Abstract
Background
Asphyxia is the most common reason for newborns to fail to make a successful fetal-to-neonatal transition. There is currently a lack of data evaluating hemodynamic effects of epinephrine during neonatal cardiopulmonary resuscitation.
Methods
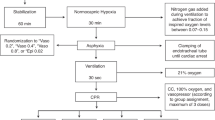
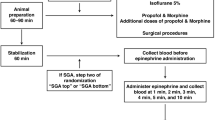
Twenty-four newborn piglets were exposed to asphyxia. Thereafter, positive pressure ventilation was commenced for 30 s, followed by chest compressions (CC). Piglets were randomized into three experimental groups: 3:1 compression:ventilation ratio; CC during sustained inflation (SI) at a rate of 90 CC per minute, or CC during SI at a rate of 120 CC per minute. Epinephrine (0.01 mg/kg per dose) was administered to a maximum of four doses. Hemodynamic parameters were measured throughout the experiment.
Results
Animals were divided into survivors and nonsurvivors. End-diastolic and developed pressures declined after epinephrine administration in the survivor group. dp/dt min was significantly higher in the survivor group whereas dp/dt max showed no significant differences. Epinephrine had no effect on either heart rate or cardiac output in both groups. Ejection fraction increased after epinephrine with no significant difference between groups.
Conclusion
Epinephrine did not affect survival rates or return of spontaneous circulation in our postnatal porcine model of neonatal asphyxia.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Kapadia V, Wyckoff MH . Chest compressions for bradycardia or asystole in neonates. Clin Perinatol 2012;39:833–842.
Solevåg AL, Cheung P-Y, O'Reilly M, Schmölzer GM . A review of approaches to optimise chest compressions in the resuscitation of asphyxiated newborns. Arch Dis Child Fetal Neonatal Ed 2016;101:F272–6.
Pinto M, Solevåg AL, O'Reilly M, Aziz K, Cheung P-Y, Schmölzer GM . Evidence on adrenaline use in resuscitation and its relevance to newborn infants: a non-systematic review. Neonatology 2016;111:37–44.
Kapadia VS, Wyckoff MH . Epinephrine use during newborn resuscitation. Front Pediatr 2017;5:97.
Barber CA, Wyckoff MH . Use and efficacy of endotracheal versus intravenous epinephrine during neonatal cardiopulmonary resuscitation in the delivery room. Pediatrics 2006;118:1028–1034.
Kilkenny C, Browne WJ, Cuthill IC, Emerson M, Altman DG . Improving bioscience research reporting: the ARRIVE guidelines for reporting animal research. Osteoarthr Cartil 2012;20:256–260.
Li ES, Cheung P-Y, Lee T-F, Lu M, O'Reilly M, Schmölzer GM . Return of spontaneous circulation is not affected by different chest compression rates superimposed with sustained inflations during cardiopulmonary resuscitation in newborn piglets. PLoS ONE 2016;11:e0157249–14.
Li ES, Görens I, Cheung P-Y et al. Chest compressions during sustained inflations improve recovery when compared to a 3:1 compression:ventilation ratio during cardiopulmonary resuscitation in a neonatal porcine model of asphyxia. Neonatology 2017;112:337–346.
Wyckoff MH, Aziz K, Escobedo MB et al. Part 13: neonatal resuscitation: 2015 American Heart Association Guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care (reprint). Pediatrics 2015;136 (Suppl 2): S196–S218.
Weiner GM, Niermeyer S . Medications in neonatal resuscitation: epinephrine and the search for better alternative strategies. Clin Perinatol 2012;39:843–855.
Idris AH, Becker LB, Fuerst RS et al. Effect of ventilation on resuscitation in an animal model of cardiac arrest. Circulation 1994;90:3063–3069.
Linner R, Werner O, Perez-de-Sa V, Cunha-Goncalves D . Early adrenaline administration does not improve circulatory recovery during resuscitation from severe asphyxia in newborn piglets. Resuscitation 2012;83:1298–1303.
Sobotka KS, Polglase GR, Schmölzer GM, Davis PG, Klingenberg C, Hooper SB . Effects of chest compressions on cardiovascular and cerebral hemodynamics in asphyxiated near-term lambs. Pediatr Res 2015;78:395–400.
Halling C, Sparks JE, Christie L, Wyckoff MH . Efficacy of intravenous and endotracheal epinephrine during neonatal cardiopulmonary resuscitation in the delivery room. J Pediatr 2017;185:232–236.
Vali P, Chandrasekharan P, Rawat M et al. Evaluation of timing and route of epinephrine in a neonatal model of asphyxial arrest. J Am Heart Assoc 2017;6:e004402–e004413.
McNamara PJ, Engelberts D, Finelli M, Adeli K, Kavanagh BP . Vasopressin improves survival compared with epinephrine in a neonatal piglet model of asphyxial cardiac arrest. Pediatr Res 2014;75:738–748.
Wenzel V, Krismer AC, Arntz HR, Sitter H, Stadlbauer KH, Lindner KH . A comparison of vasopressin and epinephrine for out-of-hospital cardiopulmonary resuscitation. N Engl J Med 2004;350:105–113.
Morgan RW, Kilbaugh TJ, Shoap W et al. A hemodynamic-directed approach to pediatric cardiopulmonary resuscitation (HD-CPR) improves survival. Resuscitation 2017;111:41–47.
Perondi MBM, Reis AG, Paiva EF, Nadkarni VM, Berg RA . A comparison of high-dose and standard-dose epinephrine in children with cardiac arrest. N Engl J Med 2004;350:1722–1730.
Savani M, Upadhyay K, Talati AJ . Characteristics and outcomes of very low birth weight infants receiving epinephrine during delivery room resuscitation. Resuscitation 2017;115:1–4.
Caspi J, Coles JG, Benson LN et al. Age-related response to epinephrine-induced myocardial stress. A functional and ultrastructural study. Circulation 1991;84:III394–III399.
Perlman JM, Wyllie J, Kattwinkel J et al. Part 7: neonatal resuscitation: 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations (Reprint). Pediatrics 2015;136 (Suppl 2): S120–S166.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
AUTHOR CONTRIBUTIONS
Conception and design: G.M.S. and P.Y.C. Collection and assembly of data: G.M.S., E.S.L., T.F.L., M.L., M.O.R., P.Y.C., and M.W. Analysis and interpretation of the data: G.M.S., E.S.L., T.F.L., M.L., M.O.R., P.Y.C., M.W., and M.O. Drafting of the article: G.M.S., E.S.L., T.F.L., M.L., M.O.R., P.Y.C., M.W., and M.O. Critical revision of the article for important intellectual content: G.M.S., E.S.L., T.F.L., M.L., M.O.R., P.Y.C., M.W., and M.O. Final approval of the article: G.M.S., E.S.L., T.F.L., M.L., M.O.R., P.Y.C., M.W., and M.O.
STATEMENT OF FINANCIAL SUPPORT:
We thank the public for donating money to our funding agencies: E.S.L. was supported by Alberta Innovates–Health Solutions Summer-Studentship. G.M.S. is a recipient of the Heart and Stroke Foundation/University of Alberta Professorship of Neonatal Resuscitation, a National New Investigator of the Heart and Stroke Foundation Canada, and an Alberta New Investigator of the Heart and Stroke Foundation Alberta. We acknowledge the Neonatal Resuscitation Program Canada Grant Program within the Canadian Society of Pediatrics for supporting the study.
Rights and permissions
About this article
Cite this article
Wagner, M., Cheung, PY., Li, E. et al. Effects of epinephrine on hemodynamic changes during cardiopulmonary resuscitation in a neonatal piglet model. Pediatr Res 83, 897–903 (2018). https://doi.org/10.1038/pr.2017.316
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/pr.2017.316
This article is cited by
-
Pharmacokinetics and pharmacodynamics of endotracheal versus supraglottic airway epinephrine in a healthy neonatal piglet model
Pediatric Research (2025)
-
Pharmacokinetic and pharmacodynamic evaluation of various vasopressin doses and routes of administration in a neonatal piglet model
Scientific Reports (2024)
-
Epinephrine vs placebo in neonatal resuscitation: ROSC and brain MRS/MRI in term piglets
Pediatric Research (2023)