Abstract
Background
Attention deficit hyperactivity disorder (ADHD) has been linked to excessive weight; however, the underlying mechanisms of this association are not well understood. To date, the bidirectional associations between ADHD and nutritional status in childhood have been explored in a limited number of studies, with particularly few of those incorporating body composition data. This study aims to evaluate the associations of ADHD symptoms, nutritional status, and body composition in childhood.
Methods
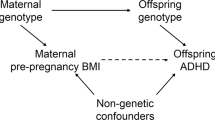
We analyzed data from 3940 children from the 2015 Pelotas (Brazil) Birth Cohort at 4 and 6–7 years of age. Linear regression was performed to evaluate the association between ADHD symptoms and nutritional status (weight, height, and body mass index [BMI]) at ages 4 and 6–7, as well as body composition, specifically fat mass (FF) and fat-free mass (FFM) at ages 6–7. Moreover, a cross-lagged panel model (CLPM) analysis between ADHD symptoms and BMI was performed to explore the bidirectional associations.
Results
ADHD symptoms were associated with increased height (β 0.01, 95%CI 0.001, 0.026) and FFM (β 0.02, 95%CI 0.008–0.035) at age 4, and increased BMI (β0.02, 95%IC 0.002, 0.038), weight (β 0. 02, 95%CI 0.005, 0.039), height (β 0.01, 95%CI 0.000, 0.024), and FFM (β 0.02, 95%CI 0.012, 0.040) at ages 6–7. Although the CLPM indicated a small effect suggesting a bidirectional relationship between ADHD symptoms and BMI, the observed associations were not statistically significant: ADHD scores at age 4 predicting BMI z-scores at ages 6–7 (β 0.003; 95% CI: –0.026, 0.020), and BMI z-scores at age 4 predicting ADHD scores at ages 6–7 (β 0.013; 95% CI: –0.018, 0.044).
Conclusion
Children with higher ADHD symptoms showed increased growth in weight, height, and BMI. The observed increase in weight and BMI was attributed to greater FFM in these children.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated and analyzed during this study are not publicly available due to confidentiality and data protection commitments to the participants. However, they can be obtained from the corresponding author upon reasonable request.
References
APA AAP. DSM-5: Diagnostic and Statistical Manual of Mental Disorders. Artmed Publisher.
Faraone SV. The pharmacology of amphetamine and methylphenidate: Relevance to the neurobiology of attention-deficit/hyperactivity disorder and other psychiatric comorbidities. Neurosci Biobehav Rev. 2018;87:255–70.
Swanson JM, Arnold LE, Molina BSG, Sibley MH, Hechtman LT, Hinshaw SP, et al. Young adult outcomes in the follow-up of the Multimodal Treatment Study of Attention-Deficit/Hyperactivity Disorder: symptom persistence, source discrepancy and height Suppression. J Child Psychol Psychiatry. 2017;58:663–78.
Cortese S, Moreira-Maia CR, St Fleur D, Morcillo-Peñalver C, Rohde LA, Faraone SV. Association between ADHD and obesity: a systematic review and meta-analysis. Am J Psychiatry. 2016;173:34–43.
Turan S, Tunctürk M, Çıray RO, Halaç E, Ermiş Ç. ADHD and risk of childhood adiposity: a review of recent research. Curr Nutr Rep. 2021;10:30–46.
Erhart M, Herpertz-Dahlmann B, Wille N, Sawitzky-Rose B, Hölling H, Ravens-Sieberer U. Examining the relationship between attention-deficit/hyperactivity disorder and overweight in children and adolescents. Eur Child Adolesc Psychiatry. 2012;21:39–49.
Waring ME, Lapane KL. Overweight in children and adolescents in relation to attention-deficit/hyperactivity disorder: results from a national sample. Pediatrics. 2008;122:e1–e6.
Bowling AB, Tiemeier HW, Jaddoe VWV, Barker ED, Jansen PW. ADHD symptoms and body composition changes in childhood: a longitudinal study evaluating directionality of associations. Pediatr Obes. 2018;13:567–75.
Porter PA, Henry LN, Halkett A, Hinshaw SP. Body mass indices of girls with and without ADHD: developmental trajectories from childhood to adulthood. J Clin Child Adolesc Psychol. 2022;51:688–700.
Cortese S, Ramos Olazagasti MA, Klein RG, Castellanos FX, Proal E, Mannuzza S. Obesity in men with childhood ADHD: a 33-year controlled, prospective, follow-up study. Pediatrics. 2013;131:e1731–1738.
Khalife N, Kantomaa M, Glover V, Tammelin T, Laitinen J, Ebeling H, et al. Childhood attention-deficit/hyperactivity disorder symptoms are risk factors for obesity and physical inactivity in adolescence. J Am Acad Child Adolesc Psychiatry. 2014;53:425–36.
Martins-Silva T, Dos Santos Vaz J, Schäfer JL, Salum GA, Carpena MX, Vitola ES, et al. ADHD in childhood predicts BMI and body composition measurements over time in a population-based birth cohort. Int J Obes 2005. 2022;46:1204–11.
Adamczak M, Wiecek A. The adipose tissue as an endocrine organ. Adipose Tissue Endocr Organ. 2013;33:2–13.
Özcan Ö, Arslan M, Güngör S, Yüksel T, Selimoğlu MA. Plasma leptin, adiponectin, neuropeptide y levels in drug naive children with ADHD. J Atten Disord. 2015;22:896–900.
Levitan RD, Masellis M, Lam RW, Muglia P, Basile VS, Jain U, et al. Childhood inattention and dysphoria and adult obesity associated with the dopamine D4 receptor gene in overeating women with seasonal affective disorder. Neuropsychopharmacology. 2004;29:179–86.
Choudhry Z, Sengupta SM, Grizenko N, Harvey WJ, Fortier M-È, Schmitz N, et al. Body weight and ADHD: examining the role of self-regulation. PloS One. 2013;8:e55351.
Comings DE, Blum K (2000) Reward deficiency syndrome: genetic aspects of behavioral disorders. In: Prog. Brain Res. Elsevier, pp 325-41
Martins-Silva T, Vaz JDS, Genro JP, Hutz MH, Loret de Mola C, Mota NR, et al. Obesity and ADHD: Exploring the role of body composition, BMI polygenic risk score, and reward system genes. J Psychiatr Res. 2021;136:529–36.
Cortese S, Vincenzi B (2011) Obesity and ADHD: Clinical and Neurobiological Implications. In: Stanford C, Tannock R (eds) Behav. Neurosci. Atten. Deficit Hyperact. Disord. Its Treat. Springer Berlin Heidelberg, Berlin, Heidelberg, pp 199–218.
Pérez-Bonaventura I, Granero R, Ezpeleta L. The relationship between weight status and emotional and behavioral problems in Spanish preschool children. J Pediatr Psychol. 2015;40:455–63.
Ebenegger V, Marques-Vidal P-M, Munsch S, Quartier V, Nydegger A, Barral J, et al. Relationship of hyperactivity/inattention with adiposity and lifestyle characteristics in preschool children. J Child Neurol. 2012;27:852–8.
Cortese S, Comencini E, Vincenzi B, Speranza M, Angriman M. Attention-deficit/hyperactivity disorder and impairment in executive functions: a barrier to weight loss in individuals with obesity? BMC Psychiatry. 2013;13:286–286.
Merrill BM, Morrow AS, Sarver D, Sandridge S, Lim CS. Prevalence and correlates of attention-deficit hyperactivity disorder in a diverse, treatment-seeking pediatric overweight/obesity sample. J Dev Behav Pediatr JDBP. 2021;42:433–41.
Brazilian Institute of Geography and Statistics (IBGE). Pelotas (RS) | Cities and States. Available from: https://www.ibge.gov.br/cidades-e-estados/rs/pelotas.html. Accessed 14 May 2024.
Hallal PC, Bertoldi AD, Domingues MR, Da Silveira MF, Demarco FF, Da Silva ICM, et al. Cohort Profile: The 2015 Pelotas (Brazil) Birth Cohort Study. Int J Epidemiol. 2018;47:1048–1048h.
Murray J, Leão OAA, Flores TR, Demarco FF, Tovo-Rodrigues L, Oliveira IO, et al. Cohort Profile Update: 2015 Pelotas (Brazil) Birth Cohort Study–follow-ups from 2 to 6–7 years, with COVID-19 impact assessment. Int J Epidemiol. 2024;53:dyae048.
Fleitlich-Bilyk B, Goodman R. Prevalence of child and adolescent psychiatric disorders in southeast Brazil. J Am Acad Child Adolesc Psychiatry. 2004;43:727–34.
Brazilian Association of Research Companies (ABEP). Available from: https://www.abep.org/. Accessed May 26, 2024.
Kearney M. Cross-Lagged Panel Analysis. 2017.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inf. 2009;42:377–81.
Kim EJ, Kwon HJ, Ha M, Lim MH, Oh SY, Kim JH, et al. Relationship among attention-deficit hyperactivity disorder, dietary behaviours and obesity. Child Care Health Dev. 2014;40:698–705.
van Egmond-Fröhlich AWA, Widhalm K, de Zwaan M. Association of symptoms of attention-deficit/hyperactivity disorder with childhood overweight adjusted for confounding parental variables. Int J Obes 2005. 2012;36:963–8.
Reilly JJ, Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int J Obes. 2011;35:891–8.
Hanc T, Slopien A, Wolanczyk T, Szwed A, Czapla Z, Durda M, et al. Attention-deficit/hyperactivity disorder is related to decreased weight in the preschool period and to increased rate of overweight in school-age boys. J Child Adolesc Psychopharmacol. 2015;25:691–700.
Rojo-Marticella M, Arija V, Morales-Hidalgo P, Esteban-Figuerola P, Voltas-Moreso N, Canals-Sans J. Anthropometric status of preschoolers and elementary school children with ADHD: preliminary results from the EPINED study. Pediatr Res. 2023;94:1570–8.
Sha’ari N, Manaf ZA, Ahmad M, Rahman FNA. Nutritional status and feeding problems in pediatric attention deficit-hyperactivity disorder. Pediatr Int J Jpn Pediatr Soc. 2017;59:408–15.
Namimi-Halevi C, Dor C, Dichtiar R, Bromberg M, Sinai T. Attention-deficit hyperactivity disorder is associated with relatively short stature among adolescents. Acta Paediatr. 2023;112:779–86.
Davallow Ghajar L, DeBoer MD. Children with attention-deficit/hyperactivity disorder are at increased risk for slowed growth and short stature in early childhood. Clin Pediatr Philos. 2020;59:401–10.
Heinonen K, Räikkönen K, Pesonen A-K, Andersson S, Kajantie E, Eriksson JG, et al. Trajectories of growth and symptoms of attention-deficit/hyperactivity disorder in children: a longitudinal study. BMC Pediatr. 2011;11:84.
Dubnov-Raz G, Perry A, Berger I. Body mass index of children with attention-deficit/hyperactivity disorder. J Child Neurol. 2011;26:302–8.
Tashakori A, Riahi K, Afkandeh R, Ayati AH. Comparison of Height and Weight of 5-6 Year-old Boys with Attention Deficit Hyperactivity Disorder (ADHD) and Non-ADHD. Iran J Psychiatry Behav Sci. 2011;5:71–75.
Hanc T, Cieslik J, Wolanczyk T, Gajdzik M. Assessment of growth in pharmacological treatment-naïve Polish boys with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol. 2012;22:300–6.
Alpaslan AH, Ucok K, Coşkun KŞ, Genc A, Karabacak H, Guzel HI. Resting metabolic rate, pulmonary functions, and body composition parameters in children with attention deficit hyperactivity disorder. Eat Weight Disord EWD. 2017;22:91–96.
Tandon PS, Sasser T, Gonzalez ES, Whitlock KB, Christakis DA, Stein MA. Physical activity, screen time, and sleep in children with ADHD. J Phys Act Health. 2019;16:416–22.
Skinner AM, Vlachopoulos D, Barker AR, Moore SA, Rowlands AV, Soininen S, et al. Physical activity volume and intensity distribution in relation to bone, lean and fat mass in children. Scand J Med Sci Sports. 2023;33:267–82.
Papadopoulou SK, Feidantsis KG, Hassapidou MN, Methenitis S. The specific impact of nutrition and physical activity on adolescents’ body composition and energy balance. Res Q Exerc Sport. 2021;92:736–46.
Escobar-Cardozo GD, Correa-Bautista JE, González-Jiménez E, Schmidt-RioValle J, Ramírez-Vélez R. Percentiles of body fat measured by bioelectrical impedance in children and adolescents from Bogotá (Colombia): the FUPRECOL study. Arch Argent Pediatr. 2016;114:135–42.
Kurtoglu S, Mazicioglu MM, Ozturk A, Hatipoglu N, Cicek B, Ustunbas HB. Body fat reference curves for healthy Turkish children and adolescents. Eur J Pediatr. 2010;169:1329–35.
Plachta-Danielzik S, Gehrke MI, Kehden B, Kromeyer-Hauschild K, Grillenberger M, Willhöft C, et al. Body fat percentiles for german children and adolescents. Obes Facts. 2012;5:77–90.
Amaral MA, Mundstock E, Scarpatto CH, Cañon-Montañez W, Mattiello R. Reference percentiles for bioimpedance body composition parameters of healthy individuals: A cross-sectional study. Clinics. 2022;77:100078.
van Mil NH, Steegers-Theunissen RPM, Motazedi E, Jansen PW, Jaddoe VWV, Steegers EAP, et al. Low and high birth weight and the risk of child attention problems. J Pediatr. 2015;166:862–9.e1–3.
Leventakou V, Herle M, Kampouri M, Margetaki K, Vafeiadi M, Kogevinas M, et al. The longitudinal association of eating behaviour and ADHD symptoms in school age children: a follow-up study in the RHEA cohort. Eur Child Adolesc Psychiatry. 2022;31:511–7.
Acknowledgements
This article is based on data from the study “Pelotas Birth Cohort, 2015” conducted by the Postgraduate Program in Epidemiology at Universidade Federal de Pelotas, with the collaboration of the Brazilian Public Health Association (ABRASCO). The first phase of the 2015 Pelotas (Brazil) Birth Cohort was funded by the Wellcome Trust (095582). Funding for specific follow-up visits was also received from the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) and Fundação de Amparo a Pesquisa do Estado do Rio Grande do Sul (FAPERGS), Bernard van Leer Foundation (BRA-2018-178) and Department of Science and Technology (DECIT/Brazilian Ministry of Health) for the 4-year follow-up. The 6–7 years follow-up received funding from the Department of Science and Technology of the Ministry of Health (Department of Science and Technology (DECIT/Brazilian Ministry of Health), Instituto Todos Pela Saúde, Celer Biotecnologia SA, FAPERGS PqG 21/2551-0002004 -0 and CNPq through public notices: 407813/2021-7, 406582/2021-1 and 406582/2021-1. This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES) - Finance Code 001.
Author information
Authors and Affiliations
Contributions
BPG, TM-S, LT-R, and ADB conceived the study and conducted the analyses. BPG drafted the initial version of the manuscript. BPG, TM-S, IB, JM, MRD, PCH, LT-R and ADB critically revised the manuscript and contributed to the interpretation of the findings. All authors approved the final version for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gonçalves, B.P., Martins-Silva, T., Bierhals, I. et al. Exploring the bidirectional associations of ADHD symptomatology, nutritional status, and body composition in childhood: evidence from a Brazilian Birth Cohort Study. Int J Obes 49, 965–972 (2025). https://doi.org/10.1038/s41366-025-01745-1
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41366-025-01745-1