Abstract
Background
Previous intermittent fasting (IF) studies have reported inconsistent findings regarding its antihypertensive effects and safety.
Objective
This study aimed to assess the effects and safety of IF on blood pressure (BP), anthropometrics, and cardiometabolic risk markers in individuals with overweight or obesity compared to a no-intervention control group.
Methods
Relevant studies were retrieved from multiple databases, including CNKI, Wanfang, VIP, SinoMed, PubMed, Embase, the Cochrane Library, and Web of Science, up to April 30, 2024. A meta-analysis was performed using Stata version 18.0 and RevMan 5.4, calculating mean differences (MD) or risk ratios (RR) with 95% confidence intervals (CI) via the Knapp-Hartung modified random-effects model. Publication bias was evaluated using a contour-enhanced funnel plot and Egger’s test.
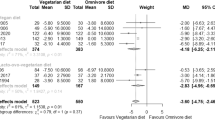
Results
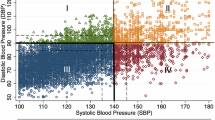
Fifteen studies (n = 929) were included. IF significantly reduced systolic blood pressure (SBP) (MD = –4.43 mmHg, 95% CI: –5.83 to –3.03, p < 0.001) and diastolic blood pressure (DBP) (MD = –2.00 mmHg, 95% CI: –3.23 to –0.78, p < 0.001) compared to control. IF also improved anthropometric measures, Homeostatic Model Assessment of Insulin Resistance (HOMA-IR), and Triglycerides (TG). Seven studies reported minor adverse effects. Although the IF group showed a higher risk of vomiting (RR = 1.11, 95% CI: 1.04–1.19, p = 0.01) and irritability (RR = 1.22, 95% CI: 1.13–1.31, p < 0.001) compared to the control group, these reactions were predominantly observed during the initial phase of the intervention and were self-resolving.
Conclusions
IF significantly lowered SBP and DBP in individuals with overweight or obesity, particularly in high-risk subgroups (obesity, age ≥45 years, and prehypertension/hypertension), with a favorable safety profile. Due to heterogeneity, future trials should standardize IF regimens and target these subgroups to confirm generalizability.
Clinical trial registration
The review protocol has been registered on PROSPERO (CRD42024540777).
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The original contributions presented in the study are included in the article; further inquiries can be directed to the corresponding authors.
References
WHO. Obesity and overweight [EB]. (2024-03-01)[2025-04-08]. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
WHO. Global report on hypertension: the race against a silent killer [EB]. (2023-09-19)[2025-04-08]. https://www.who.int/publications/i/item/9789240081062.
Shariq OA, McKenzie TJ. Obesity-related hypertension: a review of pathophysiology, management, and the role of metabolic surgery. Gland Surg. 2020;9:80–93.
Cherfan M, Vallée A, Kab S, Salameh P, Goldberg M, Zins M, et al. Unhealthy behaviors and risk of uncontrolled hypertension among treated individuals-The CONSTANCES population-based study. Sci Rep. 2020;10:1925.
Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. 2020;16:223–37.
Jiang YH, Zhang P, Tao Y, Liu Y, Cao G, Zhou L, et al. Banxia Baizhu Tianma decoction attenuates obesity-related hypertension. J Ethnopharmacol. 2021;266:113453.
Ryu S, Frith E, Pedisic Z, Kang M, Loprinzi PD. Secular trends in the association between obesity and hypertension among adults in the United States, 1999-2014. Eur J Intern Med. 2019;62:37–42.
Charchar FJ, Prestes PR, Mills C, Ching SM, Neupane D, Marques FZ, et al. Lifestyle management of hypertension: International Society of Hypertension position paper endorsed by the World Hypertension League and European Society of Hypertension. J Hypertens. 2024;42:23–49.
Bakris G, Ali W, Parati G. ACC/AHA versus ESC/ESH on hypertension guidelines: JACC guideline comparison. J Am Coll Cardiol. 2019;73:3018–26.
Patikorn C, Roubal K, Veettil SK, Chandran V, Pham T, Lee YY, et al. Intermittent fasting and obesity-related health outcomes. JAMA Netw Open. 2021;4:e2139558.
Al-Jafar R, Zografou Themeli M, Zaman S, Akbar S, Lhoste V, Khamliche A, et al. Effect of religious fasting in Ramadan on blood pressure: results from LORANS (London Ramadan Study) and a meta‐analysis. J Am Heart Assoc. 2021;10:e021560.
Liu L, Chen W, Wu D, Hu F. Metabolic efficacy of time-restricted eating in adults: a systematic review and meta-analysis of randomized controlled trials. J Clin Endocrinol Metab. 2022;107:3428–41.
Silverii GA, Cresci B, Benvenuti F, Santagiuliana F, Rotella F, Mannucci E. Effectiveness of intermittent fasting for weight loss in individuals with obesity: A meta-analysis of randomized controlled trials. Nutr Metab Cardiovas. 2023;33:1481–9.
Harris L, Hamilton S, Azevedo LB, Olajide J, De Brún C, Waller G, et al. Intermittent fasting interventions for treatment of overweight and obesity in adults: a systematic review and meta-analysis. JBI Database Syst Rev Implement Rep. 2018;16:507–47.
Chen W, Liu X, Bao L, Yang P, Zhou H. Health effects of the time-restricted eating in adults with obesity: a systematic review and meta-analysis. Front Nutr. 2023;10:1079250.
Lin YJ, Wang YT, Chan LC, Chu NF. Effect of time-restricted feeding on body composition and cardio-metabolic risk in middle-aged women in Taiwan. Nutrition 2022;93:111504.
Abstracts from the American Heart Association Epidemiology and Prevention|Lifestyle and Cardiometabolic Health Scientific Sessions 2024. AHA; 2024;Abstract P192.
Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162:777–84.
Trepanowski JF, Kroeger CM, Barnosky A, Klempel MC, Bhutani S, Hoddy KK, et al. Effect of alternate-day fasting on weight loss, weight maintenance, and cardioprotection among metabolically healthy obese adults: A randomized clinical trial. JAMA Intern Med. 2017;177:930–8.
Cui Y, Cai T, Zhou Z, Mu Y, Lu Y, Gao Z, et al. Health effects of alternate-day fasting in adults: a systematic review and meta-analysis. Front Nutr. 2020;7:586036.
Whiting P, Savović J, Higgins JPT, Caldwell DM, Reeves BC, Shea B, et al. ROBIS: a new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol. 2016;69:225–34.
Higgins JPT, Li T, Deeks JJ. Chapter 6: Choosing effect measures and computing estimates of effect. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA editors. Cochrane Handbook for Systematic Reviews of Interventions version 6. Cochrane, 2023.
Follmann D, Elliott P, Suh I, Cutler J. Variance imputation for overviews of clinical trials with continuous response. J Clin Epidemiol. 1992;45:769–73.
Brozek JL, Akl EA, Alonso-Coello P, Lang D, Jaeschke R, Williams JW et al. Grading quality of evidence and strength of recommendations in clinical practice guidelines. Part 1 of 3. An overview of the GRADE approach and grading quality of evidence about interventions. Allergy. 2009;64:669–77.
Liu JY, Ni DM. Analysis of the intervention of “5∶2 intermittent fasting” dietary pattern in obese individuals. Chin J Diab Mellit. 2023;15:852–6.
Sun JC. The effect of intermittent energy restriction in young and middle-aged overweight/obese patients with hypertension. Zhejiang University of Traditional Chinese Medicine. 2022.
Chen HJ, Gao J. The effect of nutritional therapy based on fasting diet pattern in overweight and obese populations. China Mod Dr. 2020;58:127–9.
Bhutani S, Klempel MC, Kroeger CM, Trepanowski JF, Varady KA. Alternate day fasting and endurance exercise combine to reduce body weight and favorably alter plasma lipids in obese humans. Obesity 2013;21:1370–9.
Hirsh SP, Pons M, Joyal SV, Swick AG. Avoiding holiday seasonal weight gain with nutrient-supported intermittent energy restriction: a pilot study. J Nutr Sci. 2019;8:e11.
Gabel K, Hoddy KK, Haggerty N, Song J, Kroeger CM, Trepanowski JF, et al. Effects of 8-hour time restricted feeding on body weight and metabolic disease risk factors in obese adults: A pilot study. Nutr Healthy Aging. 2018;4:345–53.
Oh M, Kim S, An KY, Min J, Yang HI, Lee J, et al. Effects of alternate day calorie restriction and exercise on cardio-metabolic risk factors in overweight and obese adults: an exploratory randomized controlled study. BMC Public Health. 2018;18:1124.
Cienfuegos S, Gabel K, Kalam F, Ezpeleta M, Wiseman E, Pavlou V, et al. Effects of four-hour and six-hour time-restricted feeding on weight and cardiometabolic health: a randomized controlled trial in adults with obesity. Cell Metab. 2020;32:366–378.e3.
Lowe DA, Wu N, Rohdin-Bibby L, Moore AH, Kelly N, Liu YE, et al. Effects of time-restricted eating on weight loss and other metabolic parameters in women and men with overweight and obesity: the TREAT randomized clinical trial. JAMA Intern Med. 2020;180:1491–9.
Zhang LM, Liu Z, Wang JQ, Li RQ, Ren JY, Gao X, et al. Randomized controlled trial for time-restricted eating in overweight and obese young adults. iScience. 2022;25:104870.
Kotarsky CJ, Johnson NR, Mahoney SJ, Mitchell SL, Schimek RL, Stastny SN, et al. Time-restricted eating and concurrent exercise training reduces fat mass and increases lean mass in overweight and obese adults. Physiol Rep. 2021;9:e14868.
Haganes KL, Silva CP, Eyjólfsdóttir SK, Steen S, Grindberg M, Lydersen S, et al. Time-restricted eating and exercise training improve HbA1c and body composition in women with overweight/obesity: a randomized controlled trial. Cell Metab. 2022;34:1457–1471.e4.
Chow LS, Manoogian ENC, Alvear A, Fleischer JG, Thor H, Dietsche K, et al. Time-restricted eating effects on body composition and metabolic measures in humans who are overweight: a feasibility study. Obesity 2020;28:860–9.
Lin S, Cienfuegos S, Ezpeleta M, Gabel K, Pavlou V, Mulas A, et al. Time-restricted eating without calorie counting for weight loss in a racially diverse population: a randomized controlled trial. Ann Intern Med. 2023;176:885–95.
Phillips NE, Mareschal J, Schwab N, Manoogian E, Borloz S, Ostinelli G, et al. The effects of time-restricted eating versus standard dietary advice on weight, metabolic health and the consumption of processed food: a pragmatic randomised controlled trial in community-based adults. Nutrients 2021;13:1042.
Papageorgiou M, Biver E, Mareschal J, Phillips NE, Hemmer A, Biolley E, et al. The effects of time-restricted eating and weight loss on bone metabolism and health: a 6-month randomized controlled trial. OBESITY 2023;31:85–95.
Chen SY. Effects of Time-restricted Feeding and walking Exercise on Body Composition, Bone Mineral Density and Blood Lipids of Hidden Obesity female college Students. Henan University of Traditional Chinese Medicine. 2024.
Teng NIMF, Shahar S, Rajab NF, Manaf ZA, Johari MH, Ngah WZW. Improvement of metabolic parameters in healthy older adult men following a fasting calorie restriction intervention. Aging Male. 2013;16:177–83.
Kord-Varkaneh H, Nazary-Vannani A, Mokhtari Z, Salehi-sahlabadi A, Rahmani J, Clark CCT, et al. The influence of fasting and energy restricting diets on blood pressure in humans: a systematic review and meta-analysis. High Blood Press Cardiovasc Prev. 2020;27:271–80.
Jamshed H, Steger FL, Bryan DR, Richman JS, Warriner AH, Hanick CJ, et al. Effectiveness of early time-restricted eating for weight loss, fat loss, and cardiometabolic health in adults with obesity: a randomized clinical trial. JAMA Intern Med. 2022;182:953–62.
Conley M, Le Fevre L, Haywood C, Proietto J. Is two days of intermittent energy restriction per week a feasible weight loss approach in obese males? A randomised pilot study. Nutr Diet. 2018;75:65–72.
Sun ML, Yao W, Wang XY, Gao S, Varady KA, Forslund SK, et al. Intermittent fasting and health outcomes: an umbrella review of systematic reviews and meta-analyses of randomised controlled trials. eClinicalMedicine. 2024;70:102519.
Wilson PW, D’Agostino RB, Sullivan L, Parise H, Kannel WB. Overweight and obesity as determinants of cardiovascular risk: the Framingham experience. Arch Intern Med. 2002;162:1867–72.
Yoo JK, Fu Q. Impact of sex and age on metabolism, sympathetic activity, and hypertension. FASEB J 2020;34:11337–46.
Mattson MP, Moehl K, Ghena N, Schmaedick M, Cheng A. Intermittent metabolic switching, neuroplasticity and brain health. Nat Rev Neurosci. 2018;19:63–80.
Yao K, Su H, Cui K, Gao Y, Xu D, Wang Q, et al. Effectiveness of an intermittent fasting diet versus regular diet on fat loss in overweight and obese middle-aged and elderly people without metabolic disease: a systematic review and meta-analysis of randomized controlled trials. J Nutr Health Aging. 2024;28:100165.
Anton S, Ezzati A, Witt D, McLaren C, Vial P. The effects of intermittent fasting regimens in middle-age and older adults: Current state of evidence. Exp Gerontol. 2021;156:111617.
Liang X, Chen J, An X, Ren Y, Liu Q, Huang L, et al. The optimal time restricted eating interventions for blood pressure, weight, fat mass, glucose, and lipids: A meta-analyses and systematic review. Trends Cardiovasc Med. 2023;34:389–401.
Svendsen M, Forslund HB. Meal patterns, including intermittent fasting – a scoping review for Nordic Nutrition Recommendations 2023. Food Nutr Res. 2024;68:1–23.
Roman YM, Dominguez MC, Easow TM, Pasupuleti V, White CM, Hernandez AV. Effects of intermittent versus continuous dieting on weight and body composition in obese and overweight people: a systematic review and meta-analysis of randomized controlled trials. Int J Obes. 2019;43:2017–27.
Ezpeleta M, Cienfuegos S, Lin S, Pavlou V, Gabel K, Tussing-Humphreys L, et al. Time-restricted eating: watching the clock to treat obesity. Cell Metab. 2024;36:301–14.
Varady KA, Lin S, Oddo VM, Cienfuegos S. Debunking the myths of intermittent fasting. Nat Rev Endocrinol. 2024;20:503–4.
Conde-Pipó J, Mora-Fernandez A, Martinez-Bebia M, Gimenez-Blasi N, Lopez-Moro A, Latorre JA, et al. Intermittent fasting: does it affect sports performance? a systematic review. Nutrients 2024;16:168.
Xie Y, Yu C, Zhou W, Zhu L, Wang T, Bao H, et al. Relationship between normal weight central obesity and arterial stiffness in Chinese adults with hypertension. Nutr, Metab Cardiovasc Dis. 2024;34:343–52.
Schwingshackl L, Zähringer J, Nitschke K, Torbahn G, Lohner S, Kühn T, et al. Impact of intermittent energy restriction on anthropometric outcomes and intermediate disease markers in patients with overweight and obesity: systematic review and meta-analyses. Crit Rev Food Sci Nutr. 2021;61:1293–304.
Tutor AW, Lavie CJ, Kachur S, Milani RV, Ventura HO. Updates on obesity and the obesity paradox in cardiovascular diseases. Prog Cardiovasc Dis. 2023;78:2–10.
Ren H, Guo Y, Wang D, Kang X, Yuan G. Association of normal-weight central obesity with hypertension: a cross-sectional study from the China health and nutrition survey. BMC Cardiovasc Disord. 2023;23:120.
Gupta RD, Parray AA, Kothadia RJ, Pulock OS, Pinky SD, Haider SS, et al. The association between body mass index and abdominal obesity with hypertension among South Asian population: findings from nationally representative surveys. Clin Hypertens. 2024;30:3.
Mohseni P, Khalili D, Djalalinia S, Mohseni H, Farzadfar F, Shafiee A, et al. The synergistic effect of obesity and dyslipidemia on hypertension: results from the STEPS survey. Diabetol Metab Syndr. 2024;16:81.
de Koning L, Merchant AT, Pogue J, Anand SS. Waist circumference and waist-to-hip ratio as predictors of cardiovascular events: meta-regression analysis of prospective studies. Eur Heart J. 2007;28:850–6.
Yang F, Liu C, Liu X, Pan X, Li X, Tian L, et al. Effect of epidemic intermittent fasting on cardiometabolic risk factors: a systematic review and meta-analysis of randomized controlled trials. Front Nutr. 2021;8:669325.
Zhang Q, Zhang C, Wang H, Ma Z, Liu D, Guan X, et al. Intermittent fasting versus continuous calorie restriction: which is better for weight loss? Nutrients 2022;14:1781.
Varady KA, Cienfuegos S, Ezpeleta M, Gabel K. Cardiometabolic benefits of intermittent fasting. Annu Rev Nutr. 2021;41:333–61.
Jayawardena R, Sooriyaarachchi P, Misra A. Abdominal obesity and metabolic syndrome in South Asians: prevention and management. Expert Rev Endocrinol Metab. 2021;16:339–49.
Zhong F, Zhu T, Jin X, Chen X, Wu R, Li S, et al. Adverse events profile associated with intermittent fasting in adults with overweight or obesity: a systematic review and meta-analysis of randomized controlled trials. Nutr J. 2024;23:72.
Li DX. Brief discussion on Bigu method in Taoist medicine. China J Tradit Chin Med Pharm. 2012;27:1230–2.
Voroshilov AP, Volinsky AA, Wang Z, Marchenko EV. Modified qigong breathing exercise for reducing the sense of hunger on an empty stomach. J Evid Based Complementary Alter Med. 2017;22:687–95.
Guo JH, Liao JX, Luo RQ, Yan XW, Li BY. Effect of traditional Chinese medicine “Fuqi Bigu” technique (TCM-guided fasting with Qi-regulation) on blood pressure. China J Tradit Chin Med Pharm. 2020;35:4732–4.
Venturini C, Mancinelli L, Matacchione G, Olivieri F, Antonicelli R. The cardioprotective effects of nutritional ketosis: mechanisms and clinical implications. Nutrients 2024;16:4204.
Puchalska P, Crawford PA. Multi-dimensional roles of ketone bodies in fuel metabolism, signaling, and therapeutics. Cell Metab. 2017;25:262–84.
Acknowledgements
This research was supported by the Haidian District Health Development Research and Cultivation Program (No: HP2024-52-504002) and Xiyuan Hospital CACMS Enhancement Fund (NO. XYZX0101-14). The funders had no role in study design, data collection, data analysis, data interpretation, or writing of the manuscript.
Author information
Authors and Affiliations
Contributions
YXG, study design, data interpretation, and writing – original draft. LJL, literature search, screening, extraction, and quality assessment. LYC, literature search, screening, extraction, and quality assessment. YJW, literature search, screening, literature extraction, and quality assessment. FFZ, study design, methodology, and writing – review & editing; YRJ, study design, funding acquisition, supervision, and writing – review & editing. All authors contributed to the article and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Guo, Y., Lu, L., Chen, L. et al. Effectiveness and safety of intermittent fasting on blood pressure in adults with overweight or obesity: a systematic review. Int J Obes 49, 1240–1251 (2025). https://doi.org/10.1038/s41366-025-01823-4
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41366-025-01823-4