Abstract
Objective
It is critical to accurately determine the level of obesity and health status since overweight/obesity has become a main global public health problem. This systematic review attempted to evaluate the consistency and correlation between body composition measurement indicators and body mass index (BMI) in childhood and adolescence.
Methods
Seven electronic databases (Web of Science, PubMed, Cochrane Library, Embase, CNKI, WANFANG DATA, SinoMed) were searched to collect the literature published since 1999 with the focus on the relationship between body composition measurement indicators and BMI to measure obesity in childhood and adolescence.
Results
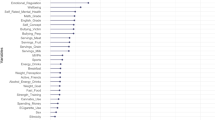
Among the 28 articles included, 13 articles reported a moderate to very strong correlation between %BF and BMI in obesity measurement (range: 0.49–0.907), while two articles reported a strong to very strong correlation between FM and BMI (range: 0.60–0.86). Six articles reported good to excellent obesity measurement consistency between %BF and BMI (range: 0.441–0.876), one article reported WC (0.58) and WHtR (0.46) in the moderate consistency with BMI, and one article reported a relatively poor to fair consistency between FM and BMI (range: 0.167–0.409). WC, WHtR, and BMI showed the moderate consistency in pre-adolescent children. In pre-adolescence and adolescence, the measurement consistency between %BF and BMI was higher than that between FM and BMI. Gender difference existed in the consistency between %BF and BMI during adolescence.
Conclusion
A range of body composition indicators such as %BF, WC, WHtR, and FM could provide valuable body composition measurements, complement BMI for obesity assessment in children and adolescents, and facilitate efficient and comprehensive surveillance of childhood obesity.
Registration
PROSPERO CRD42024506932.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
James W. WHO recognition of the global obesity epidemic. Int J Obes. 2008;32:S120–S126.
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in underweight and obesity from 1990 to 2022: a pooled analysis of 3663 population representative studies with 222 million children, adolescents, and adults. Lancet. 2024;403:1027–50.
O’Connor E, Evans C, Burda B, Walsh E, Eder M, Lozano P. Screening for obesity and intervention for weight management in children and adolescents: a systematic evidence review for the US Preventive Services Task Force. J Am Med Assoc 2017;317:2427–44.
Liang J, Zheng S, Li X, Xiao D, Wang P. Associations of community, family and early individual factors with body mass index z-scores trajectories among Chinese children and adolescents. Sci Rep. 2021;11:14535.
Banack H, Wactawski-Wende J, Hovey K, Stokes A. Is BMI a valid measure of obesity in post-menopausal women? Menopause. 2018;25:307–13.
Nuttall F. Body mass index obesity, BMI, and health: a critical review. Nutr Today. 2015;50:117–23.
Malina R, Katzmarzyk P. Validity of the body mass index as an indicator of the risk and presence of overweight in adolescents. Am J Clin Nutr. 1997;70:131S–6S.
Jayawardena R, Ranasinghe P, Ranathunga T, Mathangasinghe Y, Wasalathanththri S, Hills A. Novel anthropometric parameters to define obesity and obesity-related disease in adults: a systematic review. Nutr Rev. 2020;78:498–513.
Magalhães E, Sant’Ana L, Priore S, Franceschini S. Waist circumference, waist/height ratio, and neck circumference as parameters of central obesity assessment in children. Rev Paul Pediatr. 2014;32:273–81.
Junior C, Mocellin M, Gonçalves E, Silva D, Trindade E. Anthropometric indicators as body fat discriminators in children and adolescents: a systematic review and meta-analysis. Adv Nutr. 2017;8:718–27.
Mahmoud I, Al-Wandi A, Gharaibeh S, Mohamed S. Concordances and correlations between anthropometric indices of obesity: a systematic review. Public Health. 2021;198:301–6.
United Nations. Convention on the Rights of the Child. General Assembly resolution 44/25, United Nations Headquarter; 1989.
Farbo D, Rhea D. A pilot study examining body composition classification differences between body mass index and bioelectrical impedance analysis in children with high levels of physical activity. Front Pediatr. 2021;9:724053.
Himes J. Agreement among anthropometric indicators identifying the fattest adolescents. Int J Obes. 1999;23:S18–S21.
Laurson K, Eisenmann J, Welk G. Body mass index standards based on agreement with health-related body fat. Am J Prev Med. 2011;41:S100–S105.
McConnell-Nzungaa J, Naylorb P, Macdonaldc H, Rhodesb R, Hoferd S, McKaye H. Classification of obesity varies between body mass index and direct measures of body fat in boys and girls of Asian and European ancestry. Meas Phys Educ Exerc Sci. 2018;22:154–66.
Kakinami L, Henderson M, Chiolero A, Cole T, Paradis G. Identifying the best body mass index metric to assess adiposity change in children. Arch Dis Child. 2014;99:1020–4.
Ellis K, Abrams S, Wong W. Monitoring childhood obesity: assessment of the weight/height2 index. Am J Epidemiol. 1999;150:939–46.
Clasey J, Easley E, Murphy M, Kiessling S, Stromberg A, Schadler A, et al. Body mass index percentiles versus body composition assessments: challenges for disease risk classifications in children. Front Pediatr. 2023;11:1112920.
Brann L. Classifying preadolescent boys based on their weight status and percent body fat produces different groups. J Am Diet Assoc. 2008;108:1018–22.
Salman H, Koca T, Dereci S, Akçam M. Comparison of body composition and body mass index in the determination of obesity in schoolchildren. Turk Arch Pediatr. 2022;57:506–10.
Veldhuis L, Vogel I, Jansen W, Renders C, HiraSing R, Raat H. Moderate agreement between body mass index and measures of waist circumference in the identification of overweight among 5-year-old children; the ‘Be active, eat right’ study. BMC Pediatr. 2013;13:1–8.
Hubert H, Guinhouya C, Allard L, Durocher A. Comparison of the diagnostic quality of body mass index, waist circumference and waist-to-height ratio in screening skinfold-determined obesity among children. J Sci Med Sport. 2009;12:449–51.
Cameron N, Jones L, Griffiths P, Norris S, Pettifor J. How well do waist circumference and body mass index reflect body composition in pre-pubertal children? Eur J Clin Nutr. 2009;63:1065–70.
Kim K, Yun S, Jang M, Oh K. Body fat percentile curves for Korean children and adolescents: a data from the Korea National Health and Nutrition Examination Survey 2009-2010. J Korean Med Sci. 2013;28:443–9.
Rerksuppaphol S, Rerksuppaphol L. Optimal cut-off points of weight for height, waist circumference and waist-to-height ratio for defining overweight and obesity in Thai school-aged children. J Res High Sch. 2013;13:13–18.
Wu S, Ma S, Ma J, Ma J, Guo J, Yang Q, et al. Body composition analysis of children and adolescents in Haidian District. Chin J Sch Health. 2009;30:1014–6.
Huang X, Zhang Y, Lv J, Li Y, Chen D, Gao P, et al. Study on the relationship between body mass index and body fat percentage of school-age children and adolescents in Shunyi District, Beijing. Med Inf. 2019;32:134–6.
Zhang Q, Du W, Hu X, Liu A, Pan H, Ma G. The relationship between body mass index and percentage body fat among Chinese adolescent living in urban Beijing. Chin J Epidemiol. 2004;25:113–6.
Zhang H, Li Y, Liu C, Xu Y. Body composition analysis of preschool children aged 4 to 6 years in Jinan city. Chin J Child Health Care. 2019;27:554–7.
Zhang W, Liu W, Lin R, Wu J, Du L. Relation between percentage body fat and body mass index among primary school students aged between 6 to 11 years old living in urban Guangzhou. Chin J Child Health Care. 2008;16:271–4.
Su Y, Wang H, Li Q, Zhang X, Qiu M. Analysis of body composition of children with different genders, ages and nutritional status. Chin J Child Health Care. 2021;29:713–6.
Li B, Guo J, Wang H, Cao X, Zhang Y, Hua L. Evaluation of obesity by body mass index, waist-hip-ratio and percentage body fat in adolescent. Chongqin Med J. 2014;43:4637–42.
Li S, Zhong Y. Application of body composition analysis in screening overweight and obesity of school-age children. Chin J Child Health Care. 2022;30:540–4.
Trung N, Chu D, Hanh N. Percentage body fat is as a good indicator for determining adolescents who are overweight or obese: a cross-sectional study in Vietnam. Osong Public Health Res Perspect. 2019;10:108.
Taylor R, Jones I, Williams S, Goulding A. Body fat percentages measured by dual-energy X-ray absorptiometry corresponding to recently recommended body mass index cutoffs for overweight and obesity in children and adolescents aged 3–18 y. Am J Clin Nutr. 2002;76:1416–21.
van Gent M, Pienaar A, Noorbhai H. Comparison of body mass index and fat percentage criteria classification of 7–13 year-old rural boys in South Africa. BMC Pediatr. 2020;20:1–8.
Houda B, Sarra K, Karmous I, Henda J, Khalid E, Hassan A, et al. Relationship of body mass index to percent body fat determined by deuterium isotopic dilution and impedancemetry among Tunisian schoolchildren. Afr Health Sci. 2023;23:664–71.
Kigaru D, Ndung’u Z, Macharia-Mutie C. Application of stable isotope dilution techniques to assess body fat and comparison with WHO BMI-for-age classification as a measure of obesity among schoolchildren in Nairobi, Kenya. Public Health Nutr. 2021;24:3587–91.
Anzolin C, Silva D, Zanuto E, Cayres S, Codogno J, Junior P, et al. Accuracy of different cutoff points of body mass index to identify overweight according to body fat values estimated by DEXA. J Pediatr. 2017;93:58–63.
Altman D. Practical statistics for medical research. 1st ed. New York, NY: Chapman and Hall/CRC;1990.
World Health Organization. World Health Organization AnthroPlus for personal computers manual: software for assessing growth of the world’s children and adolescents. Geneva: WHO; 2009.
Lin W, Ren R, Wen D. Research advances in childhood obesity intervention sites. Chin J Child Health Care. 2017;25:51–4.
Srdić B, Obradović B, Dimitrić G, Stokic E, Babovic S. Relationship between body mass index and body fat in children-age and gender differences. Obes Res Clin Pract. 2012;6:e167–e173.
Tennefors C, Forsum E. Assessment of body fatness in young children using the skinfold technique and BMI vs body water dilution. Eur J Clin Nutr. 2004;58:541–7.
Morimoto A, Nishimura R, Sano H, Matsudaira T, Miyashita Y, Shirasawa T, et al. Gender differences in the relationship between percent body fat (%BF) and body mass index (BMI) in Japanese children. Diabetes Res Clin Pract. 2007;78:123–5.
Jinyuan L, Wan T, Guanqin C, Yin L, Changyong F. Correlation and agreement: overview and clarification of competing concepts and measures. Shanghai Arch Psychiatry. 2016;28:115.
Gao Y, Xie X, Cianflone K, Lapointe M, Guan J, Bu-Jiaer G, et al. Ethnic differences in acylation stimulating protein (ASP) in Xinjiang Uygur autonomous region, China. Int J Clin Exp Med. 2015;8:2823–30.
Taylor R, Williams S, Grant A, Taylor B, Goulding A, Goulding A. Predictive ability of waist-to-height in relation to adiposity in children is not improved with age and sex-specific values. Obesity. 2011;19:1062–8.
He W, Li Q, Yang M, Jiao J, Ma X, Zhou Y, et al. Lower BMI cutoffs to define overweight and obesity in China. Obesity. 2015;23:684–91.
He W, Zhang S, Song A, Yang M, Jiao J, Allison D, et al. Greater abdominal fat accumulation is associated with higher metabolic risk in Chinese than in white people: an ethnicity study. PLoS ONE. 2013;8:e58688.
Kurtoglu S, Mazicioglu M, Ozturk A, Hatipoglu N, Cicek B, Ustunbas H. Body fat reference curves for healthy Turkish children and adolescents. Eur J Pediatr. 2010;169:1329–35.
Loomba-Albrecht L, Styne D. Effect of puberty on body composition. Curr Opin Endocrinol Diabetes Obes. 2009;16:10–15.
Acknowledgements
We appreciate the Shanghai Municipal Centres for Disease Control and Prevention (SCDC) and the participating district CDCs, local communities and schools, as well as all participants in the Sixth Round of Shanghai Public Health Three Year Action Program.
Funding
This study was supported by The Sixth Round of Shanghai Public Health Three Year Action Program 2023–2025 (Grant no. GWVI-7), Ministry of Science and Technology (Grant no. G2023141005L), Ministry of Education (Grant no. 1125000172), Fundamental Research Funds for the Central Universities (Grant no. 3225002002A1), and Jiangsu Provincial Department of Science and Technology.
Author information
Authors and Affiliations
Contributions
RY and JY were responsible for designing the review plan, retrieving and screening articles, analyzing and interpreting the results, and drafting the report. CL, WQ, DY, HX, XN, and SY assisted in the analysis, result interpretation, and critical appraisal of the report. WD and FZ conceptualized the study, provided guidance throughout the study, and contributed to the critical review of the final draft.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yang, R., Yu, J., Luo, C. et al. Correlations and consistency of body composition measurement indicators and BMI: a systematic review. Int J Obes 49, 4–12 (2025). https://doi.org/10.1038/s41366-024-01638-9
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41366-024-01638-9
This article is cited by
-
Relationship of fat mass index and fat free mass index with body mass index and association with sleeping patterns and physical activity in Saudi young adults women
Journal of Health, Population and Nutrition (2025)
-
Adiposity indices mediate the association between dietary inflammatory index and type 2 diabetes risk in women with prior gestational diabetes mellitus
Diabetology & Metabolic Syndrome (2025)
-
Supervised machine learning algorithms for the classification of obesity levels using anthropometric indices derived from bioelectrical impedance analysis
Scientific Reports (2025)