Abstract
Background
Various methods have been used to assess adiposity and its associations with morbidity and mortality. In this study, we aimed to examine the association of four adiposity markers with all‑cause and cause‑specific mortality, while evaluating the potential influence of reverse causation bias.
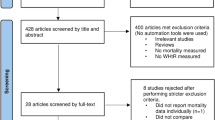
Methods
This prospective cohort study included 158,699 participants from the Mexico City Prospective Study. Cox regression models were performed to estimate the associations of body mass index, waist circumference, waist-to-height ratio, and waist-to-hip ratio with mortality risk. To minimize the influence of reverse causation, we excluded participants with prevalent diseases at baseline and conducted additional analyses excluding deaths occurring within the first 2, 5, and 10 years of follow-up.
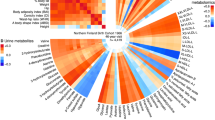
Results
Over a median of 15.5 years, 28,296 death were recorded. Waist circumference values above the recommended cutoff considered high were associated with higher all-cause mortality after the exclusion of the first 2, 5, and 10 years of follow-up (HR: 1.83; 95% CI: 1.26–2.55, HR: 1.83; 95% CI: 1.23–2.62, and HR: 1.85; 95% CI: 1.14–2.70, respectively). Elevated waist-to-hip ratio was associated with increased all-cause mortality across the same exclusion periods (HR: 1.71; 95% CI: 1.07–2.30, HR: 1.70; 95% CI: 1.05–2.49, and HR: 1.71; 95% CI: 1.01-2.52). High waist circumference was strongly associated with CVD mortality after exclusion of the first 2, 5, and 10 years (HR: 4.76; 95% CI: 1.70–11.82, HR: 4.75; 95% CI: 1.56–11.88, and HR: 4.73; 95% CI: 1.42–12.90, respectively). Elevated waist-to-hip ratio similarly showed associations with CVD mortality (HR: 2.69; 95% CI: 1.10–5.60, HR: 2.66; 95% CI: 1.12–5.75, and HR: 2.64; 95% CI: 1.03–7.32). Body mass index, waist circumference, waist-to-height ratio, and waist-hip ratio were not associated with respiratory and cancer mortality.
Conclusions
Waist circumference was the adiposity marker most strongly associated with all-cause and CVD mortality, even after excluding the first 10 years of follow-up.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
Data from the Mexico City Prospective Study are available to bona fide researchers for collaborative and/or open-access research purposes. The study’s Data and Sample Sharing policy can be downloaded (in English or Spanish: https://www.ctsu.ox.ac.uk/research/mcps). Available study data can be examined in the study Data Showcase (https://datashare.ndph.ox.ac.uk/mexico).
References
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in underweight and obesity from 1990 to 2022: a pooled analysis of 3663 population-representative studies with 222 million children, adolescents, and adults. Lancet. 2024;403:1027–50.
Barquera S, Hernández-Barrera L, Trejo-Valdivia B, Shamah T, Campos-Nonato I, Rivera-Dommarco J. Obesity in Mexico, prevalence andtrends in adults. Ensanut 2018-19. Salud Publ Mex. 2020;62:682–92.
Abdelaal M, le Roux CW, Docherty NG. Morbidity and mortality associated with obesity. Ann Transl Med. 2017;5:161.
Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, Halsey J, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373:1083–96.
Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309:71–82.
Global BMI Mortality Collaboration, Di Angelantonio E, Bhupathiraju Sh N, Wormser D, Gao P, Kaptoge S, et al. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet. 2016;388:776–86.
Xu H, Cupples LA, Stokes A, Liu CT. Association of obesity with mortality over 24 years of weight history: findings from the Framingham Heart Study. JAMA Netw Open. 2018;1:e184587.
Han TS, Sattar N, Lean M. Assessment of obesity and its clinical implications. BMJ. 2006;333:695–8.
Piqueras P, Ballester A, Durá-Gil JV, Martinez-Hervas S, Redón J, Real JT. Anthropometric indicators as a tool for diagnosis of obesity and other health risk factors: a literature review. Front Psychol. 2021;12:631179.
Goh LG, Dhaliwal SS, Welborn TA, Lee AH, Della PR. Anthropometric measurements of general and central obesity and the prediction of cardiovascular disease risk in women: a cross-sectional study. BMJ Open. 2014;4:e004138.
Lawlor DA, Hart CL, Hole DJ, Davey Smith G. Reverse causality and confounding and the associations of overweight and obesity with mortality. Obesity. 2006;14:2294–304.
Rezende LFM, Ferrari G, Lee DH, Aune D, Liao B, Huang W, et al. Lifestyle risk factors and all-cause and cause-specific mortality: assessing the influence of reverse causation in a prospective cohort of 457,021 US adults. Eur J Epidemiol. 2022;37:1123.
Lee DH, Giovannucci EL. Body composition and mortality in the general population: a review of epidemiologic studies. Exp Biol Med. 2018;243:1275–85.
Aune D, Sen A, Prasad M, Norat T, Janszky I, Tonstad S, et al. BMI and all cause mortality: systematic review and non-linear dose-response meta-analysis of 230 cohort studies with 3.74 million deaths among 30.3 million participants. BMJ. 2016;353:i2156.
Kumar A, Karmarkar AM, Tan A, Graham JE, Arcari CM, Ottenbacher KJ, et al. The effect of obesity on incidence of disability and mortality in Mexicans aged 50 years and older. Salud Publica Mex. 2015;57:S31–8.
Jadhav R, Markides KS, Al Snih S. Body mass index and 12-year mortality among older Mexican Americans aged 75 years and older. BMC Geriatrics. 2022;22:236.
NCD Risk Factor Collaboration (NCD-RisC). Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. Lancet. 2016;387:1377–96.
Gnatiuc L, Tapia-Conyer R, Wade R, Ramirez-Reyes R, Aguilar-Ramirez D, Herrington W, et al. Abdominal and gluteo-femoral markers of adiposity and risk of vascular-metabolic mortality in a prospective study of 150 000 Mexican adults. Eur J Prev Cardiol. 2022;29:730–8.
Gnatiuc L, Alegre-Díaz J, Wade R, Ramirez-Reyes R, Tapia-Conyer R, Garcilazo-Ávila A, et al. General and abdominal adiposity and mortality in mexico city: a prospective study of 150 000 adults. Ann Intern Med. 2019;171:397–405.
Tapia-Conyer R, Kuri-Morales P, Alegre-Díaz J, Whitlock G, Emberson J, Clark S, et al. Cohort profile: the Mexico City Prospective Study. Int J Epidemiol. 2006;35:243–9.
Keys A, Fidanza F, Karvonen MJ, Kimura N, Taylor HL. Indices of relative weight and obesity. J Chronic Dis. 1972;25:329–43.
Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:1–253. i-xii.
Alberti KG, Zimmet P, Shaw J. Metabolic syndrome-a new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabet Med. 2006;23:469–80.
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42:3599–726.
Hsieh SD, Yoshinaga H. Abdominal fat distribution and coronary heart disease risk factors in men-waist/height ratio as a simple and useful predictor. Int J Obes Relat Metab Disord. 1995;19:585–9.
Nishida C, Ko GT, Kumanyika S. Body fat distribution and noncommunicable diseases in populations: overview of the 2008 WHO Expert Consultation on Waist Circumference and Waist-Hip Ratio. Eur J Clin Nutr. 2010;64:2–5.
Mikkelsen L, Phillips DE, AbouZahr C, Setel PW, de Savigny D, Lozano R, et al. A global assessment of civil registration and vital statistics systems: monitoring data quality and progress. Lancet. 2015;386:1395–406.
Visaria A, Setoguchi S. Body mass index and all-cause mortality in a 21st century U.S. population: A National Health Interview Survey analysis. PLoS One. 2023;18:e0287218.
Winter JE, MacInnis RJ, Wattanapenpaiboon N, Nowson CA. BMI and all-cause mortality in older adults: a meta-analysis. Am J Clin Nutr. 2014;99:875–90.
Grabowski DC, Ellis JE. High body mass index does not predict mortality in older people: analysis of the Longitudinal Study of Aging. J Am Geriatr Soc. 2001;49:968–79.
Carr PR, Webb KL, Neumann JT, Thao LTP, Beilin LJ, Ernst ME, et al. Associations of body size with all-cause and cause-specific mortality in healthy older adults. Sci Rep. 2023;13:3799.
Nowak MM, Niemczyk M, Gołębiewski S, Pączek L. Impact of body mass index on all-cause mortality in adults: a systematic review and meta-analysis. J Clin Med. 2024;13:2305.
Cerhan JR, Moore SC, Jacobs EJ, Kitahara CM, Rosenberg PS, Adami HO, et al. A pooled analysis of waist circumference and mortality in 650,000 adults. Mayo Clin Proc. 2014;89:335–45.
Kim YH, Kim SM, Han KD, Jung JH, Lee SS, Oh SW, et al. Waist Circumference and all-cause mortality independent of body mass index in korean population from the National Health Insurance Health Checkup 2009-2015. J Clin Med. 2019;8:72.
Ross R, Neeland IJ, Yamashita S, Shai I, Seidell J, Magni P, et al. Waist circumference as a vital sign in clinical practice: a Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nat Rev Endocrinol. 2020;16:177–89.
Song DK, Hong YS, Sung YA, Lee H. Waist circumference and mortality or cardiovascular events in a general Korean population. PLoS One. 2022;17:e0267597.
Chen Q, Li L, Yi J, Huang K, Shen R, Wu R, et al. Waist circumference increases risk of coronary heart disease: evidence from a Mendelian randomization study. Mol Genet Genomic Med. 2020;8:e1186.
Ashwell M, Gunn P, Gibson S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Obes Rev. 2012;13:275–86.
Ashwell M, Gibson S. A proposal for a primary screening tool: ‘Keep your waist circumference to less than half your height. BMC Med. 2014;12::207.
Neeland IJ, Ross R, Després JP, Matsuzawa Y, Yamashita S, Shai I, et al. Visceral and ectopic fat, atherosclerosis, and cardiometabolic disease: a position statement. Lancet Diabetes Endocrinol. 2019;7:715–25.
Chait A, den Hartigh LJ. Adipose tissue distribution, inflammation and its metabolic consequences, including diabetes and cardiovascular disease. Front Cardiovasc Med. 2020;7:22.
Abdi Dezfouli R, Mohammadian Khonsari N, Hosseinpour A, Asadi S, Ejtahed H-S, Qorbani M. Waist to height ratio as a simple tool for predicting mortality: a systematic review and meta-analysis. Int J Obes. 2023;47:1286–301.
Jayedi A, Soltani S, Zargar MS, Khan TA, Shab-Bidar S. Central fatness and risk of all cause mortality: systematic review and dose-response meta-analysis of 72 prospective cohort studies. BMJ. 2020;370:m3324.
Harris E. Study: Waist-to-hip ratio might predict mortality better than BMI. JAMA. 2023;330:1515–6.
Myint PK, Kwok CS, Luben RN, Wareham NJ, Khaw K-T. Body fat percentage, body mass index and waist-to-hip ratio as predictors of mortality and cardiovascular disease. Heart. 2014;100:1613–9.
Acknowledgements
This research has been conducted using Mexico City Prospective Study (MCPS) Data under Application Number 2022-020. MCPS (https://www.ctsu.ox.ac.uk/research/mcps) has received funding from the Mexican Health Ministry, the National Council of Science and Technology for Mexico, Wellcome, and core grants from the UK Medical Research Council to the MRC Population Health Research Unit at the University of Oxford. We would like to thank the participants from the Mexico City Prospective Study. We thank everyone who took part in the Mexico City Prospective Study.
Funding
The present research received financial support from Vicerrectoría de Investigación y Doctorados, Universidad Autónoma de Chile. National Council for Scientific and Technological Development - CNPq (311109-2023-3; LFMR). This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES) - Finance Code 001 (WAdS). GF was funded by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES) – Code: 88887.979411/2024-00.
Author information
Authors and Affiliations
Contributions
WAdS, and GF, contributed to the conception and design of the study. WAdS, and GF advised on all statistical aspects. LFMR, AM, MdMN, EN, DC, and RFdC performed the literature search, the analyses and interpreted the data. All authors critically reviewed this and previous drafts. All authors approved the final draft for submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
da Silva, W.A., Rezende, L.F.M., Marques, A. et al. Which adiposity marker is most strongly associated with all‑cause and cause‑specific mortality? a prospective study of 158,699 Mexican adults. Int J Obes 49, 1792–1799 (2025). https://doi.org/10.1038/s41366-025-01827-0
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41366-025-01827-0