Abstract
Background
Obesity is major cause of heart failure (HF), but it is related with a better prognosis among the elderly. Therefore, we aimed to examine whether metabolically healthy obesity (MHO) in late life increases HF risk and is reflected in impaired left ventricular (LV) function.
Methods
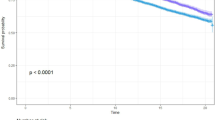
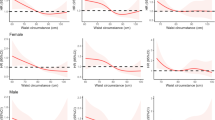
The participants were grouped into four metabolic phenotypes based on obesity and metabolic status: metabolically healthy non-obesity (MHN), MHO, metabolically unhealthy non-obesity (MUN), metabolically unhealthy obesity (MUO). Association of metabolic phenotypes with LV function was evaluated using multiple linear regression models. And association between metabolic phenotypes and risk of HF was assessed using multivariable logistic regression models. In addition, we validated the association of metabolic phenotypes and HF risk in a separate longitudinal cohort.
Results
In the primary cohort of 6335 participant, there were 434 participants diagnosed with HF. Compared to MHN participants, the risk of HF was higher among older individuals with MUN (OR = 1.51 [95% CI: 1.14–1.99]) and MUO (OR = 2.01 [95% CI: 1.39–2.91]), but not older individuals with MHO (OR = 0.86 [95% CI: 0.30–2.43). Regarding to LV function, worse LV diastolic function was noted among MUN and MUO individuals rather than MHO individuals. Older adults with MHO were also not associated with risk of HF in the validation cohort.
Conclusion
Among older individuals, the metabolic health status might modify the association of obesity with risk of HF and LV diastolic dysfunction. Worse LV diastolic function and higher risk of HF were just noted in individuals with MUO, but not in those with MHO.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The data used and/or analyzed in this study are available to all researchers upon reasonable request.
References
Tsao CW, Aday AW, Almarzooq ZI, Alonso A, Beaton AZ, Bittencourt MS, et al. Heart Disease and Stroke Statistics-2022 Update: A Report From the American Heart Association. Circulation. 2022;145:e153–e639.
Blecker S, Paul M, Taksler G, Ogedegbe G, Katz S. Heart failure–associated hospitalizations in the United States. J Am Coll Cardiol. 2013;61:1259–67.
Tromp J, Paniagua SMA, Lau ES, Allen NB, Blaha MJ, Gansevoort RT, et al. Age dependent associations of risk factors with heart failure: pooled population based cohort study. Bmj. 2021;372:n461.
Ryg J, Anru PL, Engberg H, Jorgensen MG, Masud T, Christensen K, et al. Association of Body Mass Index With All-Cause Mortality in Acutely Hospitalized Older Patients. J Am Med Dir Assoc. 2022;23:507–13.e1.
Fonseca G, von Haehling S. The fatter, the better in old age: the current understanding of a difficult relationship. Curr Opin Clin Nutr Metab Care. 2022;25:1–6.
Amankwaa I, Nelson K, Rook H, Hales C. Association between body mass index, multi-morbidity and activities of daily living among New Zealand nursing home older adults: a retrospective analysis of nationwide InterRAI data. BMC Geriatrics. 2022;22:62.
Piché ME, Tchernof A, Després JP. Obesity Phenotypes, Diabetes, and Cardiovascular Diseases. Circ Res. 2020;126:1477–500.
Després JP. Body fat distribution and risk of cardiovascular disease: an update. Circulation. 2012;126:1301–13.
Lu Y, Hajifathalian K, Ezzati M, Woodward M, Rimm EB, Danaei G. Metabolic mediators of the effects of body-mass index, overweight, and obesity on coronary heart disease and stroke: a pooled analysis of 97 prospective cohorts with 1·8 million participants. Lancet. 2014;383:970–83.
Brandão I, Martins MJ, Monteiro R. Metabolically Healthy Obesity-Heterogeneity in Definitions and Unconventional Factors. Metabolites. 2020;10:48.
Stefan N, Häring HU, Hu FB, Schulze MB. Metabolically healthy obesity: epidemiology, mechanisms, and clinical implications. Lancet Diabetes Endocrinol. 2013;1:152–62.
Chen C. The guidelines for prevention and control of overweight and obesity in Chinese adults. Biomed Environ Sci. 2004;17:1–36.
Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA. 2001;285:2486–97.
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–5.
Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep. Ser. 2000;894:1–253.
The Atherosclerosis Risk in Communities (ARIC) Study: design and objectives. The ARIC investigators. Am J Epidemiol. 1989;129:687–702.
Mørkedal B, Vatten LJ, Romundstad PR, Laugsand LE, Janszky I. Risk of myocardial infarction and heart failure among metabolically healthy but obese individuals: HUNT (Nord-Trøndelag Health Study), Norway. J Am Coll Cardiol. 2014;63:1071–8.
Caleyachetty R, Thomas GN, Toulis KA, Mohammed N, Gokhale KM, Balachandran K, et al. Metabolically Healthy Obese and Incident Cardiovascular Disease Events Among 3.5 Million Men and Women. J Am Coll Cardiol. 2017;70:1429–37.
Patel KV, Segar MW, Lavie CJ, Kondamudi N, Neeland IJ, Almandoz JP, et al. Diabetes Status Modifies the Association Between Different Measures of Obesity and Heart Failure Risk Among Older Adults: A Pooled Analysis of Community-Based NHLBI Cohorts. Circulation. 2022;145:268–78.
Wang YC, Liang CS, Gopal DM, Ayalon N, Donohue C, Santhanakrishnan R, et al. Preclinical Systolic and Diastolic Dysfunctions in Metabolically Healthy and Unhealthy Obese Individuals. Circulation Heart Fail. 2015;8:897–904.
Dobson R, Burgess MI, Sprung VS, Irwin A, Hamer M, Jones J, et al. Metabolically healthy and unhealthy obesity: differential effects on myocardial function according to metabolic syndrome, rather than obesity. Int J Obes. 2016;40:153–61.
Wang Y, Liang J, Zheng S, He A, Chen C, Zhao X, et al. Combined associations of obesity and metabolic health with subclinical left ventricular dysfunctions: Danyang study. ESC heart Fail. 2021;8:3058–69.
Russo C, Jin Z, Homma S, Rundek T, Elkind MS, Sacco RL, et al. Effect of obesity and overweight on left ventricular diastolic function: a community-based study in an elderly cohort. J Am Coll Cardiol. 2011;57:1368–74.
Russo C, Sera F, Jin Z, Palmieri V, Homma S, Rundek T, et al. Abdominal adiposity, general obesity, and subclinical systolic dysfunction in the elderly: A population-based cohort study. Eur J Heart Fail. 2016;18:537–44.
Yeboah J, Rodriguez CJ, Stacey B, Lima JA, Liu S, Carr JJ, et al. Prognosis of individuals with asymptomatic left ventricular systolic dysfunction in the multi-ethnic study of atherosclerosis (MESA). Circulation. 2012;126:2713–9.
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur heart J. 2021;42:3599–726.
Miller SL, Wolfe RR. The danger of weight loss in the elderly. J Nutr Health Aging. 2008;12:487–91.
Bozkurt B. It Is Time to Screen for Heart Failure: Why and How? JACC Heart Fail. 2022;10:598–600.
Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022;145:e895–e1032.
Acknowledgements
We thank all the staff and participants of the RED-CARPET study and ARIC study for their contributions.
Funding
This study was supported by the National Natural Science Foundation of China (81870195, 82070384 to XL; 81900329 to YG), Guangdong Basic and Applied Basic Research Foundation (2019A1515011582, 2021A1515011668 to XL; 2019A1515011098, 2022A1515010416 to YG; 2022A1515111181 to ML; 2021A1515110266 to ZX) and China Postdoctoral Science Foundation (2022M723635 to ML; 2021TQ0386, 2021M703738 to ZX).
Author information
Authors and Affiliations
Contributions
XL, XZ, PW and ML conceived and designed the study. XL, XZ, PW, ML, SZ, YG, ZX, YH, XC, LH, ZC and YZ contributed to the acquisition, analysis and interpretation of the data. PW and ML were responsible for writing the manuscript. All authors contributed to revising the manuscript draft for important intellectual content and approved the final submitted manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was followed the principles of the Declaration of Helsinki and was approved by the ethics committee (ChiCTR2000039901 and NCT00005131). Written informed consent was obtained from all participants prior to data collection.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, P., Liu, M., Zhang, S. et al. Association of metabolically healthy obesity with risk of heart failure and left ventricular dysfunction among older adults. Int J Obes 48, 1587–1592 (2024). https://doi.org/10.1038/s41366-024-01587-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41366-024-01587-3