Abstract
Background
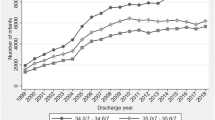
Extremely preterm infants (EPT, <29 weeks’ gestation) represent only 0.9% of births in the United States; yet these infants are the focus of most published research. Moderately preterm neonates (MPT, 29–336/7 weeks) are an understudied group of high-risk infants.
Methods
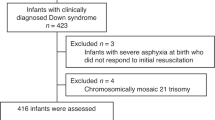
To determine the neonatal outcomes of MPT infants across the gestational age spectrum, and to compare these with EPT infants. A prospective observational cohort was formed in 18 level 3–4 neonatal intensive care units (NICUs) in the Eunice Kennedy Shriver NICHD Neonatal Research Network. Participants included all MPT infants admitted to NICUs and all EPT infants born at sites between January 2012 and November 2013. Antenatal characteristics and neonatal morbidities were abstracted from records using pre-specified definitions by trained neonatal research nurses.
Results
MPT infants experienced morbidities similar to, although at lower rates than, those of EPT infants. The main cause of mortality was congenital malformation, accounting for 43% of deaths. Central Nervous System injury occurred, including intraventricular hemorrhage. Most MPT infants required respiratory support, but sequelae such as bronchopulmonary dysplasia were rare. The primary contributors to hospitalization beyond 36 weeks’ gestation were inability to achieve adequate oral intake and persistent apnea.
Conclusions
MPT infants experience morbidity and prolonged hospitalization. Such morbidity deserves focused research to improve therapeutic and prevention strategies.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Martin JA, Hamilton BE, Osterman MJ, Curin SC, Mathews TJ . Births: final data for 2013. Natl Vital Stat Rep 2015;64:1–65.
NICHD Neonatal Research Network, protocol list. neonatal.rti.org. Accessed 11 March 2016.
Kattwinkel J, Bloom BT, Delmore P et al, Prophylactic administration of calf lung surfactant is more effective than early treatment of respiratory distress syndrome in neonates of 29 through 32 weeks gestation. Pediatrics 1993;92:90–98.
Been JV, Lugtenberg MJ, Smets E et al, Preterm birth and childhood wheezing disorders: a systematic review and meta-analysis. PLoS Med 2014;11:e1001596.
Colin AA, McEvoy C, Castile RG . Respiratory morbidity and lung function in preterm infants of 32 to 36 weeks gestational age. Pediatrics 2010;126:115–118.
Saarenpaa HK, Tikanmaki M, Siola-Leppanen M et al, Lung function in very low birth weight adults. Pediatrics 2015;136:642–650.
Lindstrom K, Winbladh B, Haglund B, Hiern A . Preterm infants as young adults: a Swedish national cohort study. Pediatrics 2007;120:70–77.
Moster D, Lie RT, Markestad T . Long term medical and social consequences of preterm birth. NEJM 2008;359:262–273.
Stoll BJ, Hansen NI, Bell EF et al, Trends in care practices, morbidity and mortality of extremely preterm neonates, 1993-2012. JAMA 2015;314:1039–1051.
Walsh MC, Kliegman RM . Necrotizing enterocolitis: treatment based on staging criteria. Pediatr Clin North Am 1986;33:179–201.
Papille LA, Burstein J, Burstein R, Koffler H . Incidence and evolution of supependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr 1978;92:529–534.
International Committee for the Classification of Retinopathy of Prematurity. The international classification of retinopathy of prematurity revisited. Arch Ophthalmol 2005;123:991–999.
Thoyre SM, Shaker CS, Pridham KF . The early feeding skills assessment for preterm infants. Neonatal Netw 2005;24:7–16.
Eichenwald EC, Zupancic JA, Mao WY, Richardson DK, McCormick MC, Escobar GJ . Variation in diagnosis of apnea in moderatelyly preterm infants predicts length of stay. Pediatrics 2011;127:e53–e58.
Eichenwald EC, the Committee on the Fetus and Newborn, American Academy of Pediatrics. Apnea of prematurity. Pediatrics 2015;137:e20153757.
Manuck TA, Murguia Rice M, Bailit JL et al, Preterm neonatal morbidity and mortality by gestational age: a contemporary cohort. Am J Obstet Gynecol 2016;215:103.e1–103.e14.
Grobham WA, Bailit JL, Rice MM et al, Can differences in obstetric outcomes be explained by differences in the care provided? The MFMU APEX Study. Am J Obstet Gynecol 2014;211:147.e1–147.e16.
Boyle EM, Johnson S, Manktelow B et al, Neonatal outcomes and delivery of care for infants born late preterm or moderatelyly preterm: a prospective population based study. Arch Dis Child Fetal Neonatal Ed 2015;100:F479–F485.
Walsh MC, Yao Q, Horbar JD, Carpenter JH, Lee SK, Ohlsson A . Changes in the use of postnatal steroids for bronchopulmonary dysplasia in 3 large neonatal networks. Pediatrics 2006;118:e1328–e1335.
Acknowledgements
Funding Sources: The National Institutes of Health, the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), and the National Center for Advancing Translational Sciences provided grant support for the Neonatal Research Network’s Moderately Preterm Registry through cooperative agreements. Although NICHD staff did have input into the study design, conduct, analysis, and manuscript drafting, the content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author contributions
The contributions made by each author for this manuscript are given in detail below.
The MPR Subcommittee investigators have monthly conference calls, during which protocol design and implementation issues are discussed, manuscripts are reviewed, and input obtained. The following authors have made significant contributions as determined by the Uniform Requirements for Manuscripts Submitted to Biomedical Journals:
Michele C. Walsh, MD, MS, is the Lead Principal Investigator (PI) at Case Western Reserve University (CWRU) and the Chair of the Moderately Preterm Registry Protocol Subcommittee. She developed the study and managed protocol implementation. As the PI at CWRU, she oversaw enrollment at the site—which enrolled 302 infants in this study. Walsh drafted the manuscript and received input from the authors below as part of manuscript revision. Walsh had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Edward F. Bell, MD, is the PI at the University of Iowa and a member of the Moderately Preterm Registry Protocol Subcommittee. He helped develop the study and manage protocol implementation. As the PI at the University of Iowa, he oversaw enrollment at the site—which enrolled 495 infants in this study. He contributed critical revisions of the manuscript and approved the final manuscript for submission.
Sarah Kandefer, BS, served as the primary statistician for the study, and completed the statistical analyses for the paper. She developed the tables for the paper and provided critical revision to the manuscript and approved the final version of the manuscript.
Waldemar A. Carlo, MD, is the PI at the University of Alabama at Birmingham (UAB) and a member of the Moderately Preterm Registry Protocol Subcommittee. He helped develop the study and manage protocol implementation. As the PI at UAB, he oversaw enrollment at the site—which enrolled 537 infants in this study. He contributed critical revisions of the manuscript and approved the final manuscript for submission.
Carl T. D’Angio, MD, is the PI at the University of Rochester and a member of the Moderately Preterm Registry Protocol Subcommittee. He helped develop the study and manage protocol implementation. As the PI at the University of Rochester, he oversaw enrollment at the site—which enrolled 617 infants in this study. He contributed critical revisions of the manuscript and approved the final manuscript for submission.
Abbot R. Laptook, MD, is the PI at Brown University and a member of the Moderately Preterm Registry Protocol Subcommittee. He helped develop the study and manage protocol implementation. As the PI at Brown University, he oversaw enrollment at the site—which enrolled 424 infants in this study. He contributed critical revisions of the manuscript and approved the final manuscript for submission.
Pablo J. Sanchez, MD, is the PI at Nationwide Children’s Hospital and a member of the Moderately Preterm Registry Protocol Subcommittee. He helped develop the study and manage protocol implementation. As the PI at Nationwide Children’s Hospital, he oversaw enrollment at the site—which enrolled 512 infants in this study. He contributed critical revisions of the manuscript and approved the final manuscript for submission.
Barbara J. Stoll, MD, is the PI at Emory University and the Vice Chair of the Moderately Preterm Registry Protocol Subcommittee. She helped develop the study and manage protocol implementation. As the PI at Emory University, she oversaw enrollment at the site—which enrolled 335 infants in this study. She contributed critical revisions of the manuscript and approved the final manuscript for submission.
Seetha Shankaran, MD, is the PI at Wayne State University and a member of the Moderately Preterm Registry Protocol Subcommittee. She helped develop the study and manage protocol implementation. As the PI at Wayne State University, she oversaw enrollment at the site—which enrolled 363 infants in this study. She contributed critical revisions of the manuscript and approved the final manuscript for submission.
Krisa P. Van Meurs, MD, is the PI at Stanford University and a member of the Moderately Preterm Registry Protocol Subcommittee. She helped develop the study and manage protocol implementation. As the PI at Stanford University, she oversaw enrollment at the site—which enrolled 205 infants in this study. She contributed critical revisions of the manuscript and approved the final manuscript for submission.
Betty R. Vohr, MD, is the Follow-up PI at Brown University and a member of the Moderately Preterm Registry Protocol Subcommittee. She helped develop and implement the study and contributed critical revisions of the manuscript and approved the final manuscript for submission.
Rosemary D. Higgins, MD, served as the Program Scientist for the NICHD NRN and is a member of the Moderately Preterm Registry Protocol Subcommittee. Dr Higgins helped develop the protocol, oversaw recruitment, and assisted with data edits from the sites. She also provided critical revision to the manuscript and approved the final version of the manuscript.
Abhik Das, PhD, is the PI for the NRN Data Coordinating Center and a member of the Moderately Preterm Registry Protocol Subcommittee. Das oversaw all aspects of the statistical analysis, provided critical revisions to the manuscript, and approved the final version of the manuscript.
Ellen C. Hale, BS, RN, CCRC, is the Coordinator at Emory University and a member of the Moderately Preterm Registry Protocol Subcommittee. She helped develop the study and manage protocol implementation. As the Coordinator at Emory University, she enrolled 335 infants in this study. She contributed critical revisions of the manuscript and approved the final manuscript for submission.
Nancy S. Newman, RN, is the Coordinator at CWRU and a member of the Moderately Preterm Registry Protocol Subcommittee. She helped develop the study and manage protocol implementation. As the Coordinator at CWRU, she enrolled 302 infants in this study. She contributed critical revisions of the manuscript and approved the final manuscript for submission.
Kurt Schibler, MD, is the PI at Cincinnati Children’s Medical Center (CCMC). As the PI he oversaw enrollment at the site—which enrolled 683 infants in this study. He contributed critical revisions of the manuscript and approved the final manuscript for submission.
Barbara Schmidt, MD, is the PI at the University of Pennsylvania. As the PI she oversaw enrollment at the site—which enrolled 511 infants in this study. She contributed critical revisions of the manuscript and approved the final manuscript for submission.
C. Michael Cotten, MD, MHS, is the PI at Duke University. As the PI he oversaw enrollment at the site—which enrolled 457 infants in this study. He contributed critical revisions of the manuscript and approved the final manuscript for submission.
Kathleen A. Kennedy, MD, MPH, is the PI at the University of Texas Health Science Center at Houston. As the PI she oversaw enrollment at the site—which enrolled 456 infants in this study. She contributed critical revisions of the manuscript and approved the final manuscript for submission.
Brenda B. Poindexter, MD, MS, is the PI at Indiana University. As the PI, she oversaw enrollment at the site—which enrolled 333 infants in this study. She contributed critical revisions of the manuscript and approved the final manuscript for submission.
Kristi L. Watterberg, MD, is the PI at the University of New Mexico. As the PI, she oversaw enrollment at the site—which enrolled 242 infants in this study. She contributed critical revisions of the manuscript and approved the final manuscript for submission.
William E. Truog, MD, is the PI at Children's Mercy Hospital, Kansas City. As the PI, he oversaw enrollment at the site—which enrolled 172 infants in this study. He contributed critical revisions of the manuscript and approved the final manuscript for submission.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Presentations: portions of the material in this manuscript were presented at the Pediatric Academic Society Meeting, May 2014, Vancouver, BC, Canada.
Rights and permissions
About this article
Cite this article
Walsh, M., Bell, E., Kandefer, S. et al. Neonatal outcomes of moderately preterm infants compared to extremely preterm infants. Pediatr Res 82, 297–304 (2017). https://doi.org/10.1038/pr.2017.46
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/pr.2017.46
This article is cited by
-
Standardizing feeding strategies for preterm infants born greater than 1500 grams
Pediatric Research (2025)
-
Respiratory insufficiency, feeding issues and length of stay in 33–36 weeks post-menstrual age infants
Pediatric Research (2025)
-
Brain oxygenation monitoring during neonatal stabilization and resuscitation and its potential for improving preterm infant outcomes: a systematic review and meta-analysis with Bayesian analysis
European Journal of Pediatrics (2025)
-
Sample entropy correlates with intraventricular hemorrhage and mortality in premature infants early in life
Pediatric Research (2024)
-
Impact of concomitant necrotizing enterocolitis on mortality in very low birth weight infants with intraventricular hemorrhage
Journal of Perinatology (2023)