Abstract
Introduction
Glucagon-like peptide-1 receptor agonists (GLP-1ra) are increasingly used in treating type 2 diabetes and obesity. Exendin-4 (Ex-4), a long acting GLP-1ra, was previously reported to decrease oxidative stress in hepatocytes, adipocytes and skeletal muscle cells in obese nondiabetic fa/fa Zucker rats (ZFR), thereby improving insulin resistance.
Aim
We aimed first to identify Ex-4-induced changes in the transcriptome of skeletal muscle cells in ZFR.
Results
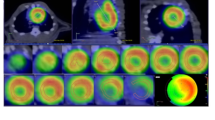
Ontology analysis of differentially expressed genes (DEGs) in ZFR versus lean animals (LR) showed that the extracellular matrix (ECM) is the first most affected cellular compartment, followed by myofibrils and endoplasmic reticulum (ER). Interestingly, among 15 genes regulated in ZFR versus LR, 14 of them were inversely regulated by Ex-4, as further confirmed by RT-qPCR. Picro-Sirius red histological staining showed that decreased ECM fiber area in ZFR is partially restored by Ex-4. Ontology analysis of the myofibril compartment revealed that decreased muscle contractile function in ZFR is partially restored by Ex-4, as confirmed by Phalloidin histological staining that showed a partial restoration by Ex-4 of altered contractile apparatus in ZFR. Ontology analysis of ER DEGs in ZFR versus LR showed that some of them are related to the AMP-activated protein kinase (AMPK) signaling pathway. Phosphorylated AMPK levels were strongly increased in Ex-4-treated ZFR.
Conclusion
Altogether, our results suggest that GLP-1ra strongly restructure ECM and reinforce contractile capabilities in ZFR, while optimizing the cellular metabolism through AMPK.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
Data available within the article or its Supplementary Materials. RNAseq row data available on request from the authors.
References
Lyseng-Williamson KA. Glucagon-like peptide-1 receptor analogues in type 2 diabetes: their use and differential features. Clin Drug Investig. 2019;39:805–19.
Ahren B. Glucagon-like peptide-1 receptor agonists for type 2 diabetes: a rational drug development. J Diabetes Investig. 2019;10:196–201.
Muller TD, Finan B, Bloom SR, D’Alessio D, Drucker DJ, Flatt PR, et al. Glucagon-like peptide 1 (GLP-1). Mol Metab. 2019;30:72–130.
Nauck MA, Meier JJ. Management of endocrine disease: are all GLP-1 agonists equal in the treatment of type 2 diabetes? Eur J Endocrinol. 2019;181:R211–34.
American Diabetes Association. 9. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes-2020. Diabetes Care. 2020;43 Suppl 1:S98–110.
Colin IM, Colin H, Dufour I, Gielen CE, Many MC, Saey J, et al. Extrapancreatic effects of incretin hormones: evidence for weight-independent changes in morphological aspects and oxidative status in insulin-sensitive organs of the obese nondiabetic Zucker rat (ZFR). Physiol Rep. 2016;4:e12886.
Trapnell C, Roberts A, Goff L, Pertea G, Kim D, Kelley DR, et al. Differential gene and transcript expression analysis of RNA-seq experiments with TopHat and Cufflinks. Nat Protoc. 2012;7:562–78.
Chen J, Bardes EE, Aronow BJ, Jegga AG. ToppGene Suite for gene list enrichment analysis and candidate gene prioritization. Nucleic Acids Res. 2009;37:W305–11.
Bonnans C, Chou J, Werb Z. Remodelling the extracellular matrix in development and disease. Nat Rev Mol Cell Biol. 2014;15:786–801.
Kagan HM, Li W. Lysyl oxidase: properties, specificity, and biological roles inside and outside of the cell. J Cell Biochem. 2003;88:660–72.
Molnar J, Fong KS, He QP, Hayashi K, Kim Y, Fong SF, et al. Structural and functional diversity of lysyl oxidase and the LOX-like proteins. Biochim Biophys Acta. 2003;1647:220–4.
Blackburn PR, Xu Z, Tumelty KE, Zhao RW, Monis WJ, Harris KG, et al. Bi-allelic alterations in AEBP1 lead to defective collagen assembly and connective tissue structure resulting in a variant of Ehlers-Danlos syndrome. Am J Hum Genet. 2018;102:696–705.
Kadomatsu T, Endo M, Miyata K, Oike Y. Diverse roles of ANGPTL2 in physiology and pathophysiology. Trends Endocrinol Metab. 2014;25:245–54.
Ouchi N, Oshima Y, Ohashi K, Higuchi A, Ikegami C, Izumiya Y, et al. Follistatin-like 1, a secreted muscle protein, promotes endothelial cell function and revascularization in ischemic tissue through a nitric-oxide synthase-dependent mechanism. J Biol Chem. 2008;283:32802–11.
Gorgens SW, Raschke S, Holven KB, Jensen J, Eckardt K, Eckel J. Regulation of follistatin-like protein 1 expression and secretion in primary human skeletal muscle cells. Arch Physiol Biochem. 2013;119:75–80.
Tripathi G, Salih DA, Drozd AC, Cosgrove RA, Cobb LJ, Pell JM. IGF-independent effects of insulin-like growth factor binding protein-5 (Igfbp5) in vivo. FASEB J. 2009;23:2616–26.
Dees C, Distler JH. Canonical Wnt signalling as a key regulator of fibrogenesis—implications for targeted therapies? Exp Dermatol. 2013;22:710–3.
Sanchez EJ, Munske GR, Criswell A, Milting H, Dunker AK, Kang C. Phosphorylation of human calsequestrin: implications for calcium regulation. Mol Cell Biochem. 2011;353:195–204.
Bodine SC, Baehr LM. Skeletal muscle atrophy and the E3 ubiquitin ligases MuRF1 and MAFbx/atrogin-1. Am J Physiol Endocrinol Metab. 2014;307:E469–84.
Rashid MM, Runci A, Polletta L, Carnevale I, Morgante E, Foglio E, et al. Muscle LIM protein/CSRP3: a mechanosensor with a role in autophagy. Cell Death Discov. 2015;1:15014.
Stamatikos AD, Paton CM. Role of stearoyl-CoA desaturase-1 in skeletal muscle function and metabolism. Am J Physiol Endocrinol Metab. 2013;305:E767–75.
Park SW, Zhou Y, Lee J, Lu A, Sun C, Chung J, et al. The regulatory subunits of PI3K, p85alpha and p85beta, interact with XBP-1 and increase its nuclear translocation. Nat Med. 2010;16:429–37.
Delaigle AM, Senou M, Guiot Y, Many MC, Brichard SM. Induction of adiponectin in skeletal muscle of type 2 diabetic mice: In vivo and in vitro studies. Diabetologia. 2006;49:1311–23.
Li F, Li Y, Duan Y, Hu CA, Tang Y, Yin Y. Myokines and adipokines: Involvement in the crosstalk between skeletal muscle and adipose tissue. Cytokine Growth Factor Rev. 2017;33:73–82.
Bosma M. Lipid droplet dynamics in skeletal muscle. Exp Cell Res. 2016;340:180–6.
Gemmink A, Goodpaster BH, Schrauwen P, Hesselink MKC. Intramyocellular lipid droplets and insulin sensitivity, the human perspective. Biochim Biophys Acta Mol Cell Biol Lipids. 2017;1862:1242–9.
Khor VK, Shen WJ, Kraemer FB. Lipid droplet metabolism. Curr Opin Clin Nutr Metab Care. 2013;16:632–7.
Roden M, Shulman GI. The integrative biology of type 2 diabetes. Nature. 2019;576:51–60.
Petersen MC, Shulman GI. Mechanisms of insulin action and insulin resistance. Physiol Rev. 2018;98:2133–23.
Wasserman DH, Kang L, Ayala JE, Fueger PT, Lee-Young RS. The physiological regulation of glucose flux into muscle in vivo. J Exp Biol. 2011;214:254–62.
Shulman GI. Ectopic fat in insulin resistance, dyslipidemia, and cardiometabolic disease. N Engl J Med. 2014;371:1131–41.
Korach-Andre M, Gounarides J, Deacon R, Beil M, Sun D, Gao J, et al. Age and muscle-type modulated role of intramyocellular lipids in the progression of insulin resistance in nondiabetic Zucker rats. Metabolism. 2005;54:522–8.
Machann J, Haring H, Schick F, Stumvoll M. Intramyocellular lipids and insulin resistance. Diabetes Obes Metab. 2004;6:239–48.
Kucera O, Cervinkova Z. Experimental models of non-alcoholic fatty liver disease in rats. World J Gastroenterol. 2014;20:8364–76.
Abu-Hamdah R, Rabiee A, Meneilly GS, Shannon RP, Andersen DK, Elahi D. Clinical review: The extrapancreatic effects of glucagon-like peptide-1 and related peptides. J Clin Endocrinol Metab. 2009;94:1843–52.
Wu H, Sui C, Xu H, Xia F, Zhai H, Zhang H, et al. The GLP-1 analogue exenatide improves hepatic and muscle insulin sensitivity in diabetic rats: tracer studies in the basal state and during hyperinsulinemic-euglycemic clamp. J Diabetes Res. 2014;2014:524517.
Rowlands J, Heng J, Newsholme P, Carlessi R. Pleiotropic effects of GLP-1 and analogs on cell signaling, metabolism, and function. Front Endocrinol. 2018;9:672.
Koska J, Lopez L, D’Souza K, Osredkar T, Deer J, Kurtz J, et al. Effect of liraglutide on dietary lipid-induced insulin resistance in humans. Diabetes Obes Metab. 2018;20:69–76.
Fiorentino TV, Casiraghi F, Davalli AM, Finzi G, La RS, Higgins PB, et al. Exenatide regulates pancreatic islet integrity and insulin sensitivity in the nonhuman primate baboon Papio hamadryas. JCI Insight. 2019;4:e93091.
Choung JS, Lee YS, Jun HS. Exendin-4 increases oxygen consumption and thermogenic gene expression in muscle cells. J Mol Endocrinol. 2017;58:79–90.
Xu F, Cao H, Chen Z, Gu H, Guo W, Lin B, et al. Short-term GLP-1 receptor agonist exenatide ameliorates intramyocellular lipid deposition without weight loss in ob/ob mice. Int J Obes. 2020;44:937-947.
Andreozzi F, Raciti GA, Nigro C, Mannino GC, Procopio T, Davalli AM, et al. The GLP-1 receptor agonists exenatide and liraglutide activate Glucose transport by an AMPK-dependent mechanism. J Transl Med. 2016;14:229.
Yu P, Xu X, Zhang J, Xia X, Xu F, Weng J, et al. Liraglutide attenuates nonalcoholic fatty liver disease through adjusting lipid metabolism via SHP1/AMPK signaling pathway. Int J Endocrinol. 2019;2019:1567095.
Gillies AR, Lieber RL. Structure and function of the skeletal muscle extracellular matrix. Muscle Nerve. 2011;44:318–31.
Lund DK, Cornelison DD. Enter the matrix: shape, signal and superhighway. FEBS J. 2013;280:4089–99.
Hyldahl RD, Nelson B, Xin L, Welling T, Groscost L, Hubal MJ, et al. Extracellular matrix remodeling and its contribution to protective adaptation following lengthening contractions in human muscle. FASEB J. 2015;29:2894–904.
Grzelkowska-Kowalczyk K. The importance of extracellular matrix in skeletal muscle development and function. In: Travascio F, editor. Composition and function of the extracellular matrix in the human body. InTech; 2016. p. 3–24. https://www.intechopen.com/books/5225. https://doi.org/10.5772/61601
Berria R, Wang L, Richardson DK, Finlayson J, Belfort R, Pratipanawatr T, et al. Increased collagen content in insulin-resistant skeletal muscle. Am J Physiol Endocrinol Metab. 2006;290:E560–5.
Coletta DK, Mandarino LJ. Mitochondrial dysfunction and insulin resistance from the outside in: extracellular matrix, the cytoskeleton, and mitochondria. Am J Physiol Endocrinol Metab. 2011;301:E749–55.
Martinez-Huenchullan S, McLennan SV, Verhoeven A, Twigg SM, Tam CS. The emerging role of skeletal muscle extracellular matrix remodelling in obesity and exercise. Obes Rev. 2017;18:776–90.
Datta R, Podolsky MJ, Atabai K. Fat fibrosis: friend or foe? JCI Insight. 2018;3:e122289.
Kang L, Ayala JE, Lee-Young RS, Zhang Z, James FD, Neufer PD, et al. Diet-induced muscle insulin resistance is associated with extracellular matrix remodeling and interaction with integrin alpha2beta1 in mice. Diabetes. 2011;60:416–26.
Pincu Y, Linden MA, Zou K, Baynard T, Boppart MD. The effects of high fat diet and moderate exercise on TGFbeta1 and collagen deposition in mouse skeletal muscle. Cytokine. 2015;73:23–9.
Tam CS, Power JE, Markovic TP, Yee C, Morsch M, McLennan SV, et al. The effects of high-fat feeding on physical function and skeletal muscle extracellular matrix. Nutr Diabetes. 2015;5:e187.
He D, Bolstad G, Brubakk A, Medbo JI. Muscle fibre type and dimension in genetically obese and lean Zucker rats. Acta Physiol Scand. 1995;155/1:1–7.
Cao HY, Xu F, Chen ZL, Lin BS, Zheng XB, Yuan SH, et al. Effect of exendin-4 on lipid deposition in skeletal muscle of diet-induced obese mice and its underlying mechanism. Zhonghua Yi Xue Za Zhi. 2017;97:131–6.
Wu H, Sui C, Xia F, Zhai H, Zhang H, Xu H, et al. Effects of exenatide therapy on insulin resistance in the skeletal muscles of high-fat diet and low-dose streptozotocin-induced diabetic rats. Endocr Res. 2016;41:1–7.
Huang H, Aminian A, Hassan M, Dan O, Axelrod CL, Schauer PR, et al. Gastric bypass surgery improves the skeletal muscle ceramide/S1P ratio and upregulates the AMPK/ SIRT1/ PGC-1alpha pathway in Zucker diabetic fatty rats. Obes Surg. 2019;29:2158–65.
Acknowledgements
Authors thanks Mrs Catherine Rasse (support en méthodologie et calcul statistique, Louvain institute of data analysis and modeling in economics and statistics, Université catholique de Louvain (UCLouvain)) for her help in statistical analysis.
Funding
This study was supported by a grant from the “Fonds de la Recherche Scientifique dans le Hainaut 2018”, and from the King Baudouin Foundation “Amelie G488730 fund”.
Author information
Authors and Affiliations
Contributions
IMC conceived and designed the study, participated to results interpretation, and wrote the manuscript. BK participated to results interpretation and critical revision of the manuscript. ACG participated to conception and design of the study, performed experiments, data collection, data analysis, and figures design, contributed to manuscript. All authors approved the final version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Colin, I.M., Knoops, B. & Gérard, AC. Incretin-induced changes in the transcriptome of skeletal muscles of fa/fa Zucker rat (ZFR) with obesity, without diabetes. Int J Obes 46, 1311–1318 (2022). https://doi.org/10.1038/s41366-022-01114-2
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41366-022-01114-2