Abstract
Background
To evaluate a whole-body rapid imaging technique to calculate neonatal lean body mass and percentage adiposity using 3.0 Tesla chemical shift magnetic resonance imaging (MRI).
Methods
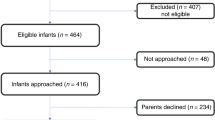
A 2-Point Dixon MRI technique was used to calculate whole-body fat and water images in term (n=10) and preterm (n=15) infants.
Results
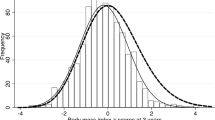
Chemical shift images were obtained in 42 s. MRI calculated whole-body mass correlated closely with measured body weight (R2=0.87; P<0.001). Scan–rescan analysis demonstrated a 95% limit of agreement of 1.3% adiposity. Preterm infants were born at a median of 25.7 weeks’ gestation with birth weight 840 g. At term-corrected age, former preterm infants were lighter than term-born controls, 2,519 vs. 3,094 g regressing out age and group as covariates (P=0.005). However, this was not because of reduced percentage adiposity 26% vs. 24% (P=0.28). At term-corrected age, former preterm infants had significantly reduced lean body mass compared with that of term-born controls 1,935 vs. 2,416 g (P=0.002).
Conclusion
Rapid whole-body imaging for assessment of lean body mass and adiposity in term and preterm infants is feasible, accurate, and repeatable. Deficits in whole-body mass in former preterm infants at term-corrected age are due to reductions in lean body mass not due to differences in adiposity.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Hsiao CC, Tsai ML, Chen CC, Lin HC . Early optimal nutrition improves neurodevelopmental outcomes for very preterm infants. Nutr Rev 2014;72:532–40.
Schneider N, Garcia-Rodenas CL . Early nutritional interventions for brain and cognitive development in preterm Infants: a review of the literature. Nutrients 2017;9:1–20.
Johnson MJ, Wootton SA, Leaf AA, Jackson AA . Preterm birth and body composition at term equivalent age: a systematic review and meta-analysis. Pediatrics 2012;130:640–9.
Daly-Wolfe KM, Jordan KC, Slater H, Beachy JC, Moyer-Mileur LJ . Mid-arm circumference is a reliable method to estimate adiposity in preterm and term infants. Pediatr Res 2015;78:336–41.
Rice MS, Valentine CJ . Neonatal body composition: measuring lean mass as a tool to guide nutrition management in the neonate. Nutr Clin Pract 2015;30:625–32.
McLeod G, Simmer K, Sherriff J, Nathan E, Geddes D, Hartmann P . Feasibility study: Assessing the influence of macronutrientintakes on preterm body composition, using air displacement plethysmography. J Ped Child Health 2015;51:862–9.
Rigo J, Nyamugabo K, Picuad JC, Gerard P, Pieltain C, De Curtis M . Reference values of body composition obtained by dual energy X-ray absorptometry in preterm and term neonates. J Pediatr Gastroenterol Nutr 1998;27:184–90.
Wrottesley SV, Pisa PT, Micklesfield LK, Pettifor JM, Norris SA . A comparison of body composition estimates using dual-energy X-ray absorptiometry and air-displacement plethysmography in South African neonates. Eur J Clin Nutr 2016;70:1254–8.
Dixon WT . Simple proton spectroscopic imaging. Radiology 1984;153:189–94.
Yeung HN, Kormos DW . Separation of true fat and water images by correcting magnetic field inhomogeneity in situ. Radiology 1986;159:783–6.
Glover GH, Schneider E . Three-point Dixon technique for true water/fat decomposition with B0 inhomogeneity correction. Magn Reson Med 1991;18:371–83.
Groves AM, Chiesa G, Durighel G et al. Functional cardiac MRI in preterm and term newborns. Arch Dis Child Fetal Neonatal Ed 2011;96:86–91.
International Electrotechnical Commission Medical electrical equipment – part 2-33: particular requirements for the basic safety and essential performance of magnetic resonance equipment for medical diagnosis. IEC 60601-2-33:2010. 3.2, 2015-06.
Malik SJ, Beqiri A, Price AN, Teixeira JN, Hand JW, Hajnal JV . Specific absorption rate in neonates undergoing magnetic resonance procedures at 1.5T and 3T. NMR Biomed 2015;28:344–52.
Ward SR, Lieber RL . Density and hydration of fresh and fixed human skeletal muscle. J Biomech 2005;38:2317–2320.
Martin AD, Daniel MZ, Drinkwater DT, Clarys JP . Adipose tissue density, estimated adipose lipid fraction and whole body adiposity in male cadavers. Int J Obes Relat Metab Disord 1994;18:79–83.
Ma J . Breath-hold water and fat imaging using a dual-echo two-point dixon technique with an efficient and robust phase-correction algorithm. Magn Reson Med 2004;52:415–9.
Harrington TA, Thomas EL, Frost G, Modi N, Bell JD . Distribution of adipose tissue in the newborn. Ped Res 2004;55:437–41.
Thomas EL, Saeed N, Hajnal JV et al. Magnetic resonance imaging of total body fat. J Appl Physiol 1998;85:1778–85.
Ludwig UA, Klausmann F, Baumann S et al. Whole-body MRI-based fat quantification: a comparison to air displacement plethysmography. J Magn Reson Imaging 2014;40:1437–44.
Bauer JS, Noel PB, Vollhardt C et al. Accuracy and reproducibility of adipose tissue measurements in young infants by whole body magnetic resonance imaging. PLoS ONE 2015;10:1371.
Roggero P, Giannì ML, Amato O et al. Is term newborn body composition being achieved postnatally in preterm infants? Early Hum Dev 2009;85:349–52.
Roggero P, Giannì ML, Amato O et al. Evaluation of air-displacement plethysmography for body composition assessment in preterm infants. Pediatr Res 2012;72:316–20.
Uthaya S, Bell J, Modi N . Adipose tissue magnetic resonance imaging in the newborn. Horm Res 2004;62 (Suppl 3): 143–8.
Olhager E, Flinke E, Hannerstad U, Forsum E . Studies on human body composition during the first 4 months of life using magnetic resonance imaging and isotope dilution. Pediatr Res 2003;54:906–12.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
STATEMENT OF FINANCIAL SUPPORT
No financial assistance was received in support of this study.
Supplementary information
Rights and permissions
About this article
Cite this article
Dyke, J., Garfinkel, A., Groves, A. et al. High-resolution rapid neonatal whole-body composition using 3.0 Tesla chemical shift magnetic resonance imaging. Pediatr Res 83, 638–644 (2018). https://doi.org/10.1038/pr.2017.294
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/pr.2017.294
This article is cited by
-
Body composition in preterm infants: a systematic review on measurement methods
Pediatric Research (2023)
-
Assessment of lung ventilation of premature infants with bronchopulmonary dysplasia at 1.5 Tesla using phase-resolved functional lung magnetic resonance imaging
Pediatric Radiology (2023)
-
Body composition measurement for the preterm neonate: using a clinical utility framework to translate research tools into clinical care
Journal of Perinatology (2022)
-
Free-breathing 3-D quantification of infant body composition and hepatic fat using a stack-of-radial magnetic resonance imaging technique
Pediatric Radiology (2019)