Abstract
Background
Obesity is a major public health concern affecting millions of people globally. Early identification of individuals susceptible to obesity is crucial for reducing the burden of obesity. Obesity is often defined based on body-mass-index (BMI), and tracking BMI trajectories from early childhood offers a valuable tool for risk stratification. Although the role of mothers in shaping these trajectories is well-recognized, the paternal influence on childhood obesity development remains a knowledge gap. We hypothesize that children of fathers with obesity have higher odds of being in the rapid BMI growth trajectory with stronger estimates when the mother is also with overweight or obesity.
Methods
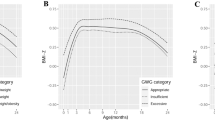
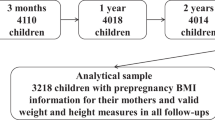
We analyzed data from the Canadian CHILD Cohort Study, a pregnancy cohort in which both parents were enrolled in early pregnancy when BMI was assessed. The child’s BMI was repeatedly collected from birth to age five. We used group-based trajectory modeling to identify offspring BMI z-score (BMIz) trajectory groups (age-and-sex standardized) and weighted multinomial logistic regression analysis to determine the associations between prenatal paternal BMI and offspring growth trajectories, stratified by maternal weight categories.
Results
Among 2 238 participants, the mean prenatal paternal BMI was 27.44 (SD = 4.77), and 22.83% of fathers were with obesity. The four identified offspring BMIz trajectories were: low stable (n = 220, 9.83%), normative (n = 1 356, 60.59%), high stable (n = 572, 25.56%), and rapid BMIz growth trajectory (n = 90, 4.02%). Children of normal-weight mothers and fathers with obesity had 1.86 higher odds (OR: 1.86; 95%CI: 1.22–2.84) of being classified in the rapid growth BMIz trajectory, compared to children of normal-weight fathers. The odds of being in the rapid growth BMIz trajectory were higher when both mothers and fathers were with obesity (OR: 4.35; 95%CI: 2.65–7.14).
Conclusions
Children of fathers with obesity had higher odds of being in the rapid BMI growth trajectory, particularly when also the mother was with overweight or obesity. These results support the need for preconception advice and interventions for couples to optimize their offspring’s health.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
A list of variables available in the CHILD Cohort Study is available at https://childstudy.ca/for-researchers/study-data/. Researchers interested in collaborating on a project and accessing CHILD Cohort Study data should contact the Study’s National Coordinating Centre (NCC) to discuss their needs before initiating a formal request. To contact the NCC, please email child@mcmaster.ca. More information about data access for the CHILD Cohort Study can be found at https://childstudy.ca/for-researchers/data-access/.
References
World Health Organization. Obesity and Overweight. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (World Health Organization, 2024).
Umer A, Kelley GA, Cottrell LE, Giacobbi P, Innes KE, Lilly CL. Childhood obesity and adult cardiovascular disease risk factors: a systematic review with meta-analysis. BMC Public Health. 2017;17:683.
Llewellyn A, Simmonds M, Owen CG, Woolacott N. Childhood obesity as a predictor of morbidity in adulthood: a systematic review and meta-analysis. Obes Rev J Int Assoc Study Obes. 2016;17:56–67.
Péneau S, Giudici KV, Gusto G, Goxe D, Lantieri O, Hercberg S, et al. Growth trajectories of body mass index during childhood: associated factors and health outcome at adulthood. J Pediatr. 2017;186:64–71.e1.
Araújo J, Severo M, Barros H, Mishra GD, Guimarães JT, Ramos E. Developmental trajectories of adiposity from birth until early adulthood and association with cardiometabolic risk factors. Int J Obes 2005. 2015;39:1443–9.
Ahanchi NS, Ramezankhani A, Munthali RJ, Asgari S, Azizi F, Hadaegh F. Body mass index trajectories from adolescent to young adult for incident high blood pressure and high plasma glucose. PLOS ONE. 2019;14:e0213828.
Reyna ME, Petersen C, Dai DLY, Dai R, Becker AB, Azad MB, et al. Longitudinal body mass index trajectories at preschool age: children with rapid growth have differential composition of the gut microbiota in the first year of life. Int J Obes. 2022;46:1351–8.
Barker DJ. The fetal and infant origins of adult disease. BMJ. 1990;301:1111.
Heslehurst N,Vieira R,Akhter Z,Bailey H, Slack E,Ngongalah L, et al. The association between maternal body mass index and child obesity: a systematic review and meta-analysis. PLOS Med. 2019;16:e1002817.
Baidal JAW, Locks LM, Cheng ER, Blake-Lamb TL, Perkins ME, Taveras EM. Risk factors for childhood obesity in the first 1000 days: a systematic review. Am J Prev Med. 2016;50:761–79.
Hunt KJ, Ferguson PL, Neelon B, Commodore S, Bloom MS, Sciscione AC, et al. The association between maternal pre-pregnancy BMI, gestational weight gain and child adiposity: a racial-ethnically diverse cohort of children. Pediatr Obes. 2022;17:e12911.
Gete DG, Waller M, Mishra GD. Pre-pregnancy diet quality is associated with lowering the risk of offspring obesity and underweight: finding from a prospective cohort study. Nutrients. 2021;13:1044.
Linabery AM, Nahhas RW, Johnson W, Choh AC, Towne B, Odegaard AO, et al. Stronger influence of maternal than paternal obesity on infant and early childhood body mass index: the Fels Longitudinal Study. Pediatr Obes. 2013;8:159–69.
Gaillard R, Steegers EAP, Duijts L, Felix JF, Hofman A, Franco OH, et al. Childhood cardiometabolic outcomes of maternal obesity during pregnancy: the Generation R Study. Hypertens Dallas Tex 1979. 2014;63:683–91.
Voerman E, Santos S, Patro Golab B, Amiano P, Ballester F, Barros H, et al. Maternal body mass index, gestational weight gain, and the risk of overweight and obesity across childhood: An individual participant data meta-analysis. PLoS Med. 2019;16:e1002744.
Sharp GC, Lawlor DA. Paternal impact on the life course development of obesity and type 2 diabetes in the offspring. Diabetologia. 2019;62:1802–10.
Soubry A, Guo L, Huang Z, Hoyo C, Romanus S, Price T, et al. Obesity-related DNA methylation at imprinted genes in human sperm: results from the TIEGER study. Clin Epigenet. 2016;8:51.
Soubry A, Murphy SK, Wang F, Huang Z, Vidal AC, Fuemmeler BF, et al. Newborns of obese parents have altered DNA methylation patterns at imprinted genes. Int J Obes 2005. 2015;39:650–7.
Potabattula R, Dittrich M, Schorsch M, Hahn T, Haaf T, El Hajj N. Male obesity effects on sperm and next-generation cord blood DNA methylation. PLoS ONE. 2019;14:e0218615.
Soubry A, Schildkraut JM, Murtha A, Wang F, Huang Z, Bernal A, et al. Paternal obesity is associated with IGF2hypomethylation in newborns: results from a Newborn Epigenetics Study (NEST) cohort. BMC Med. 2013;11:29.
Billah MM, Khatiwada S, Morris MJ, Maloney CA. Effects of paternal overnutrition and interventions on future generations. Int J Obes 2005. 2022;46:901–17. May
Tomar A, Gomez-Velazquez M, Gerlini R, Comas-Armangué G, Makharadze L, Kolbe T, et al. Epigenetic inheritance of diet-induced and sperm-borne mitochondrial RNAs. Nature. 2024;630:1–8.
Kaati G, Bygren LO, Edvinsson S. Cardiovascular and diabetes mortality determined by nutrition during parents’ and grandparents’ slow growth period. Eur J Hum Genet. 2002;10:682–8.
Li J, Yang Q, An R, Sesso HD, Zhong VW, Chan KHK, et al. Famine and trajectories of body mass index, waist circumference, and blood pressure in two generations: results from the CHNS from 1993-2015. Hypertension. 2022;79:518–31.
Yao WY, Li L, Jiang HR, Yu YF, Xu WH. Transgenerational associations of parental famine exposure in early life with offspring risk of adult obesity in China. Obesity. 2023;31:279–89.
Ng SF, Lin RCY, Laybutt DR, Barres R, Owens JA, Morris MJ. Chronic high-fat diet in fathers programs β-cell dysfunction in female rat offspring. Nature. 2010;467:963–6.
Carone BR, Fauquier L, Habib N, Shea JM, Hart CE, Li R, et al. Paternally induced transgenerational environmental reprogramming of metabolic gene expression in mammals. Cell. 2010;143:1084–96.
Watkins AJ, Dias I, Tsuro H, Allen D, Emes RD, Moreton J, et al. Paternal diet programs offspring health through sperm- and seminal plasma-specific pathways in mice. Proc Natl Acad Sci USA. 2018;115:10064–9.
Watkins AJ, Sinclair KD. Paternal low protein diet affects adult offspring cardiovascular and metabolic function in mice. Am J Physiol-Heart Circ Physiol. 2014;306:H1444–52.
de Castro Barbosa T, Ingerslev LR, Alm PS, Versteyhe S, Massart J, Rasmussen M, et al. High-fat diet reprograms the epigenome of rat spermatozoa and transgenerationally affects metabolism of the offspring. Mol Metab. 2016;5:184–97.
Northstone K, Golding J, Davey Smith G, Miller LL, Pembrey M. Prepubertal start of father’s smoking and increased body fat in his sons: further characterisation of paternal transgenerational responses. Eur J Hum Genet. 2014;22:1382–6.
Miliku K, Bergen NE, Bakker H, Hofman A, Steegers EAP, Gaillard R, et al. Associations of maternal and paternal blood pressure patterns and hypertensive disorders during pregnancy with childhood blood pressure. J Am Heart Assoc Cardiovasc Cerebrovasc Dis. 2016;5:e003884.
Deveci AC, Keown-Stoneman CDG, Maguire JL, O’Connor DL, Anderson LN, Dennis CL, et al. Paternal BMI in the preconception period, and the association with child zBMI. Int J Obes. 2023;47:1–8.
Subbarao P, Anand SS, Becker AB, Befus AD, Brauer M, Brook JR, et al. The Canadian Healthy Infant Longitudinal Development (CHILD) study: examining developmental origins of allergy and asthma. Thorax. 2015;70:998–1000.
World Health Organization. A Healthy Lifestyle—WHO Recommendations. https://www.who.int/europe/news-room/fact-sheets/item/a-healthy-lifestyle---who-recommendations (World Health Organization, 2010).
Bridgman SL, Azad MB, Persaud RR, Chari RS, Becker AB, Sears MR, et al. Impact of maternal pre‐pregnancy overweight on infant overweight at 1 year of age: associations and sex‐specific differences. Pediatr Obes. 2018;13:579–89.
WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr. 2006;450:76–85.
de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85:660–7.
Takaro TK, Scott JA, Allen RW, Anand SS, Becker AB, Befus AD, et al. The Canadian Healthy Infant Longitudinal Development (CHILD) birth cohort study: assessment of environmental exposures. J Expo Sci Environ Epidemiol. 2015;25:580–92.
Kelemen LE, Anand SS, Vuksan V, Yi Q, Teo KK, Devanesen S, et al. Development and evaluation of cultural food frequency questionnaires for South Asians, Chinese, and Europeans in North America. J Am Diet Assoc. 2003;103:1178–84.
Buuren Svan, Groothuis-Oudshoorn K. mice: multivariate imputation by chained equations in R. J Stat Softw. 2011;45:1–67.
Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B Methodol. 1995;57:289–300.
Simmonds M, Burch J, Llewellyn A, Griffiths C, Yang H, Owen C, et al. The use of measures of obesity in childhood for predicting obesity and the development of obesity-related diseases in adulthood: a systematic review and meta-analysis. NIHR J. Library; 2015.
Regnault N, Botton J, Forhan A, Hankard R, Thiebaugeorges O, Hillier TA, et al. Determinants of early ponderal and statural growth in full-term infants in the EDEN mother-child cohort study. Am J Clin Nutr. 2010;92:594–602.
Fleten C, Nystad W, Stigum H, Skjaerven R, Lawlor DA, Davey Smith G, et al. Parent-offspring body mass index associations in the Norwegian mother and child cohort study: a family-based approach to studying the role of the intrauterine environment in childhood adiposity. Am J Epidemiol. 2012;176:83–92.
Murrin CM, Kelly GE, Tremblay RE, Kelleher CC. Body mass index and height over three generations: evidence from the lifeways cross-generational cohort study. BMC Public Health. 2012;12:81.
Durmuş B, Arends LR, Ay L, Hokken-Koelega AC, Raat H, Hofman A, et al. Parental anthropometrics, early growth and the risk of overweight in pre-school children: the generation R study: parental and childhood anthropometrics. Pediatr Obes. 2013;8:339–50.
Lawlor DA, Smith GD, O’Callaghan M, Alati R, Mamun AA, Williams GM, et al. Epidemiologic evidence for the fetal overnutrition hypothesis: findings from the mater-university study of pregnancy and its outcomes. Am J Epidemiol. 2007;165:418–24.
Petersen TL, Møller LB, Brønd JC, Jepsen R, Grøntved A. Association between parent and child physical activity: a systematic review. Int J Behav Nutr Phys Act. 2020;17:67.
Rhodes RE, Perdew M, Malli S. Correlates of parental support of child and youth physical activity: a systematic review. Int J Behav Med. 2020;27:636–46.
Matos R, Monteiro D, Amaro N, Antunes R, Coelho L, Mendes D, et al. Parents’ and children’s (6–12 years old) physical activity association: a systematic review from 2001 to 2020. Int J Environ Res Public Health. 2021;18:12651.
Su DLY, Tang TCW, Chung JSK, Lee ASY, Capio CM, Chan DKC. Parental influence on child and adolescent physical activity level: a meta-analysis. Int J Environ Res Public Health. 2022;19:16861.
Huang RC, de Klerk NH, Smith A, Kendall GE, Landau LI, Mori TA, et al. Lifecourse childhood adiposity trajectories associated with adolescent insulin resistance. Diabetes Care. 2011;34:1019–25.
Zhang T, Xu J, Li S, Bazzano LA, He J, Whelton PK, et al. Trajectories of childhood BMI and adult diabetes: the Bogalusa Heart Study. Diabetologia. 2019;62:70–7.
Corder K, Winpenny EM, Foubister C, Guagliano JM, Hartwig XM, Love R, et al. Becoming a parent: a systematic review and meta-analysis of changes in BMI, diet, and physical activity. Obes Rev J Int Assoc Study Obes. 2020;21:e12959.
Lo BK, Kang AW, Haneuse S, Yu X, Ash Tvon, Redline S, et al. Changes in fathers’ Body Mass Index, sleep, and diet from prebirth to 12 months postbirth: exploring the moderating roles of parenthood experience and coparenting support. Ann Behav Med. 2021;55:1211–9.
Acknowledgements
We thank the CHILD Cohort Study participant families for their dedication and commitment to advancing health research. CHILD was initially funded by CIHR and AllerGen NCE. Visit CHILD at www.childstudy.ca.
Funding
This work was funded from a CIHR Operating Grant; Ontario Regional Centre of the Canadian Statistical Sciences Institute, the Connaught New Investigator Award, and the University of Toronto Pathway Grants (KM). PS holds a Tier 1 Canada Research Chair in Pediatric Asthma and Lung Health. SET holds a Tier 1 Canada Research Chair in Pediatric Precision Health and the Aubrey J. Tingle Professor of Pediatric Immunology. ZL holds an Early Career Researcher Award in Asthma. The authors report no conflicts of interest related to the study.
Author information
Authors and Affiliations
Contributions
The authors’ responsibilities were as follows—KM designed and managed the project; PJM, ES, SET, TJM and PS conceived the CHILD cohort design, managed study recruitment, and oversaw clinical assessments of study participants; AR conducted all the statistical analyses, and ZHC, MA, MER, ZL and KM oversaw the statistical analyses; AR and KM interpreted the data and wrote the manuscript; all authors (AR, ZHC, MA, SSC, MER, KD, DJ, DO, AE, PJM, ES, SET, TJM, ZL, PS, and KM) provided feedback and read and approved the final manuscript. AR and ZHC have full access to the data in the study.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rossi, A., Chen, Z.H., Ahmadiankalati, M. et al. Determining the interplay of prenatal parental BMI in shaping child BMI trajectories: the CHILD Cohort Study. Int J Obes 49, 1608–1615 (2025). https://doi.org/10.1038/s41366-025-01792-8
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41366-025-01792-8