Abstract
Background
Early-life adversity that increases the risk of growth stunting is hypothesized to increase the risk of obesity and, in girls, early-onset puberty. This hypothesis was tested in children adopted from orphanages.
Methods
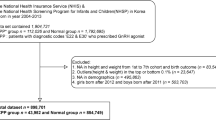
Post-institutionalized (PI) youth were compared with youth reared in comparable families (non-adopted; NA) on height, weight, pubertal stage, and fat mass (127 PI, 80 female; 156 NA, 85 female, aged 7–14 years). Anthropometric findings at adoption were obtained from first US clinic visits.
Results
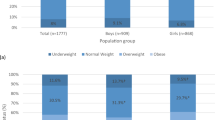
Overall, 25% of PI youth were height-stunted (<3rd percentile) at adoption. Years post adoption, PI youth had lower BMI-for-age (P=0.004), height-for-age (P<0.001), and less body fat (P<0.001) than NA youth had, but they did not differ by sex. Pubertal status did not differ by group or sex. The anthropometric findings held when the stunted-at-adoption subset was examined; they were also less likely to be in central puberty than other PI youth.
Conclusion
Early deprived orphanage care increases the risk of growth stunting but not obesity in children adopted into US families, and it does not independently contribute to early-onset puberty for PI girls. The role of the environment following early adversity may modify the impact of early adverse care.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Bateson P, Barker D, Clutton-Brock T et al, Developmental plasticity and human health. Nature 2004;430:419–21.
Popkin BM, Richards MK, Montiero CA . Stunting is associated with overweight in children of four nations that are undergoing the nutrition transition. J Nutr 1996;126:3009–16.
Clarkin PF . Adiposity and height of adult Hmong refugees: relationship with war-related early malnutrition and later migration. Am J Hum Biol 2008;20:174–84.
Villamor E, Jansen EC . Nutritional determinants of the timing of puberty. Annu Rev Public Health 2016;37:33–46.
Mendle J, Ryan RM, McKone KM . Early childhood maltreatment and pubertal development: replication in a population-based sample. J Res Adolesc 2016;26:595–602.
Mendle J, Leve LD, Van Ryzin M, Natsuaki MN, Ge X . Associations between early life stress. Child maltreatment, and pubertal development among girls in foster care. J Res Adolesc 2011;21:871–80.
Boynton-Jarrett R, Wright RJ, Putnam FW . Childhood abuse and age at menarche. J Adolesc Health 2013;52:241–7.
Johnson DE, Gunnar MR IV . Growth failure in institutionalized children. Monogr Soc Res Child Dev 2011;76:92–126.
Johnson DE . Long-term medical issues in international adoptees. Pediatr Ann 2000;29:234–41.
Kroupina MG, Eckerle JK, Fuglestad AJ et al, Associations between physical growth and general cognitive functioning in international adoptees from Eastern Europe at 30 months post-arrival. J Neurodev Disord 2015;7:36.
Miller BS, Kroupina MG, Mason P et al, Determinants of catch-up growth in international adoptees from Eastern Europe. Int J Pediatr Endocrinol 2010;2010:107252.
Monk C, Georgieff MK, Osterholm EA . Research review: maternal prenatal distress and poor nutrition - mutually influencing risk factors affecting infant neurocognitive development. J Child Psychol Psychiatry 2013;54:115–30.
Adair LS . Size at birth and growth trajectories to young adulthood. Am J Hum Biol 2007;19:327–37.
Lucas A, Fewtrell MS, Cole TJ . Fetal origins of adult disease-the hypothesis revisited. BMJ 1999;319:245–9.
Sawaya AL, Roberts S . Stunting and future risk of obesity: principal physiological mechanisms. Cad Saude Publica 2003;19:S21–8.
Monteiro PO, Victora CG . Rapid growth in infancy and childhood and obesity in later life—a systematic review. Obes Rev 2005;6:143–54.
Golub MS, Collman GW, Foster PM et al, Public health implications of altered puberty timing. Pediatrics 2008;121:S218–30.
Downing J, Bellis MA . Early pubertal onset and its relationship with sexual risk taking, substance use and anti-social behaviour: a preliminary cross-sectional study. BMC Public Health 2009;9:446.
Dunbar J, Sheeder J, Lezotte D . Age at menarche and first pregnancy among psychosocially at-risk adolescents. Am J Public Health 2008;98:1822–4.
Glynn JR, Kayuni N, Gondwe L, Price AJ, Crampin AC . Earlier menarche is associated with a higher prevalence of Herpes simplex type-2 (HSV-2) in young women in rural Malawi. Elife 2014;3:e01604.
Proos LA . Growth & development of Indian children adopted in Sweden. Indian J Med Res 2009;130:646–50.
Teilmann G, Pedersen CB, Skakkebaek NE, Jensen TK . Increased risk of precocious puberty in internationally adopted children in Denmark. Pediatrics 2006;118:e391–9.
Partsch CJ, Sippell WG . Pathogenesis and epidemiology of precocious puberty. Effects of exogenous oestrogens. Hum Reprod Update 2001;7:292–302.
Mul D, Oostdijk W, Drop SL . Early puberty in adopted children. Horm Res 2002;57:1–9.
Krstevska-Konstantinova M, Charlier C, Craen M et al, Sexual precocity after immigration from developing countries to Belgium: evidence of previous exposure to organochlorine pesticides. Hum Reprod 2001;16:1020–6.
Hayes P, Tan TX . Timing of menarche in girls adopted from China: a cohort study. Child Care Health Dev 2016;42:859–62.
Mason P, Narad C . Long-term growth and puberty concerns in international adoptees. Pediatr Clin North Am 2005;52:1351–68.
de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J . Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ 2007;85:660–7.
Dempster P, Aitkens S . A new air displacement method for the determination of human body composition. Med Sci Sports Exerc 1995;27:1692–7.
Marshall WA, Tanner JM . Variations in pattern of pubertal changes in girls. Arch Dis Child 1969;44:291–303.
Marshall WA, Tanner JM . Variations in the pattern of pubertal changes in boys. Arch Dis Child 1970;45:13–23.
Carskadon MA, Acebo C . A self-administered rating scale for pubertal development. J Adolesc Health 1993;14:190–5.
Petersen AC, Crockett L, Richards M, Boxer A . A self-report measure of pubertal status: reliability, validity, and initial norms. J Youth Adolesc 1988;17:117–33.
Ogden CL, Carroll MD, Kit BK, Flegal KM . Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014;311:806–14.
Walker SP, Chang SM, Powell CA . The association between early childhood stunting and weight status in late adolescence. Int J Obes 2007;31:347–52.
Schwandt P, Haas GM . Is the ratio waist circumference to height (WHtR) of 0.5 a universal measure for abdominal adiposity in children and adolescents? Int J Obes 2016;40:1141–2.
Skidmore PM, Cassidy A, Swaminathan R et al, An obesogenic postnatal environment is more important than the fetal environment for the development of adult adiposity: a study of female twins. Am J Clin Nutr 2009;90:401–6.
Addo OY, Miller BS, Lee PA, Hediger ML, Himes JH . Age at hormonal onset of puberty based on luteinizing hormone, inhibin B, and body composition in preadolescent U.S. girls. Pediatr Res 2014;76:564–70.
Zhang YX, Zhao JS, Chu ZH . Children and adolescents with low body mass index but large waist circumference remain high risk of elevated blood pressure. Int J Cardiol 2016;215:23–5.
Gonzalez-Barranco J, Rios-Torres JM . Early malnutrition and metabolic abnormalities later in life. Nutr Rev 2004;62:S134–9.
Acknowledgements
We thank the families for their participation and the International Adoption Project. We thank Tori Simenec, Bao Moua, and Lea Neumann for their assistance with the study, as well as our nurses Janet Goodwalt, Terri Jones, and Melissa Stoll. This material is based on work supported by the National Science Foundation Graduate Research Fellowship under Grant No. (NSF Grant 00039202).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
STATEMENT OF FINANCIAL SUPPORT
This study was funded by Grant Number 5R01 HD075349-02 (to M.G.) from the Eunice Kennedy Shriver National Institute of Child Health & Human Development (NICHD) at the National Institute of Health (NIH).
Disclaimer
Any opinion, findings, and conclusions or recommendations expressed in this material are those of the authors(s) and do not necessarily reflect the views of the National Science Foundation.
Rights and permissions
About this article
Cite this article
Reid, B., Miller, B., Dorn, L. et al. Early growth faltering in post-institutionalized youth and later anthropometric and pubertal development. Pediatr Res 82, 278–284 (2017). https://doi.org/10.1038/pr.2017.35
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/pr.2017.35
This article is cited by
-
Auxological and endocrinological features in internationally adopted children
Italian Journal of Pediatrics (2020)
-
Auxo-endocrinological features in a cohort of internationally adopted children in Italy
World Journal of Pediatrics (2019)
-
Catch-up growth, metabolic, and cardiovascular risk in post-institutionalized Romanian adolescents
Pediatric Research (2018)