Abstract
Introduction
Obesity has numerous etiologies and includes biological factors. Studies have demonstrated that the human adenovirus subtype 36 (Adv36) is an adipogenic agent and causes metabolic alterations. Study results on the prevalence of Adv36 and clinical effects in humans vary substantially. This was a systematic review to summarize the studies on the prevalence of Adv36 infection and its association with human obesity.
Methods
A systematic literature review was conducted using the preferred reporting items for systematic reviews and meta-analysis (PRISMA). Observational or experimental studies found in the Medline, Embase, LILACS, Science Direct and SciELO databases that presented results on the prevalence of Adv36 in humans were included.
Results
Thirty-seven studies were screened. A total of 10,300 adults aged 18–70 years and 4585 children and adolescents aged 3–18 years were assessed. The average prevalence of Adv36 among adults was 22.9%, ranging from 5.5% to 49.8%. Among children and adolescents, the average prevalence of Adv36 was 28.9%, ranging from 7.5% to 73.9%. There was a positive statistical relationship between Adv36 and weight gain, obesity, or metabolic changes in 31 studies. However, in four studies there was no association with obesity, and in one, no association was described. One of the studies showed an inverse correlation, i.e., Adv36 was a protective factor against obesity.
Conclusion
Strong evidence suggested a positive association between viral infection and obesity. However, due to the multi-causality of obesity and heterogeneity of studies, diagnostic tests should be standardized and easily accessible by the population to estimate the overall prevalence of Adv36 infection and its association with obesity.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Obesity: preventing and managing the global epidemic. Report of a WHO Consultation (WHO Technical Report Series 894). Authors: World Health Organization. 252. Publication date: 2000.
WHO. Obesity and overweight. Updated 16 Feb 2018. Available at: http://www.who.int/news-room/factsheets/detail/obesity-and-overweight. Accessed 5 Jan 2020.
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis. Lancet. 2014; 384:766–81. https://doi.org/10.1016/S0140-6736(14)60460-8.
Hruby A, Hu FB. The epidemiology of obesity: a big picture. Pharmacoeconomics. 2015;33:673–89. https://doi.org/10.1007/s40273-014-0243-x.
Hainer V, Zamrazilová H, Kunešová M, Bendlová B, Aldhoon-Hainerová I. Obesity and infection: reciprocal causality. Physiol Res. 2015;64:S105–19. https://doi.org/10.33549/physiolres.933130.
Mullen JT, Moorman DW, Davenport DL. The obesity paradox: body mass index and outcomes in patients undergoing non-bariatric general surgery. Ann Surg. 2009;250:166–72. https://doi.org/10.1097/SLA.0b013e3181ad8935.
Morgan OW, Bramley A, Fowlkes A, Freedman DS, Taylor TH, Gargiullo P. et al. Morbid obesity as a risk factor for hospitalization and death due to 2009 pandemic influenza a(h1n1) disease. PLoS ONE. 2010;5:e9694 https://doi.org/10.1371/journal.pone.0009694.
Arslan E, Atilgan H, Yavasoglu I. The prevalence of Helicobacter pylori in obese subjects. Eur J Intern Med. 2009;20:695–7. https://doi.org/10.1016/j.ejim.2009.07.013.
Uberos J, Molina-Carballo A, Fernandez-Puentes V, Rodriguez-Belmonte R, Munoz-Hoyos A. Overweight and obesity as risk factors for the asymptomatic carrier state of Neisseria meningitidis among a paediatric population. Eur J Clin Microbiol Infect Dis. 2010;29:333–4. https://doi.org/10.1007/s10096-009-0849-7.
Huttunen R, Syrjänen J. Obesity and the risk and outcome of infection. Int J Obes. 2013;37:333–40. https://doi.org/10.1038/ijo.2012.62.
Nadeau KJ, Maahs DM, Daniels SR, Eckel RH. Childhood obesity and cardiovascular disease: links and prevention strategies. Nat Rev Cardiol. 2011;8:513–25. https://doi.org/10.1038/nrcardio.2011.86.
Jubber AS. Respiratory complications of obesity. Int J Clin Pract. 2004;58:573–80. https://doi.org/10.1111/j.1368-5031.2004.00166.x.
Roswall N, Li Y, Sandin S, Ström P, Adami HO, Weiderpass E. Changes in body mass index and waist circumference and concurrent mortality among Swedish women. Obesity. 2017;25:215–22. https://doi.org/10.1002/oby.21675.
Hill JO, Wyatt HR, Melanson EL. Genetic and environmental contributions to obesity. Med Clin North Am. 2000;84:333–45. https://doi.org/10.1016/s0025-7125(05)70224-8.
Campbell AMLV. Genetics of obesity. Aust Fam Phys. 2017;46:456–9.
Aveyard P, Lewis A, Tearne S, Hood K, Christian-Brown A, Adab P. et al. Screening and brief intervention for obesity in primary care: a parallel, two-arm, randomized trial. Lancet. 2016;356:2492–500. https://doi.org/10.1016/S0140-6736(16)31893-1.
Zhang Y, Liu JU, Yao J, Ji G, Qian L, Wang J. et al. Obesity: pathophysiology and Intervention. Nutrients.2014;6:5153–83. https://doi.org/10.3390/nu6115153.
English WJ, Williams DB. Metabolic and bariatric surgery: an effective treatment option for obesity and cardiovascular disease. Prog Cardiovasc Dis. 2018;61:253–69. https://doi.org/10.1016/j.pcad.2018.06.003.
Manna P, Jain SK. Obesity, oxidative stress, adipose tissue dysfunction, and the associated health risks: Causes and therapeutic strategies. Metab Syndr Relat Disord. 2015;13:423–44. https://doi.org/10.1089/met.2015.0095.
Dhurandhar NV. Is obesity caused by an adenovirus?. Expert Rev Anti-Infect Ther. 2012;10:521–4. https://doi.org/10.1586/eri.12.41.
Kim JY, Van de Wall E, Laplante M, Azzara A, Trujillo ME, Hofmann SM. et al. Obesity-associated improvements in metabolic profile through expansion of adipose tissue. J Clin Investig. 2007;117:2621–37. https://doi.org/10.1172/JCI31021.
Lyons MJ, Faust IM, Hemmes RB, Buskirk DR, Hirsch J, Zabriskie JB. A virally induced obesity syndrome in mice. Science. 1982;216:82–5. https://doi.org/10.1126/science.7038878.
Verlaeten O, Griffond B, Khuth ST, Giraudon P, Akaoka H, Belin MF. et al. Down regulation of melanin concentrating hormone in virally induced obesity. Mol Cell Endocrinol. 2001;181:207–19. https://doi.org/10.1016/s0303-7207(01)00488-9.
Herden C, Herzog S, Richt JA, Nesseler A, Christ M, Failing K. et al. Distribution of borna disease virus in the brain of rats infected with an obesity-inducing virus strain. Brain Pathology. 2000;10:39–48. https://doi.org/10.1111/j.1750-3639.2000.tb00241.x.
So PW, Herlihy AH, Bell JD. Adiposity induced by adenovirus 5 inoculations. Int J Obes. 2005;29:603–6. https://doi.org/10.1038/sj.ijo.0802917.
Pasarica M, Shin AC, Yu M, Ou Yang HM, Rathod M, Jen KL. et al. Human adenovirus 36 induces adiposity, increases insulin sensitivity, and alters hypothalamic monoamines in rats. Obesity. 2006;14:1905–13. https://doi.org/10.1038/oby.2006.222.
Carter JK, Ow CL, Smith RE. Rous-associated virus type 7 induces a syndrome in chickens characterized by stunting and obesity. Infect Immunol. 1983;39:410–22.
Dhurandhar NV, Kulkarni P, Ajinkya SM, Sherikar A. Effect of adenovirus infection on adiposity in chicken. Vet Microbiol. 1992;31:101–7. https://doi.org/10.1016/0378-1135(92)90068-5.
Dhurandhar NV, Israel BA, Kolesar JM, Mayhew G, Cook ME, Atkinson RL. Transmissibility of adenovirus-induced adiposity in a chicken model. Int J Obes Relat Metab Disord. 2001;25:990–6. https://doi.org/10.1038/sj.ijo.0801668.
Whigham LD, Israel BA, Atkinson RL. Adipogenic potential of multiple human adenoviruses in vivo and in vitro in animals. Am J Physiol Regul Integr Comput Physiol. 2006;290:R190–4. https://doi.org/10.1152/ajpregu.00479.2005.
Dhurandhar NV, Whigham LD, Abbott DH, Schultz-Darken NJ, Israel BA, Bradley SM. et al. Human adenovirus ad-36 promotes weight gain in male rhesus and marmoset monkeys. J Nutr. 2002;132:3155–60. https://doi.org/10.1093/jn/131.10.3155.
Kapila M, Khosla P, Dhurandhar NV. Novel short-term effects of adenovirus ad-36 on hamster lipoproteins. Int J Obes Relat Metab Disord. 2004;28:1521–7. https://doi.org/10.1038/sj.ijo.0802710.
Dhurandhar NV, Israel BA, Kolesar JM, Mayhew GF, Cook ME, Atkinson RL. Increased adiposity in animals due to a human virus. Int J Obes Relat Metab Disord. 2000;24:989–96. https://doi.org/10.1038/sj.ijo.0801319.
Krishnapuram R, Dhurandhar EJ, Dubuisson O, Kirk-Ballard H, Bajpeyi S, Butte N, et al. Template to improve glycemic control without reducing adiposity or dietary fat. Am J Physiol Endocrinol Metab. 2011;300:E779–89. https://doi.org/10.1152/ajpendo.00703.2010. May
Dhurandhar NV, Kulkarni PR, Ajinkya SM, Sherikar AA, Atkinson RL. Association of adenovirus infection with human obesity. Obes Res. 1997;5:464–9. https://doi.org/10.1002/j.1550-8528.1997.tb00672.x.
Atkinson RL, Dhurandhar NV, Allison DB, Bowen RL, Israel BA, Albu JB. et al. Human adenovirus‐36 is associated with increased body weight and paradoxical reduction of serum lipids. Int J Obes. 2005;29:281–6. https://doi.org/10.1038/sj.ijo.0802830.
Trovato GM, Castro A, Tonzuso A, Garozzo A, Martines GF, Pirri C. et al. Human obesity relationship with Ad36 adenovirus and insulin resistance. Int J Obes. 2009;33:1402–9. https://doi.org/10.1038/ijo.2009.196.
Trovato GM, Martines GF, Garozzo A, Tonzudo A, Timpanaro R, Pirri C. et al. Ad36 adipogenic adenovirus in human non‐alcoholic fatty liver disease. Liver Int. 2010;30:184–90. https://doi.org/10.1111/j.1478-3231.2009.02127.x.
Almgren M, Atkinson R, He J, Hilding A, Hagman E, Wolk A. et al. Adenovirus‐36 is associated with obesity in children and adults in Sweden as determined by rapid ELISA. PLoS ONE. 2012;7:e41652 https://doi.org/10.1371/journal.pone.0041652.
Na HN, Kim J, Lee HS, Shim KW, Kimm H, Jee SH. et al. Association of human adenovirus-36 in overweight Korean adults. Int J Obes. 2012;36:281–5. https://doi.org/10.1038/ijo.2011.102.
Trovato GM, Martines GF, Trovato FM, Pirri C, Pace P, Garozzo A. et al. Adenovirus‐36 seropositivity enhances effects of nutritional intervention on obesity, bright liver, and insulin resistance. Dig Dis Sci. 2012;57:535–44. https://doi.org/10.1007/s10620-011-1903-8.
Lin WY, Dubuisson O, Rubicz R, Liu N, Allison DB, Curran JE. et al. Long‐term changes in adiposity and glycemic control are associated with past adenovirus infection. Diabetes Care. 2013;36:701–7. https://doi.org/10.2337/dc12-1089.
Almgren M, Atkinson RL, Hilding A, He J, Brismar K, Schalling M. et al. Human adenovirus-36 is uncommon in type 2 diabetes and is associated with increased insulin sensitivity in adults in Sweden. Ann Med. 2014;46:539–46. https://doi.org/10.3109/07853890.2014.935469.
Bil-Lula I, Stapor S, Sochocka M, Wolyniec M, Zatonska K, Ilow R. et al. Infectobesity in the polish population—evaluation of an association between adenoviruses type 5, 31, 36 and human obesity. Int J Virol Mol Biol. 2014;3:1–8. https://doi.org/10.5923/j.ijvmb.20140301.01.
Jiao Y, Mao X, Chang X, Abudureyimu K, Zhang C, Lu J. et al. Adenovirus 36 infection expresses cellular APMI and Visfatin genes in overweight Uygur individuals. Diagn Pathol. 2014;9:83–9. https://doi.org/10.1186/1746-1596-9-83.
Ergin S, Altan E, Pilanci O, Sirekbasan S, Cortuk O, Cizmecigil U. et al. The role of adenovirus 36 as a risk factor in obesity: the first clinical study made in the fatty tissues of adults in Turkey. Microb Pathog. 2015;80:57–62. https://doi.org/10.1016/j.micpath.2015.02.008.
Karamese M, Altoparlak U, Turgut A, Aydogdu S, Karamese SA. The relationship between adenovirus‐36 seropositivity, obesity and metabolic profile in Turkish children and adults. Epidemiol Infect. 2015;143:3550–6. https://doi.org/10.1017/S0950268815000679.
Kocazeybek B, Saribas S, Ergin S. The role of Ad-36 as a risk factor in males with gynecomastia. Med Hypotheses. 2015;85:992–6. https://doi.org/10.1016/j.mehy.2015.08.020.
Sabin MA, Burgner D, Atkinson RL, Pei-Lun LZ, Magnussen CG, Cheung M. et al. Longitudinal investigation of adenovirus 36 seropositivity and human obesity: the cardiovascular risk in young finns study. Int J Obes. 2015;39:1644–50. https://doi.org/10.1038/ijo.2015.108.
Waye MM, Chan JC, Tong PC, Ma R, Chan PK. Association of human adenovirus-36 with diabetes, adiposity, and dyslipidaemia in Hong Kong Chinese. Hong Kong Med J. 2015;21:45–7.
Sapunar J, Fonseca L, Molina, Ortiz E, Barra MI, Reimer C. et al. Adenovirus 36 seropositivity is related to obesity risk, glycemic control, and leptin levels in Chilean subjects. Int J Obes. 2020;44:159–66. https://doi.org/10.1038/s41366-019-0321-4.
Atkinson RL, Lee I, Shin HJ, He J. Human adenovirus-36 antibody status is associated with obesity in children. Int J Pediatr Obes. 2010;5:157–60. https://doi.org/10.3109/17477160903111789.
Gabbert C, Donohue M, Arnold J, Schwimmer JB. Adenovirus 36 and obesity in children and adolescents. Pediatrics. 2010;126:721–6. https://doi.org/10.1542/peds.2009-3362.
Na HN, Hong YM, Kim J, Kim HK, Jo I, Nam JH. Association between human adenovirus-36 and lipid disorders in Korean school children. Int J Obes. 2010;34:89–93. https://doi.org/10.1038/ijo.2009.207.
Tosh AK, Broy-Aschenbrenner A, El Khatib J, Ge B. Adenovirus-36 antibody status & BMI comparison among obese Missouri adolescents. Mol Med. 2012;109:402–3. PMCID: PMC6179760
Aldhoon-Hainerova I, Zamrazilova H, Atkinson RL, Dušátková L, Sedláčková B, Hlavatý P. et al. Clinical and laboratory characteristics of 1179 Czech adolescents evaluated for antibodies to human adenovirus 36. Int J Obes. 2014;38:285–91. https://doi.org/10.1038/ijo.2013.72.
Laing EM, Tripp RA, Pollock NK, Baile CA, Della-Fera MA, Rayalam S. et al. Adenovirus 36, adiposity, and bone strength in late-adolescent females. J Bone Miner Res. 2013;28:489–96. https://doi.org/10.1002/jbmr.1776.
Parra-Rojas I, Del Moral-Hernandez O, Salgado-Bernabe AB, Guzman-Guzman IP, Salgado-Goytia L, Munoz-Valle JF. Adenovirus 36 seropositivity and its relation with obesity and metabolic profile in children. Int J Endocrinol. 2013;2013:463194 https://doi.org/10.1155/2013/463194.
Vander Wal JS, Huelsing J, Dubuisson O, Dhurandhar NV. An observational study of the association between adenovirus 36 antibody status and weight loss among youth. Obes Facts. 2013;6:269–78. https://doi.org/10.1159/000353109.
Cakmakliogullari EK, Sanlidag T, Ersoy B, Akcali S, Var A, Cicek C. Are human adenovirus-5 and 36 associated with obesity in children?. J Investig Med. 2014;62:821–4. https://doi.org/10.2310/JIM.0000000000000084.
Dusatkova L, Zamrazilova H, Aldhoon-Hainerova I, Atkinson RL, Sedlackova B, Lee ZP, et al. Association of adenovirus 36 infection with obesity-related gene variants in adolescents. Physiol Res 2015;64:S197–S202. https://doi.org/10.33549/physiolres.933131. Suppl 2
Park S, Kim J, Shin HJ, Hong YM, Sheen YH, Park HL. et al. Tracking study about adenovirus 36 infection: increase of adiposity. J Microbiol Biotechnol. 2015;25:2169–72. https://doi.org/10.4014/jmb.1509.09003.
Zamrazilová H, Aldhoon-Hainerová I, Atkinson RL, Dušátková L, Sedláčková B, Lee ZP. et al. Adenovirus 36 infection: a role in dietary intake and response to inpatient weight management in obese girls. Int J Obes. 2015;39:1757–60. https://doi.org/10.1038/ijo.2015.167.
Kocazeybek B, Dinc HO, Ergin S. Evaluation of adenovirus-36 (Ad-36) antibody seropositivity and adipokine levels in obese children. Microb Pathog. 2017;108:27–31. https://doi.org/10.1016/j.micpath.2017.04.034.
Tosh AK, Wasserman MG, McLeay li MT, Tepe SK. Human adenovirus-36 seropositivity and obesity among Midwestern US adolescents. Int J Adolesc Med Health. 2017. https://doi.org/10.1515/ijamh-2017-0126.
Lavoy EC, Arlinghaus KR, Rooney BV, Gupta P, Atkinson R, Johnston CA. High adenovirus 36 seroprevalence among a population of Hispanic American youth. Int J Adolesc Med Health. 2018. https://doi.org/10.1515/ijamh-2018-0110.
Broderick MP, Hansen CJ, Irvine M, Metzgar D, Campbell K, Baker C. et al. Adenovirus 36 seropositivity is strongly associated with race and gender, but not obesity, among US military personnel. Int J Obes. 2010;34:302–8. https://doi.org/10.1038/ijo.2009.224.
Goossens VJ, de Jager SA, Grauls GE, Gielen M, Vlietinck RF, Derom CA. et al. Lack of evidence for the role of human adenovirus-36 in obesity in a European cohort. Obesity. 2011;19:220–1. https://doi.org/10.1038/oby.2009.452.
Voss JD, Burnett DG, Olsen CH, Haverkos HW, Atkinson RL. Adenovirus 36 Antibodies associated with clinical diagnosis of overweight/obesity but not BMI gain: a military cohort study. J Clin Endocrinol Metab.2014;99:E1708–12. https://doi.org/10.1210/jc.2014-1863.
Ponterio E, Cangemi R, Mariani S, Casella G, De Cesare A, Trovato FM. et al. Adenovirus 36 DNA in human adipose tissue. Int J Obes. 2015;39:1761–4.https://doi.org/10.3390/v7072787.
Zhou Y, Pan Q, Wang X, Zhang L, Xiao F, Guo L. The relationship between human adenovirus 36 and obesity in Chinese Han population. Biosci Rep. 2018; 38. https://doi.org/10.1042/BSR20180553.
Berger PK, Pollock NK, Laing EM, Warden SJ, Hill-Gallant KM, Hausman DB. et al. Association of adenovirus 36 infection with adiposity and inflammatory-related markers in children. J Clin Endocrinol Metab. 2014;99:3240–6. https://doi.org/10.1210/jc.2014-1780.
Dhurandhar NV. A framework for identification of infections that contribute to human obesity. Lancet Infect. Dis. 2011;11:963–69.https://doi.org/10.1016/S1473-3099(11)70274-2.
Hegde V, Dhurandhar NV. Microbes and obesity: interrelationship between infection, adipose tissue and the immune system. Clin Microbiol Infect. 2013;19:314–20.https://doi.org/10.1111/1469-0691.12157.
Rathod MA, Rogers PM, Vangipuram SD, McAllister EJ, Dhurandhar NV. Adipogenic cascade can be induced without adipogenic media by a human adenovirus. Obesity. 2009;17:657–64.https://doi.org/10.1038/oby.2008.630.
Ponterio E, Gnessi L. Adenovirus 36 and obesity: an overview. Viruses. 2015;7:3719–40. https://doi.org/10.3390/v7072787
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1 https://doi.org/10.1186/2046-4053-4-1
Kolesar JM, Miller JA, Dhurandhar NV, Atkinson RL. Direct quantification of AD36 adenovirus DNA by capillary electrophoresis with laser-induced fluorescence. J Chromatogr B Biomed Sci Appl. 2000;744:1–8.
Yeung R, Eshaghi A, Lombos E, Blair J, Mazzulli T, Burton L, et al. Characterization of culture-positive adenovirus serotypes from respiratory specimens in Toronto, Ontario, Canada: September 2007–June 2008. Virol J. 2009;6:11.
Chappell CL, Dickerson M, Day RS, Dubuisson O, Dhurandhar NV. Adenovirus 36 antibody detection: Improving the standard serum neutralization assay. J Virol Methods. 2017;239:69–74.
Dubuisson O, Day RS, Dhurandhar NV. Accurate identification of neutralizing antibodies to adenovirus Ad36—a putative contributor of obesity in humans. J Diabet Compl. 2015;29:83–7.
Nam JH, Na HN, Atkinson RL, Dhurandhar NV. Genomic stability of adipogenic human adenovirus 36. Int J Obes. 2014;38:321–4.
Atkinson RL. Adenovirus and obesity. Chapter 9. In. Haslam DW, Sharma AM, Roux CW. Controversies in obesity. London: Springer-Verlag, 2014. p.75–78.
Lessan N, Saradalekshmi KR, Alkaf B, Majeed M, Barakat MT, Lee ZPL. et al. Obesity and diabetes in an arab population: role of adenovirus 36 infection. Sci Rep. 2020;10:8107https://doi.org/10.1038/s41598-020-65008-x.
Yamada T, Hara K, Kadowaki T. Association of adenovirus 36 infection with obesity and metabolic markers in humans: a meta-analysis of observational studies. PLoS ONE. 2012;7:e42031https://doi.org/10.1371/journal.pone.0042031.
Shang Q, Wang H, Song Y, Wei L, Lavebratt C, Zhang F. et al. Serological data analyses show that adenovirus 36 infection is associated with obesity: a meta-analysis involving 5739 subjects. Obesity. 2014;22:895–900.https://doi.org/10.1002/oby.20533.
Xu MY, Cao B, Wang DF, Guo JH, Chen KL, Shi M. et al. Human adenovirus 36 infection increased the risk of obesity: a meta-analysis update. Medicine. 2015;94:e2357https://doi.org/10.1097/MD.0000000000002357.
Akheruzzaman M, Hegde V, Dhurandhar NV. Twenty-five years of research about adipogenic adenoviruses: a systematic review. Obes Rev. 2019;20:499–509.https://doi.org/10.1111/obr.12808. Apr.
Rogers PM, Fusinski KA, Rathod MA, Loiler SA, Pasarica M, Shaw MK. et al. Human adenovirus Ad-36 induces adipogenesis via its E4 orf-1 gene. Int J Obes. 2008;32:397–406.https://doi.org/10.1038/sj.ijo.0803748.
Thai M, Graham NA, Braas D, Nehil M, Komisopoulou E, Kurdistani SK. et al. Adenovirus E4ORF1-induced MYC activation promotes host cell anabolic glucose metabolism and virus replication. Cell Metab. 2014;19:694–701.https://doi.org/10.1016/j.cmet.2014.03.009.
Dhurandhar NV. Insulin sparing action of adenovirus 36 and its E4orf1 protein. J Diabet Compl. 2013;27:191–9.https://doi.org/10.1016/j.jdiacomp.2012.09.006.
Kusminski CM, Gallardo-Montejano VI, Wang ZV, Hegde V, Bickel PE, Dhurandhar NV. et al. E4orf1 induction in adipose tissue promotes insulin-independent signaling in the adipocyte. Mol Metab. 2015;4:653–64.https://doi.org/10.1016/j.molmet.2015.07.004.
Vangipuram SD, Yu M, Tian J, Stanhope KL, Pasarica M, Havel PJ. et al. Adipogenic human adenovirus-36 reduces leptin expression and secretion and increases glucose uptake by fat cells. Int J Obes. 2007;31:87–96.https://doi.org/10.1038/sj.ijo.0803366.
Rogers PM, Mashtalir N, Rathod MA, Dubuisson O, Wang Z, Dasuri K. et al. Metabolically favorable remodeling of human adipose tissue by human adenovirus type 36. Diabetes. 2008;57:2321–31.https://doi.org/10.2337/db07-1311.
Pasarica M, Mashtalir N, McAllister EJ, Kilroy GE, Koska J, Permana P. et al. Adipogenic human adenovirus ad-36 induces commitment, differentiation, and lipid accumulation in human adipose-derived stem cells. Stem Cells. 2008;26:969–78.https://doi.org/10.1634/stemcells.2007-0868.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
da Silva Fernandes, J., Schuelter-Trevisol, F., Cancelier, A.C.L. et al. Adenovirus 36 prevalence and association with human obesity: a systematic review. Int J Obes 45, 1342–1356 (2021). https://doi.org/10.1038/s41366-021-00805-6
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41366-021-00805-6
This article is cited by
-
Pan-serological antibodies and liver cancer risk: a nested case-control analysis
Scientific Reports (2025)
-
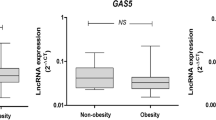
Adenovirus 36 seropositivity is related to the expression of anti-adipogenic lncRNAs GAS5 and MEG3 in adipose tissue obtained from subjects with obesity
International Journal of Obesity (2024)
-
The immunology of sickness metabolism
Cellular & Molecular Immunology (2024)