Abstract
Objectives
To investigate the association of metabolic status newly defined or obesity with asymptomatic intracranial arterial stenosis (aICAS) among populations in rural China.
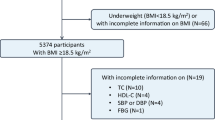
Methods
The cross-sectional study is based on the Rose asymptomatic IntraCranial Artery Stenosis (RICAS) cohort, which enrolled 2005 participants aged 40 years or older without a history of clinical stroke or transient ischemic attack. Metabolically healthy status (MH) was defined by a newly proposed criterion: (1) systolic blood pressure (SBP) < 130 mmHg and without antihypertensive medication; (2) a waist-to-hip ratio (WHR) below 1.03 for men and below 0.95 for women; (3) no diabetes. All participants were categorized based on their metabolic status and obesity. Multivariate logistic regression models were used to investigate the association between metabolic status or obesity and aICAS.
Results
Among 2005 participants, 1597 (79.65%) were defined as metabolically unhealthy status (MU) according to the new criterion. MU was significantly associated with aICAS (OR 2.02, 95% CI 1.11–3.68, P = 0.021), especially moderate-to-severe aICAS (OR 2.43, 95% CI 1.04–5.72, P = 0.042). The prevalence of aICAS increased with the numbers of metabolic disorders (P for linear trend <0.001). Both metabolically unhealthy normal-weight (MUN) (OR 2.11, 95% CI 1.10–4.03, P = 0.025) and metabolically unhealthy obesity (MUO) (OR 3.30, 95% CI 1.64–6.64, P = 0.001) were significantly correlated with aICAS, but not metabolically healthy obesity (MHO). Subgroup analysis further confirmed the association between MU and aICAS risk only in men (P for interaction = 0.042).
Conclusions
MU defined by the new criterion was significantly associated with aICAS, especially with moderate-to-severe aICAS. This novel criterion effectively identifies individuals with a high prevalence of aICAS among populations with obesity, which could be crucial for stroke prevention.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
All data used in this study were available upon request.
References
Global burden of 288 causes of death and life expectancy decomposition in 204 countries and territories and 811 subnational locations, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet (London, England) 2024;403:2100–32.
Prust ML, Forman R, Ovbiagele B. Addressing disparities in the global epidemiology of stroke. Nat Rev Neurol. 2024;20:207–21.
Wang Y, Zhao X, Liu L, Soo YO, Pu Y, Pan Y, et al. Prevalence and outcomes of symptomatic intracranial large artery stenoses and occlusions in China: the Chinese Intracranial Atherosclerosis (CICAS) Study. Stroke. 2014;45:663–9.
Schulze MB. Metabolic health in normal-weight and obese individuals. Diabetologia. 2019;62:558–66.
Schulze MB, Stefan N. Metabolically healthy obesity: from epidemiology and mechanisms to clinical implications. Nat Rev Endocrinol. 2024;20:633–46.
Li S, Sun X, Zhao Y, Wang X, Ji X, Sang S, et al. Association between metabolic syndrome and asymptomatic cerebral arterial stenosis: a cross-sectional study in Shandong, China. Front Neurol. 2021;12:644963.
Bang OY, Kim JW, Lee JH, Lee MA, Lee PH, Joo IS, et al. Association of the metabolic syndrome with intracranial atherosclerotic stroke. Neurology. 2005;65:296–8.
Rincon F, Sacco RL, Kranwinkel G, Xu Q, Paik MC, Boden-Albala B, et al. Incidence and risk factors of intracranial atherosclerotic stroke: the Northern Manhattan Stroke Study. Cerebrovasc Dis. 2009;28:65–71.
Wang Q, Zhao Y, Wang X, Ji X, Sang S, Shao S, et al. Association between asymptomatic intracranial arterial stenosis and insulin resistance or diabetes mellitus: a cross-sectional study in rural Shandong, China. BMJ Open Diab Res Care. 2020;8:e001788.
Blüher M. Metabolically healthy obesity. Endocr Rev. 2020;41:bnaa004.
Horn JW, Feng T, Mørkedal B, Strand LB, Horn J, Mukamal K, et al. Obesity and risk for first ischemic stroke depends on metabolic syndrome: The HUNT study. Stroke. 2021;52:3555–61.
Mirzaei B, Abdi H, Serahati S, Barzin M, Niroomand M, Azizi F, et al. Cardiovascular risk in different obesity phenotypes over a decade follow-up: Tehran Lipid and Glucose Study. Atherosclerosis. 2017;258:65–71.
Yu M, Zhang S, Wang L, Wu J, Li X, Yuan J. Metabolically healthy obesity and carotid plaque among steelworkers in North China: the role of inflammation. Nutrients. 2022;14:5123.
Gao M, Lv J, Yu C, Guo Y, Bian Z, Yang R, et al. Metabolically healthy obesity, transition to unhealthy metabolic status, and vascular disease in Chinese adults: a cohort study. PLoS Med. 2020;17:e1003351.
Eckel N, Li Y, Kuxhaus O, Stefan N, Hu FB, Schulze MB. Transition from metabolic healthy to unhealthy phenotypes and association with cardiovascular disease risk across BMI categories in 90 257 women (the Nurses’ Health Study): 30 year follow-up from a prospective cohort study. The Lancet. Diab Endocrinol. 2018;6:714–24.
Eckel N, Meidtner K, Kalle-Uhlmann T, Stefan N, Schulze MB. Metabolically healthy obesity and cardiovascular events: A systematic review and meta-analysis. Eur J Prevent Cardiol. 2016;23:956–66.
Hinnouho GM, Czernichow S, Dugravot A, Batty GD, Kivimaki M, Singh-Manoux A. Metabolically healthy obesity and risk of mortality: does the definition of metabolic health matter? Diab Care. 2013;36:2294–300.
Zembic A, Eckel N, Stefan N, Baudry J, Schulze MB. An empirically derived definition of metabolically healthy obesity based on risk of cardiovascular and total mortality. JAMA Netw Open. 2021;4:e218505.
Li Q, Wang P, Ma R, Guo X, Sun Y, Zhang X. A novel criterion of metabolically healthy obesity could effectively identify individuals with low cardiovascular risk among Chinese cohort. Front Endocrinol. 2023;14:1140472.
Seo DH, Cho Y, Seo S, Ahn SH, Hong S, Ha KH, et al. Association between metabolically healthy obesity and subclinical atherosclerosis in the Cardiovascular and Metabolic Diseases Etiology Research Center (CMERC) Cohort. J Clin Med. 2022;11:2440.
Wang X, Zhao Y, Ji X, Sang S, Shao S, Yan P, et al. Kongcun town asymptomatic intracranial artery stenosis study in Shandong, China: cohort profile. BMJ Open. 2020;10:e036454.
Zhao W, Ma X, Ju J, Zhao Y, Wang X, Li S, et al. Association of visceral adiposity index with asymptomatic intracranial arterial stenosis: a population-based study in Shandong, China. Lipids Health Dis. 2023;22:64.
Yang W, Li JP, Zhang Y, Fan FF, Xu XP, Wang BY, et al. Association between body mass index and all-cause mortality in hypertensive adults: results from the China Stroke Primary Prevention Trial (CSPPT). Nutrients. 2016;8:384.
Sun Q, Wang Q, Wang X, Ji X, Sang S, Shao S, et al. Prevalence and cardiovascular risk factors of asymptomatic intracranial arterial stenosis: the Kongcun Town Study in Shandong, China. Eur J Neurol. 2020;27:729–35.
Samuels OB, Joseph GJ, Lynn MJ, Smith HA, Chimowitz MI. A standardized method for measuring intracranial arterial stenosis. Ajnr Am J Neuroradiol. 2000;21:643–6.
Lee HJ, Choi EK, Lee SH, Kim YJ, Han KD, Oh S. Risk of ischemic stroke in metabolically healthy obesity: A nationwide population-based study. PloS ONE. 2018;13:e0195210.
Hamer M, Stamatakis E. Metabolically healthy obesity and risk of all-cause and cardiovascular disease mortality. J Clin Endocrinol Metab. 2012;97:2482–8.
Opio J, Croker E, Odongo GS, Attia J, Wynne K, McEvoy M. Metabolically healthy overweight/obesity are associated with increased risk of cardiovascular disease in adults, even in the absence of metabolic risk factors: A systematic review and meta-analysis of prospective cohort studies. Obes Rev. 2020;21:e13127.
Hu C, Wang S, Lin H, Wan Q, Zheng R, Zhu Y, et al. Body size, insulin sensitivity, metabolic health and risk of cardiovascular disease in Chinese adults: Insights from the China Cardiometabolic Disease and Cancer Cohort (4C) study. Diab Obes Metab. 2024;26:2176–87.
Agius R, Pace NP, Fava S. Phenotyping obesity: A focus on metabolically healthy obesity and metabolically unhealthy normal weight. Diab Metab Res Rev. 2024;40:e3725.
Goossens GH. The metabolic phenotype in obesity: fat mass, body fat distribution, and adipose tissue function. Obes Facts. 2017;10:207–15.
Martin S, Cule M, Basty N, Tyrrell J, Beaumont RN, Wood AR, et al. Genetic evidence for different adiposity phenotypes and their opposing influences on ectopic fat and risk of cardiometabolic disease. Diabetes. 2021;70:1843–56.
Shungin D, Winkler TW, Croteau-Chonka DC, Ferreira T, Locke AE, Mägi R, et al. New genetic loci link adipose and insulin biology to body fat distribution. Nature. 2015;518:187–96.
Yu S, Guo X, Li G, Yang H, Zheng L, Sun Y. Gender discrepancy in the predictive effect of metabolic syndrome and its components on newly onset cardiovascular disease in elderly from rural China. BMC Geriatr. 2021;21:505.
Huang Y, Chen Z, Wang X, Zheng C, Shao L, Tian Y, et al. Comparison of the three most commonly used metabolic syndrome definitions in the chinese population: a prospective study. Metabolites. 2022;13:12.
Santos-Marcos JA, Mora-Ortiz M, Tena-Sempere M, Lopez-Miranda J, Camargo A. Interaction between gut microbiota and sex hormones and their relation to sexual dimorphism in metabolic diseases. Biol Sex Differ. 2023;14:4.
Garaulet M, Pérex-Llamas F, Fuente T, Zamora S, Tebar FJ. Anthropometric, computed tomography and fat cell data in an obese population: relationship with insulin, leptin, tumor necrosis factor-alpha, sex hormone-binding globulin and sex hormones. Eur J Endocrinol. 2000;143:657–66.
Gerdts E, Regitz-Zagrosek V. Sex differences in cardiometabolic disorders. Nat Med. 2019;25:1657–66.
Liu J, Fox CS, Hickson DA, May WD, Hairston KG, Carr JJ, et al. Impact of abdominal visceral and subcutaneous adipose tissue on cardiometabolic risk factors: the Jackson Heart Study. J Clin Endocrinol Metab. 2010;95:5419–26.
Henstridge DC, Abildgaard J, Lindegaard B, Febbraio MA. Metabolic control and sex: a focus on inflammatory-linked mediators. Br J Pharmacol. 2019;176:4193–207.
Song HJ, Oh S, Quan S, Ryu OH, Jeong JY, Hong KS et al. Gender differences in adiponectin levels and body composition in older adults: Hallym aging study. BMC G Eriatrics. 2014;14:8.
Acknowledgements
We are grateful to all the RICAS study participants and the staff at Shandong Provincial Hospital, China involved in this study.
Funding
This study was supported by grants from the Jinan Science and Technology Bureau (201704101), the Department of Science and Technology of Shandong Province (ZR2017MH114, ZR2020QH109, ZR2022LSW010, and ZR2023MH070), the National Natural Science Foundation of China (81971128, and 82201477). The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Author information
Authors and Affiliations
Contributions
LG, YP, YY, SK and SS analysed the data and contributed to the original draft. ML,YZ, XM and XW contributed to the review and revision of the manuscript. QS conceived and designed the study. All the authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Guo, L., Pan, Y., Yang, Y. et al. Association of novel metabolic status with asymptomatic intracranial arterial stenosis: A cross-sectional study. Int J Obes 49, 1024–1030 (2025). https://doi.org/10.1038/s41366-025-01723-7
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41366-025-01723-7
This article is cited by
-
Association of hepatic steatosis index with asymptomatic intracranial arterial stenosis: a cross-sectional study
Neurological Sciences (2026)