Abstract
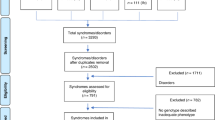
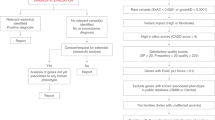
Micrognathia is a common craniofacial deformity which represents hypoplastic development of the mandible, accompanied by retrognathia and consequent airway problems. Usually, micrognathia is accompanied by multiple systematic defects, known as syndromic micrognathia, and is in close association with genetic factors. Now, large quantities of pathogenic genes of syndromic micrognathia have been revealed. However, how these different pathogenic genes could lead to similar phenotypes, and whether there are some common characteristics among these pathogenic genes are still unknown. In this study, we proposed a genetic-phenotypic classification of syndromic micrognathia based on pathogenic genes information obtained from Phenolyzer, DAVID, OMIM, and PubMed database. Pathogenic genes of syndromic micrognathia could be divided into four groups based on gene function, including cellular processes and structures, cell metabolism, cartilage and bone development, and neuromuscular function. In addition, these four groups exhibited various clinical characteristics, and the affected systems, such as central nervous system, skeletal system, cardiovascular system, oral and dental system, respiratory system and muscle, were different in these four groups. This classification could provide meaningful insights into the pathogenesis of syndromic micrognathia, and offer some clues for understanding the molecular mechanism, as well as guiding precise clinical diagnosis and treatment for syndromic micrognathia.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Singh DJ, Bartlett SP. Congenital mandibular hypoplasia: analysis and classification. J Craniofacial Surg. 2005;16:291.
Gundlach KK, Holtje WJ. The isolated mandibular ramus - a hitherto rarely described anomaly of the mandible. Pathog Treat J Cranio-Maxillo-Facial Surg. 2013;41:450–6.
Benko S, Fantes JA, Amiel J, Kleinjan DJ, Thomas S, Ramsay J, et al. Highly conserved non-coding elements on either side of SOX9 associated with Pierre Robin sequence. Nat Genet. 2009;41:359–64.
Cohen ASA, Yap DB, Suzanne LME, Chieko C, Ramos‐Arroyo MA, Natália T, et al. Weaver syndrome‐associated EZH2 protein variants show impaired histone methyltransferase function in vitro. Hum Mutat. 2016;37:301–7.
Dai J, Si J, Wang M, Huang L, Fang B, Shi J, et al. Tcof1-related molecular networks in Treacher Collins syndrome. J Craniofacial Surg. 2016;27:1420.
McMillin MJ, Beck AE, Chong JX, Shively KM, Buckingham KJ, Gildersleeve HI, et al. Mutations in PIEZO2 cause Gordon syndrome, Marden-Walker syndrome, and distal arthrogryposis type 5. Am J Hum Genet. 2014;94:734–44.
Yang H, Robinson PN, Wang K. Phenolyzer: phenotype-based prioritization of candidate genes for human diseases. Nat Methods. 2015;12:841.
Hamosh A, Scott AF, Amberger JS, Bocchini CA, Mckusick VA. Online Mendelian Inheritance in Man (OMIM), a knowledgebase of human genes and genetic disorders. Nucleic Acids Res. 2005;33:514–7.
Huang da W, Sherman BT, Lempicki RA. Systematic and integrative analysis of large gene lists using DAVID bioinformatics resources. Nat Protoc. 2009;4:44–57.
Bicknell LS, Bongers EMHF, Leitch A, Brown S, Schoots J, Harley ME, et al. Mutations in the pre-replication complex cause Meier-Gorlin syndrome. Nat Genet. 2011;43:356–9.
Bacrot S, Doyard M, Huber C, Alibeu O, Feldhahn N, Lehalle D, et al. Mutations in SNRPB, encoding components of the core splicing machinery, cause cerebro-costo-mandibular syndrome. Hum Mutat. 2015;36:187–90.
Hess D, Keusch JJ, Oberstein SA, Hennekam RC, Hofsteenge J. Peters Plus syndrome is a new congenital disorder of glycosylation and involves defective Omicron-glycosylation of thrombospondin type 1 repeats. J Biol Chem. 2008;283:7354–60.
Robertson SP. Otopalatodigital syndrome spectrum disorders: otopalatodigital syndrome types 1 and 2, frontometaphyseal dysplasia and Melnick-Needles syndrome. Eur J Hum Genet Ejhg. 2007;15:3–9.
Schindeler A, Little DG. Ras‐MAPK Signaling in osteogenic differentiation: friend or foe? J Bone Miner Res. 2010;21:1331–8.
Chai Y, Jiang X, Ito Y, Jr BP, Han J, Rowitch DH, et al. Fate of the mammalian cranial neural crest during tooth and mandibular morphogenesis. Development . 2000;127:1671–9.
De BP, Muller P, Wijmenga C, Klomp LW. Molecular pathogenesis of Wilson and Menkes disease: correlation of mutations with molecular defects and disease phenotypes. J Med Genet. 2007;44:673.
Grubenmann CE, Frank CG, Hülsmeier AJ, Schollen E, Matthijs G, Mayatepek E, et al. Deficiency of the first mannosylation step in the N-glycosylation pathway causes congenital disorder of glycosylation type Ik. Hum Mol Genet. 2017;13:535.
Waterham HR, Koster J, Romeijn GJ, Hennekam RC, Vreken P, Andersson HC, et al. Mutations in the 3beta-hydroxysterol Delta24-reductase gene cause desmosterolosis, an autosomal recessive disorder of cholesterol biosynthesis. Am J Hum Genet. 2001;69:685–94.
Giglio MJ, Lama MA. Effect of experimental diabetes on mandible growth in rats. Eur J Oral Sci. 2001;109:193–7.
Wang R, Martinez-Frias ML, Graham JM Jr. Infants of diabetic mothers are at increased risk for the oculo-auriculo-vertebral sequence: a case-based and case-control approach. J Pedia. 2002;141:611–7.
Cancedda R, Descalzi CF, Castagnola P. Chondrocyte differentiation. Int Rev Cytol. 1995;159:265–358.
Yoshida CA, Furuichi T, Fujita T, Fukuyama R, Kanatani N, Kobayashi S, et al. Core-binding factor beta interacts with Runx2 and is required for skeletal development. Nat Genet. 2002;32:633–8.
Pm VDK, Buma P, Van KT, Wb VDB. Interaction of chondrocytes, extracellular matrix and growth factors: relevance for articular cartilage tissue engineering. Osteoarthr Cartil. 2002;10:631–7.
Radlanski RJ, Klarkowski MC. Bone remodeling of the human mandible during prenatal development. J Orofac Orthop. 2001;62:191–201.
Yaeger JA. Principles of bone remodeling; an account of post-natal growth and remodeling processes in long bones and the mandible. J Am Med Assoc. 1963;184:906.
Motyckova G, Fisher DE. Pycnodysostosis: role and regulation of cathepsin K in osteoclast function and human disease. Curr Mol Med. 2002;2:407.
Robinson P, Lipscomb S, Preston LC, Altin E, Watkins H, Ashley CC, et al. Mutations in fast skeletal troponin I, troponin T, and β-tropomyosin that cause distal arthrogryposis all increase contractile function. FASEB J. 2007;21:896–905.
Salinas S, Proukakis C, Crosby A, Warner TT. Hereditary spastic paraplegia: clinical features and pathogenetic mechanisms. Lancet Neurol. 2008;7:1127–38.
Benomran T, Fahiminiya S, Sorfazlian N, Almuriekhi M, Nawaz Z, Nadaf J, et al. Nonsense mutation in the WDR73 gene is associated with Galloway-Mowat syndrome. J Med Genet. 2015;52:381–90.
Rot I, Mardesicbrakus S, Costain WJ, Saragababic M, Kablar B. Role of skeletal muscle in mandible development. Histol Histopathol. 2014;29:1377–94.
Hichijo N, Kawai N, Mori H, Sano R, Ohnuki Y, Okumura S, et al. Effects of the masticatory demand on the rat mandibular development. J Oral Rehabil. 2014;41:581–7.
Tucker AS, Al KA, Ferguson CA, Bach I, Rosenfeld MG, Sharpe PT. Conserved regulation of mesenchymal gene expression by Fgf-8 in face and limb development. Development. 1999;126:221–8.
Szeto DP, Rodriguez-Esteban C, Ryan AK, O’Connell SM, Liu F, Kioussi C, et al. Role of the Bicoid-related homeodomain factor Pitx1 in specifying hindlimb morphogenesis and pituitary development. Genes Dev. 1999;13:484–94.
Chen Q, Zhao Y, Shen G, Dai J. Etiology and Pathogenesis of Hemifacial Microsomia. J Dental Res. 2018:0022034518795609.
Roche N, Houtmeyers P, Janssens S, Blondeel P. Barber-Say syndrome in a father and daughter. Am J Med Genet A. 2010;152a:2563–8.
Gupta VA, Ravenscroft G, Shaheen R, Todd EJ, Swanson LC, Shiina M, et al. Identification of KLHL41 mutations implicates BTB-Kelch-mediated ubiquitination as an alternate pathway to myofibrillar disruption in Nemaline Myopathy. Am J Hum Genet. 2013;93:1108–17.
Inbal A, Avissar N, Shaklai M, Kuritzky A, Schejter A, Ben-David E, et al. Myopathy, lactic acidosis, and sideroblastic anemia: a new syndrome. Am J Med Genet. 1995;55:372–8.
Basel‐Vanagaite L, Wolf L, Orin M, Larizza L, Gervasini C, Krantz ID, et al. Recognition of the Cornelia de Lange syndrome phenotype with facial dysmorphology novel analysis. Clin Genet. 2016;89:557–63.
Acknowledgements
The study is supported by The National Natural Science Foundation of China (No. 81741028), Shanghai Jiaotong University Joint Foundation of Medicine and Engineering (No. YG2016MS08).
Author information
Authors and Affiliations
Contributions
QC, YZ, YQ, CL, GS, and JD contributed to conception and design, drafted and critically revised the manuscript. GS and JD gave final approval and ensured that questions relating to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Chen, Q., Zhao, Y., Qian, Y. et al. A genetic-phenotypic classification for syndromic micrognathia. J Hum Genet 64, 875–883 (2019). https://doi.org/10.1038/s10038-019-0630-4
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s10038-019-0630-4