Abstract
Objectives
To examine individual, family, and program characteristics associated with changes in anthropometric and cardiometabolic health indicators in children with overweight or obesity after participating in multidisciplinary obesity management for 12 months.
Methods
Participants included children 2–17 years old with overweight or obesity enrolled in the CANadian Pediatric Weight Management Registry (CANPWR). Multiple linear regression analyses were conducted to investigate the associations between individual, family, and program characteristics and changes in anthropometry (WHO BMI z-score) and cardiometabolic health indicators (systolic and diastolic blood pressure; fasting and 2-h glucose post-oral glucose tolerance test (OGTT); high density lipoprotein- (HDL) and non-HDL cholesterol and fasting triglycerides).
Results
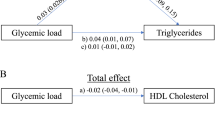
BMI z-score data were available from 1065/1286 (82.8%) at 6-months post-baseline and 893/1286 (69.4%) at 12-months post-baseline. At 6-months, BMI z-score decreased relative to baseline (mean difference (MD) [95% confidence interval (CI)] = −0.08 [−0.10 to −0.06]; p < 0.001). BMI z-score (MD [95% CI] = −0.08 [−0.13 to −0.04); p = 0.001) and fasting triglycerides (MD [95% CI] = −0.07 [−0.13 to −0.02); p = 0.011) decreased at 12 months from baseline. Older age at baseline (estimated β = 0.025; 95% CI [0.006, 0.042], p = 0.007) and female sex (estimated β = 0.241; 95% CI [0.108, 0.329], p < 0.001) were associated with a worsened Δ BMI z-score at 12 months, while total hours with mental health provider (estimated β = −0.015; 95% CI [−0.030, −0.001], p = 0.049) was associated with an improved Δ BMI z-score at 12 months. Hours with an exercise counselor (estimated β = 0.023; 95% CI [0.008, 0.039], p = 0.003) were associated with improved HDL, while hours with a registered dietitian (estimated β = −0.026; 95% CI [−0.051, −0.001], p = 0.044) were associated with improved non-HDL cholesterol.
Conclusions
Male sex and hours spent with a mental health provider, exercise counselor, and registered dietitian were related to significant improvements in several anthropometric and cardiometabolic health indicators at 12 months post-baseline.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available due to the risk of individual participant privacy being compromised, but a deidentified dataset are available from the corresponding author on reasonable request.
References
World Health Organization. Obesity and overweight. 2021. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
Goran MI, Ball GDC, Cruz ML. Obesity and risk of type 2 diabetes and cardiovascular disease in children and adolescents. J Clin Endocrinol Metab. 2003;88:1417–27.
Jebeile H, Kelly AS, O'Malley G, Baur LA. Obesity in children and adolescents: epidemiology, causes, assessment, and management. Lancet Diabetes Endocrinol. 2022;10:351–65.
Romanelli R, Cecchi N, Carbone MG, Dinardo M, Gaudino G, Miraglia del Giudice E, et al. Pediatric obesity: prevention is better than care. Ital J Pediatr. 2020;46:1–7.
Foster BA, Farragher J, Parker P, Sosa ET. Treatment interventions for early childhood obesity: a systematic review. Acad Pediatr. 2015;15:353–61.
Nordlund S, McPhee PG, Gabarin R, Deacon C, Mbuagbaw L, Morrison KM. Effect of obesity treatment interventions in preschool children aged 2–6 years: a systematic review and meta-analysis. BMJ Open. 2022;12:e053523.
Al‐Khudairy L, Loveman E, Colquitt JL, Mead E, Johnson RE, Fraser H, et al. Diet, physical activity and behavioural interventions for the treatment of overweight or obese adolescents aged 12 to 17 years. Cochrane Database Syst Rev. 2017;6:CD012691.
Mead E, Brown T, Rees K, Azevedo LB, Whittaker V, Jones D, et al. Diet, physical activity and behavioural interventions for the treatment of overweight or obese children from the age of 6 to 11 years. Cochrane Database Syst Rev. 2017;6:CD012651.
Smith JD, George SM, Prado G. Family-centered positive behavior support interventions in early childhood to prevent obesity. Child Dev. 2017;88:427–35.
Yackobovitch‐Gavan M, Wolf Linhard D, Nagelberg N, Poraz I, Shalitin S, Phillip M, et al. Intervention for childhood obesity based on parents only or parents and child compared with follow‐up alone. Pediatr Obes. 2018;13:647–55.
Rhee KE, Kessl S, Lindback S, Littman M, El-Kareh RE. Provider views on childhood obesity management in primary care settings: a mixed methods analysis. BMC Health Serv Res. 2018;18:1–10.
McPhee PG, Zenlea I, Hamilton JK, Ho J, Ball GDC, Mian R, et al. Individual and family characteristics associated with health indicators at entry into multidisciplinary pediatric weight management: findings from the CANadian Pediatric Weight management Registry (CANPWR). Int J Obes. 2022;46:85–94.
Morrison KM, Damanhoury S, Buchholz A, Chanoine J, Lambert M, Tremblay MS, et al. The CANadian Pediatric Weight management Registry (CANPWR): study protocol. BMC Pediatr. 2014;14:1–8.
Onis MD, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85:660–7.
Morrison KM, Ball GDC, Ho J, Mackie P, Buckholz A, Chanoine J, et al. The CANadian Pediatric Weight management Registry (CANPWR): lessons learned from developing and initiating a national, multi-centre study embedded in pediatric clinical practice. BMC Pediatr. 2018;18:1–7.
World Health Organization. WHO child growth standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: methods and development. World Health Organization; Geneva, Switzerland. 2006.
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114:555–76.
Jean-François Yale M, Breay Paty M, Peter A. Diabetes Canada Clinical Practice Guidelines Expert Committee. Can J Diabetes. 2018;42:S104–8.
Dileepan K, Feldt MM. Type 2 diabetes mellitus in children and adolescents. Pediatr Rev. 2013;34:541–8.
Daniels SR, Greer FR, Committee on Nutrition. Lipid screening and cardiovascular health in childhood. Pediatrics. 2008;122:198–208.
Zahn K, Ibrahim Q, Ball GDC, Buchholz A, Hamilton J, Ho J, et al. Variability in how Canadian pediatric weight management clinics deliver care: evidence from the Canadian pediatric weight management registry. Child Obes. 2021;17:420–6.
Reinehr T, Lass N, Toschke C, Rothermel J, Lanzinger S, Holl RW. Which amount of BMI-SDS reduction is necessary to improve cardiovascular risk factors in overweight children? J Clin Endocrinol Metab. 2016;101:3171–9.
Ford AL, Hunt LP, Cooper A, Shield JP. What reduction in BMI SDS is required in obese adolescents to improve body composition and cardiometabolic health? Arch Dis Child. 2009;95:256–61.
Kolsgaard MLP, Joner G, Brunborg C, Anderssen SA, Tonstad S, Andersen LF. Reduction in BMI z-score and improvement in cardiometabolic risk factors in obese children and adolescents. The Oslo Adiposity Intervention Study—a hospital/public health nurse combined treatment. BMC Pediatr. 2011;11:1–8.
Shah B, Cost KT, Fuller A, Birken CS, Anderson LN. Sex and gender differences in childhood obesity: contributing to the research agenda. BMJ Nutr Prev Health. 2020;3:387.
Tanda R, Salsberry P. The impact of the 2007 expert committee recommendations on childhood obesity preventive care in primary care settings in the United States. J Pediatr Health Care. 2014;28:241–50.
Ross MM, Kolbash S, Cohen GM, Skelton JA. Multidisciplinary treatment of pediatric obesity: nutrition evaluation and management. Nutr Clin Pract. 2010;25:327–34.
Zenlea IS, Burton ET, Askins N, Pluhar EI, Rhodes ET. The burden of psychosocial stressors and urgent mental health problems in a pediatric weight management program. Clin Pediatr. 2015;54:1247–56.
Griffiths LJ, Dezateux C, Hill A. Is obesity associated with emotional and behavioural problems in children? Findings from the Millennium Cohort Study. Int J Pediatr Obes. 2011;6:e423–32.
Halfon N, Larson K, Slusser W. Associations between obesity and comorbid mental health, developmental, and physical health conditions in a nationally representative sample of US children aged 10 to 17. Acad Pediatr. 2013;13:6–13.
Warschburger P, Kröller K. Loss to follow-up in a randomized controlled trial study for pediatric weight management (EPOC). BMC Pediatr. 2016;16:1–9.
Whitlock EP, O’Connor EA, Williams SB, Beil TL, Lutz KW. Effectiveness of weight management interventions in children: a targeted systematic review for the USPSTF. Pediatrics. 2010;125:e396–418.
Acknowledgements
The CANPWR study was funded by the Canadian Institutes of Health Research, the Population Health Research Institute (PHRI), McMaster Children’s Hospital, and McMaster University. PGM was funded by a CIHR Fellowship FRN 164649. JKH was supported with unrestricted research funds by the University of Toronto Mead Johnson Chair in Child Nutrition. GDCB was supported by an Alberta Health Services Chair in Obesity Research. The CANPWR investigators would like to acknowledge the research teams at each clinic and at the central coordinating site (PHRI) for their exceptional support and all of the children and their families for participating in this study.
Author information
Authors and Affiliations
Consortia
Contributions
PGM wrote the first draft of this manuscript supported by the writing group comprised of GDCB, AB, JKH, JH, IZ, LT, and KMM. GDCB, AB, JKH, JH, IZ, LT, and KMM contributed to the study design, study conduct, data collection and interpretation of findings. KMM also oversaw the acquisition of funding and study design. PGM conducted the analysis, and LT contributed to the analytical review. All authors, including those in the consortium listed below (CB, JPC, SH, AML, LL, MT), edited the manuscript and approved the final version.
Corresponding author
Ethics declarations
Competing interests
PGM, AB, JPC, AL, MST, JH and LT have no competing interests. IZ is an advisory board member for Novo Nordisk, Dexcom, and Abbot Diabetes Care. JKH is a site investigator for studies sponsored by Levo Therapeutics, Canada, Rhythm Pharmaceuticals and Eli Lilly, and an advisory board member for Novo Nordisk. GDCB and LL are advisory board members for Novo Nordisk. KMM is an advisory board member for Novo Nordisk and Akcea Therapeutics, Canada.
Ethics approval and consent to participate
The CANPWR study was approved by the following Research Ethics Boards: Hamilton Integrated Research Ethics Board, Conjoint Health Research Ethics Board (Calgary, Alberta), Research Ethics Board Trillium Health Partners, Health Research Ethics Board—Health Panel (Edmonton, Alberta), Children’s Hospital of Eastern Ontario Research Ethics Board, The Hospital for Sick Children Research Ethics Board, University of British Columbia Clinical Research Ethics Board, CHU Sainte-Justine Research Ethics Board, McGill University Health Centre Research Ethics Board—Pediatrics. All methods in the study were performed in accordance with the relevant guidelines and regulations of each Research Ethics Board. Written informed consent was obtained from the child’s parent or guardian, and participants provided assent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
McPhee, P.G., Ball, G.D.C., Buchholz, A. et al. Exploring the association between individual, family, and program characteristics and change in health outcomes 12 months after enrollment into the CANadian Pediatric Weight management Registry (CANPWR). Int J Obes 49, 109–117 (2025). https://doi.org/10.1038/s41366-024-01631-2
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41366-024-01631-2