Abstract
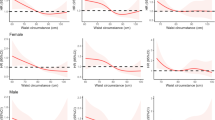
This review aimed to explore the association between metabolically healthy obesity (MHO) and the risk of depression. Databases (EMBASE, PubMed, Web of Science, Cochrane Library) were searched up to 20 June 2024. Observational studies were included if they compared groups with MHO, metabolically unhealthy nonobesity, and metabolically unhealthy obesity to groups with metabolically healthy nonobesity for the risk of depression. The random-effect model was used to calculate the pooled odds ratios (ORs). Subgroup analyses and meta-regressions were conducted according to age, study design, definition of MHO, BMI cut-off value, depression assessment method, geographic location, ethnicity, development status, and gender to explore the sources of heterogeneity. Three cohorts and 9 cross-sectional studies (N = 1,277,267 participants) were included in this review. Individuals with MHO (OR 1.08 [95% CI 1.04, 1.12], I² = 88.3%), metabolically unhealthy nonobesity (OR 1.15 [95% CI 1.04, 1.28], I² = 99.6%), and metabolically unhealthy obesity (OR 1.30 [95% CI 1.12, 1.51], I² = 99.8%) had an increased risk of depression than individuals with metabolically healthy nonobesity. The association between MHO and risk of depression was stronger in women (OR = 1.14; 95% CI: 1.08–1.20) and populations from North America (OR = 1.26; 95% CI: 1.01–1.58) and Europe (OR = 1.23; 95% CI: 1.07–1.41). Inconsistencies in MHO definitions and BMI cutoff values across studies were important sources of heterogeneity (subgroup analysis: PQ = 29.87, p = 0.001; meta-regression: p = 0.015, R² = 100%). MHO was associated with an increased risk of depression, particularly among women and populations from North America and Europe. These high-risk groups need personalized interventions. Standardizing definition for MHO could enhance comparability across studies. Future prospective cohort studies are needed to validate our findings by including populations from developing nations and employing rigorous definitions.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Milligan MN, Duemling K, Radovanovic N, Alkozah M, Riblet N. Impacts of nutrition counseling on depression and obesity: a scoping review. Obes Rev. 2023;24:e13594.
Hasin DS, Sarvet AL, Meyers JL, Saha TD, Ruan WJ, Stohl M, et al. Epidemiology of adult DSM-5 major depressive disorder and its specifiers in the United States. JAMA Psychiatry. 2018;75:336–46.
GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789–858.
van Sloten TT, Sedaghat S, Carnethon MR, Launer LJ, Stehouwer CDA. Cerebral microvascular complications of type 2 diabetes: stroke, cognitive dysfunction, and depression. Lancet Diabetes Endocrinol. 2020;8:325–36.
Plackett B. The vicious cycle of depression and obesity. Nature. 2022;608:S42–3.
Pan A, Sun Q, Czernichow S, Kivimaki M, Okereke OI, Lucas M, et al. Bidirectional association between depression and obesity in middle-aged and older women. Int J Obes. 2012;36:595–602.
Fulton S, Décarie-Spain L, Fioramonti X, Guiard B, Nakajima S. The menace of obesity to depression and anxiety prevalence. Trends Endocrinol Metab. 2022;33:18–35.
Milaneschi Y, Simmons WK, van Rossum EFC, Penninx BW. Depression and obesity: evidence of shared biological mechanisms. Mol Psychiatry. 2019;24:18–33.
Schachter J, Martel J, Lin CS, Chang CJ, Wu TR, Lu CC, et al. Effects of obesity on depression: a role for inflammation and the gut microbiota. Brain Behav Immun. 2018;69:1–8.
Delgado I, Cussotto S, Anesi A, Dexpert S, Aubert A, Aouizerate B, et al. Association between the indole pathway of tryptophan metabolism and subclinical depressive symptoms in obesity: a preliminary study. Int J Obes. 2022;46:885–8.
Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW, et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67:220–9.
Björntorp P. Do stress reactions cause abdominal obesity and comorbidities? Obes Rev. 2001;2:73–86.
Malki A, Shaik RA, Sami W. Association between metabolically healthy obesity and metastasis in lung cancer patients—a systematic review and meta-analysis. Front Endocrinol. 2023;14:1238459.
Blüher M. Metabolically healthy obesity. Endocr Rev. 2020;41:bnaa004.
Bell JA, Kivimaki M, Hamer M. Metabolically healthy obesity and risk of incident type 2 diabetes: a meta-analysis of prospective cohort studies. Obes Rev. 2014;15:504–15.
Opio J, Croker E, Odongo GS, Attia J, Wynne K, McEvoy M. Metabolically healthy overweight/obesity are associated with increased risk of cardiovascular disease in adults, even in the absence of metabolic risk factors: a systematic review and meta-analysis of prospective cohort studies. Obes Rev. 2020;21:e13127.
Liu Y, Zhao A, Sun G, Wang R, Zhang J, Lip GYH, et al. Relationship between metabolic status, physical activity and cardiovascular disease in participants with obesity. Int J Obes. 2024;48:788–95.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–5.
Yang JC, Yang ZR, Yu SQ, Zhan SY, Sun F. Introduction on ‘assessing the risk of bias of individual studies’ in systematic review of health-care intervention programs revised by the Agency for Healthcare Research and Quality. Zhonghua Liu Xing Bing Xue Za Zhi. 2019;40:106–11.
Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
Wang Z, Cheng Y, Li Y, Han J, Yuan Z, Li Q, et al. The relationship between obesity and depression is partly dependent on metabolic health status: a nationwide inpatient sample database study. Front Endocrinol. 2022;13:880230.
Seo Y, Lee S, Ahn JS, Min S, Kim MH, Kim JY, et al. Association of metabolically healthy obesity and future depression: using national health insurance system data in Korea from 2009-2017. Int J Environ Res Public Health. 2020;18:63.
Yu M, Shi Y, Gu L, Wang W. “Jolly fat” or “sad fat”: a systematic review and meta-analysis of the association between obesity and depression among community-dwelling older adults. Aging Ment Health. 2022;26:13–25.
Silva DA, Coutinho E, Ferriani LO, Viana MC. Depression subtypes and obesity in adults: a systematic review and meta-analysis. Obes Rev. 2020;21:e12966.
Quek YH, Tam WWS, Zhang MWB, Ho RCM. Exploring the association between childhood and adolescent obesity and depression: a meta-analysis. Obes Rev. 2017;18:742–54.
Flint SW, Nobles J, Gately P, Sahota P. Weight stigma and discrimination: a call to the media. Lancet Diabetes Endocrinol. 2018;6:169–70.
Mannan M, Mamun A, Doi S, Clavarino A. Prospective associations between depression and obesity for adolescent males and females—a systematic review and meta-analysis of longitudinal studies. PLoS ONE. 2016;11:e0157240.
Kimm SY, Glynn NW, Kriska AM, Barton BA, Kronsberg SS, Daniels SR, et al. Decline in physical activity in black girls and white girls during adolescence. N Engl J Med. 2002;347:709–15.
Baldini I, Casagrande BP, Estadella D. Depression and obesity among females, are sex specificities considered? Arch Womens Ment Health. 2021;24:851–66.
Czepczor-Bernat K, Modrzejewska A, Modrzejewska J, Pękała M. A preliminary study of body image and depression among adults during COVID-19: a moderation model. Arch Psychiatr Nurs. 2022;36:55–61.
Cohen GJ. Helping children and families deal with divorce and separation. Pediatrics. 2002;110:1019–23.
Moazzami K, Lima BB, Sullivan S, Shah A, Bremner JD, Vaccarino V. Independent and joint association of obesity and metabolic syndrome with depression and inflammation. Health Psychol. 2019;38:586–95.
Ouchi N, Parker JL, Lugus JJ, Walsh K. Adipokines in inflammation and metabolic disease. Nat Rev Immunol. 2011;11:85–97.
Rosenblat JD, Cha DS, Mansur RB, McIntyre RS. Inflamed moods: a review of the interactions between inflammation and mood disorders. Prog Neuropsychopharmacol Biol Psychiatry. 2014;53:23–34.
Hamer M, Batty GD, Kivimaki M. Risk of future depression in people who are obese but metabolically healthy: the English longitudinal study of ageing. Mol Psychiatry. 2012;17:940–5.
Jackson SE, Beeken RJ, Wardle J. Obesity, perceived weight discrimination, and psychological well-being in older adults in England. Obesity. 2015;23:1105–11.
Le Thuc O, García-Cáceres C. Obesity-induced inflammation: connecting the periphery to the brain. Nat Metab. 2024;6:1237–52.
Milaneschi Y, Lamers F, Bot M, Drent ML, Penninx BW. Leptin dysregulation is specifically associated with major depression with atypical features: evidence for a mechanism connecting obesity and depression. Biol Psychiatry. 2017;81:807–14.
Tsai SY, Chung KH, Wu JY, Kuo CJ, Lee HC, Huang SH. Inflammatory markers and their relationships with leptin and insulin from acute mania to full remission in bipolar disorder. J Affect Disord. 2012;136:110–6.
Selman A, Dai J, Driskill J, Reddy AP, Reddy PH. Depression and obesity: focus on factors and mechanistic links. Biochim Biophys Acta Mol Basis Dis. 2025;1871:167561.
Keller J, Gomez R, Williams G, Lembke A, Lazzeroni L, Murphy GM, et al. HPA axis in major depression: cortisol, clinical symptomatology and genetic variation predict cognition. Mol Psychiatry. 2017;22:527–36.
Pan A, Keum N, Okereke OI, Sun Q, Kivimaki M, Rubin RR, et al. Bidirectional association between depression and metabolic syndrome: a systematic review and meta-analysis of epidemiological studies. Diabetes Care. 2012;35:1171–80.
Park SH, Yu HY. How useful is the center for epidemiologic studies depression scale in screening for depression in adults? An updated systematic review and meta-analysis. Psychiatry Res. 2021;302:114037.
Cooney LG, Milman LW, Hantsoo L, Kornfield S, Sammel MD, Allison KC, et al. Cognitive-behavioral therapy improves weight loss and quality of life in women with polycystic ovary syndrome: a pilot randomized clinical trial. Fertil Steril. 2018;110:161–71.e1.
Liu C, Wang C, Guan S, Liu H, Wu X, Zhang Z, et al. The prevalence of metabolically healthy and unhealthy obesity according to different criteria. Obes Facts. 2019;12:78–90.
Mehrabi F, Amiri P, Cheraghi L, Kheradmand A, Hosseinpanah F, Azizi F. Emotional states of different obesity phenotypes: a sex-specific study in a west-Asian population. BMC Psychiatry. 2021;21:124.
Kim SR, Kim HN, Song SW. Associations between mental health, quality of life, and obesity/metabolic risk phenotypes. Metab Syndr Relat Disord. 2020;18:347–52.
Kim MH, Chang Y, Jung HS, Shin H, Ryu S. Impact of self-rated health on progression to a metabolically unhealthy phenotype in metabolically healthy obese and non-obese individuals. J Clin Med. 2019;8:34.
Hinnouho GM, Singh-Manoux A, Gueguen A, Matta J, Lemogne C, Goldberg M, et al. Metabolically healthy obesity and depressive symptoms: 16-year follow-up of the Gazel cohort study. PLoS ONE. 2017;12:e0174678.
Yang Y, Herting JR, Choi J. Obesity, metabolic abnormality, and health-related quality of life by gender: a cross-sectional study in Korean adults. Qual Life Res. 2016;25:1537–48.
Phillips CM, Perry IJ. Depressive symptoms, anxiety and well-being among metabolic health obese subtypes. Psychoneuroendocrinology. 2015;62:47–53.
Jokela M, Hamer M, Singh-Manoux A, Batty GD, Kivimäki M. Association of metabolically healthy obesity with depressive symptoms: pooled analysis of eight studies. Mol Psychiatry. 2014;19:910–4.
Acknowledgements
We are very grateful to the editor and anonymous reviewers for their constructive comments.
Funding
This work was supported by National Training Program of Innovation and Entrepreneurship for Undergraduates (grant number 202110555106); The Key Research and Development Projects of Hunan Province (grant number 2020SK51826); Scientific research project of Hunan Provincial Health Commission (grant number 202218014518); Hunan Provincial Innovation Foundation For Postgraduate (grant number CX20221011); and Clinical Research 4310 Program of the First Affiliated Hospital of University of South China (grant number 20224310NHYCG03).
Author information
Authors and Affiliations
Contributions
JD: conceptualization, data curation, formal analysis, writing of original draft, and writing of review and editing. LH: data curation, writing of review and editing. LZ: formal analysis, writing of review and editing. JW, QF and RD: data curation and formal analysis. YL and YJ: formal analysis and writing of review. XX: writing of review and editing. HZ: conceptualization, writing of review and editing.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Deng, J., He, L., Zhang, L. et al. The association between metabolically healthy obesity and risk of depression: a systematic review and meta-analysis. Int J Obes 49, 980–991 (2025). https://doi.org/10.1038/s41366-025-01741-5
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41366-025-01741-5