez N et al. Uncovering the neuroenteric-pulmonary axis: vagal nerve stimulation prevents acute lung injury following hemorrhagic shock. Life Sci 2013;92:783–792.
Balan KV, Kc P, Hoxha Z, Mayer CA, Wilson CG, Martin RJ . Vagal afferents modulate cytokine-mediated respiratory control at the neonatal medulla oblongata. Respir Physiol Neurobiol 2011;178:458–464.
Drexler SK, Foxwell BM . The role of toll-like receptors in chronic inflammation. Int J Biochem Cell Biol 2010;42:506–518.
Santello M, Bezzi P, Volterra A . TNF$\alpha$ controls glutamatergic gliotransmission in the hippocampal dentate gyrus. Neuron 2011;69:988–1001.
Kiss A, Tratsiakovich Y, Mahdi A et al. Vagal nerve stimulation reduces infarct size via a mechanism involving the alpha-7 nicotinic acetylcholine receptor and downregulation of cardiac and vascular arginase. Acta Physiol 2017;221:174–181.
Andersson U, Antoine DJ, Tracey KJ . The functions of HMGB1 depend on molecular localization and post-translational modifications. J Intern Med 2014;276:420–424.
Tanner JA . Reversible blocking of nerve conduction by alternating-current excitation. Nature 1962;195:712–713.
Kilgore KL, Bhadra N . Reversible nerve conduction block using kilohertz frequency alternating current. Neuromodulation J 2014;17:242–254 discussion 254–255.
Bowman BR, McNeal DR . Response of single alpha motoneurons to high-frequency pulse trains. Firing behavior and conduction block phenomenon. Appl Neurophysiol 1986;49:121–138.
Klune JR, Dhupar R, Cardinal J, Billiar TR, Tsung A . HMGB1: endogenous danger signaling. Mol Med 2008;14:476–484.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Statement of Financial support
This work was supported in part by NIH HD954931. Imaging was performed in the Advanced Imaging and Microscopy Core with support from NSF Grant MRI-DBI 0923559 and the Loma Linda University School of Medicine Pediatrics Research Fund.
Rights and permissions
About this article
Cite this article
Judkins, A., Johnson, R., Murray, S. et al. Vagus nerve stimulation in pregnant rats and effects on inflammatory markers in the brainstem of neonates. Pediatr Res 83, 514–519 (2018). https://doi.org/10.1038/pr.2017.265
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/pr.2017.265
This article is cited by
-
Neuromodulation for Headache Management in Pregnancy
Current Pain and Headache Reports (2025)
-
Pregnancy Outcomes in Epilepsy Patients Treated with Neuromodulating Devices
Current Neurology and Neuroscience Reports (2025)
-
Vagus nerve stimulation ameliorates L-NAME-induced preeclampsia-like symptoms in rats through inhibition of the inflammatory response
BMC Pregnancy and Childbirth (2021)
-
Unique Populations with Episodic Migraine: Pregnant and Lactating Women
Current Pain and Headache Reports (2018)