Abstract
Background
The impact of dynapenic obesity on the progression of cardiometabolic multimorbidity (CMM) remains poorly understood. This study aimed to explore the association between dynapenic obesity and cardiometabolic diseases (CMD) progression, as well as the mediating roles of C-reactive protein (CRP) and the atherogenic index of plasma (AIP).
Methods
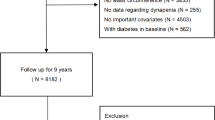
The study included 446,862 UK Biobank participants. CMM was defined as the coexistence of two or three CMDs, including type 2 diabetes (T2DM), coronary heart disease (CHD) and stroke. Dynapenic obesity was classified into dynapenic general obesity and dynapenic abdominal obesity, assessed by handgrip strength (HGS), body mass index (BMI), and waist circumference (WC). A multi-state model was employed to evaluate the influence of dynapenic obesity on CMD progression. Counterfactual mediation analyses were conducted to investigate the mediating role of CRP and AIP.
Results
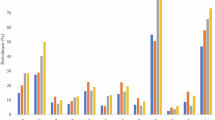
Over a median 13.67-years follow-up, 54,555 participants developed CMD, 5842 developed CMM, and 32,930 died. Compared with non-dynapenia and non-general obesity (ND/NGO), the HRs (95% CI) of first CMD (FCMD), CMM, and death for dynapenia and general obesity (D/GO) were 2.75 (2.61,2.90), 4.61 (4.05,5.24), and 1.68 (1.56,1.80), respectively. Similar results were observed for dynapenic abdominal obesity. Compared with ND/NGO, the proportions of CRP and AIP mediated associations of D/GO with FCMD risk were 19.58% (95% CI: 18.66%, 20.18%) and 18.99% (95% CI: 18.12%, 19.62%), respectively, which were lower than the proportions mediated in the associations of dynapenia and abdominal obesity (D/AO) with FCMD (CRP: 30.38% vs. 19.58%; AIP: 31.40% vs. 18.99%). Furthermore, CRP and AIP accounted for a greater proportion of the association between dynapenic obesity and CMM than FCMD.
Conclusion
This study indicated that there are differential effects associated with dynapenic obesity during the longitudinal progression of CMD. CRP and AIP may play a partial role in mediating this association.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The data that support this study are available from the UK Biobank, which were used under license for the current study, and so are not publicly available. More details can be found at https://www.ukbiobank.ac.uk/.
References
Han Y, Hu Y, Yu C, Guo Y, Pei P, Yang L, et al. Lifestyle, cardiometabolic disease, and multimorbidity in a prospective Chinese study. Eur Heart J. 2021;42:3374–84.
Singh-Manoux A, Fayosse A, Sabia S, Tabak A, Shipley M, Dugravot A, et al. Clinical, socioeconomic, and behavioural factors at age 50 years and risk of cardiometabolic multimorbidity and mortality: a cohort study. PLoS Med. 2018;15:e1002571.
Collaboration TERF. Association of cardiometabolic multimorbidity with mortality. JAMA. 2015;314:52–60.
Tessier AJ, Wing SS, Rahme E, Morais JA, Chevalier S. Physical function-derived cut-points for the diagnosis of sarcopenia and dynapenia from the Canadian longitudinal study on aging. J Cachexia Sarcopenia Muscle. 2019;10:985–99.
Alexandre Tda S, Duarte YA, Santos JL, Wong R, Lebrão ML. Sarcopenia according to the European Working Group on Sarcopenia in Older People (EWGSOP) versus dynapenia as a risk factor for mortality in the elderly. J Nutr Health Aging. 2014;18:751–6.
GBD 2021 Adult BMI Collaborators. Global, regional, and national prevalence of adult overweight and obesity, 1990-2021, with forecasts to 2050: a forecasting study for the Global Burden of Disease Study 2021. Lancet. 2025;405:813–38.
Carvalho MO, Duque AP, Huguenin GVB, Felix Mediano MF, Rodrigues Júnior LF. Increased cardiometabolic risk in dynapenic obesity: results from the Study of Workers’ Health (ESAT). Life. 2024;14:1174.
Celis-Morales CA, Welsh P, Lyall DM, Steell L, Petermann F, Anderson J, et al. Associations of grip strength with cardiovascular, respiratory, and cancer outcomes and all cause mortality: prospective cohort study of half a million UK Biobank participants. BMJ. 2018;361:k1651.
Alexandre TDS, Aubertin-Leheudre M, Carvalho LP, Máximo RO, Corona LP, Brito TRP, et al. Dynapenic obesity as an associated factor to lipid and glucose metabolism disorders and metabolic syndrome in older adults—findings from SABE Study. Clin Nutr. 2018;37:1360–6.
Carbone S, Kirkman DL, Garten RS, Rodriguez-Miguelez P, Artero EG, Lee DC, et al. Muscular strength and cardiovascular disease: an updated state-of-the-art narrative review. J Cardiopulm Rehabil Prev. 2020;40:302–9.
Setoyama Y, Honda T, Tajimi T, Sakata S, Oishi E, Furuta Y, et al. Association between dynapenic obesity and risk of cardiovascular disease: the Hisayama study. J Cachexia Sarcopenia Muscle. 2024;15:2338–48.
Gruberg L, Weissman NJ, Waksman R, Fuchs S, Deible R, Pinnow EE, et al. The impact of obesity on the short-term andlong-term outcomes after percutaneous coronary intervention: the obesity paradox?. J Am Coll Cardiol. 2002;39:578–84.
Uretsky S, Messerli FH, Bangalore S, Champion A, Cooper-DeHoff RM, Zhou Q, et al. Obesity paradox in patients with hypertension and coronary artery disease. Am J Med. 2007;120:863–70.
Ross R, Neeland IJ, Yamashita S, Shai I, Seidell J, Magni P, et al. Waist circumference as a vital sign in clinical practice: a consensus statement from the IAS and ICCR Working Group on Visceral Obesity. Nat Rev Endocrinol. 2020;16:177–89.
Máximo RO, de Oliveira DC, Ramirez PC, Luiz MM, de Souza AF, Delinocente MLB, et al. Combination of dynapenia and abdominal obesity affects long-term physical performance trajectories in older adults: sex differences. Am J Clin Nutr. 2022;115:1290–9.
Haeri NS, Perera S, Nadkarni NK, Greenspan SL. Association of inflammatory markers with muscle and cognitive function in early and late-aging older adults. J Nutr Health Aging. 2024;28:100207.
Dobiásová M, Frohlich J. The plasma parameter log (TG/HDL-C) as an atherogenic index: correlation with lipoprotein particle size and esterification rate in apoB-lipoprotein-depleted plasma (FER(HDL)). Clin Biochem. 2001;34:583–8.
Zhou Q, Wu Y, Li M. Association between the atherogenic index of plasma and long-term risk of type 2 diabetes: a 12-year cohort study based on the Japanese population. Cardiovasc Diabetol. 2025;24:50.
Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015;12:e1001779.
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48:16–31.
Koskinas KC, Van Craenenbroeck EM, Antoniades C, Blüher M, Gorter TM, Hanssen H, et al. Obesity and cardiovascular disease: an ESC clinical consensus statement. Eur Heart J. 2024;45:4063–98.
Visseren FLJ, Mach F, Smulders YM, Carballo D, Koskinas KC, Bäck M, et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2021;42:3227–337.
Fernández-Macías JC, Ochoa-Martínez AC, Varela-Silva JA, Pérez-Maldonado IN. Atherogenic index of plasma: novel predictive biomarker for cardiovascular illnesses. Arch Med Res. 2019;50:285–94.
Wang N, Jia X, Fan Z, Yang C, Wang Y, Fan J, et al. Educational inequalities in cardiovascular diseases and their mediating factors across different generations: a prospective cohort study. Eur Heart J Qual Care Clin Outcomes. 2025;qcaf010.
Shi B, Choirat C, Coull BA, VanderWeele TJ, Valeri L. CMAverse: a suite of functions for reproducible causal mediation analyses. Epidemiology. 2021;32:e20–22.
Skou ST, Mair FS, Fortin M, Guthrie B, Nunes BP, Miranda JJ, et al. Multimorbidity. Nat Rev Dis Prim. 2022;8:48.
Langenberg C, Hingorani AD, Whitty CJM. Biological and functional multimorbidity—from mechanisms to management. Nat Med. 2023;29:1649–57.
Yu B, Jia S, Sun T, Liu J, Jin J, Zhang S, et al. Sarcopenic obesity is associated with cardiometabolic multimorbidity in Chinese middle-aged and older adults: a cross-sectional and longitudinal study. J Nutr Health Aging. 2024;28:100353.
Farmer RE, Mathur R, Schmidt AF, Bhaskaran K, Fatemifar G, Eastwood SV, et al. Associations between measures of sarcopenic obesity and risk of cardiovascular disease and mortality: a cohort study and Mendelian randomization analysis using the UK Biobank. J Am Heart Assoc. 2019;8:e011638.
Putter H, Fiocco M, Geskus RB. Tutorial in biostatistics: competing risks and multi-state models. Stat Med. 2007;26:2389–430.
de Wreede LC, Fiocco M, Putter H. The mstate package for estimation and prediction in non- and semi-parametric multi-state and competing risks models. Comput Methods Prog Biomed. 2010;99:261–74.
Veronese N, Koyanagi A, Soysal P, Sapienza V, Ragusa FS, Bolzetta F, et al. Dynapenic abdominal obesity and incident multimorbidity: findings from the English longitudinal study on ageing. Aging Clin Exp Res. 2023;35:1671–8.
Kahn SE, Hull RL, Utzschneider KM. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature. 2006;444:840–6.
Stenholm S, Mehta NK, Elo IT, Heliövaara M, Koskinen S, Aromaa A. Obesity and muscle strength as long-term determinants of all-cause mortality-a 33-year follow-up of the Mini-Finland Health Examination Survey. Int J Obes. 2014;38:1126–32.
Chen Y, Koirala B, Ji M, Commodore-Mensah Y, Dennison Himmelfarb CR, Perrin N, et al. Obesity paradox of cardiovascular mortality in older adults in the United States: a cohort study using 1997-2018 National Health Interview Survey data linked with the National Death Index. Int J Nurs Stud. 2024;155:104766.
Dorner TE, Rieder A. Obesity paradox in elderly patients with cardiovascular diseases. Int J Cardiol. 2012;155:56–65.
Itoh H, Kaneko H, Okada A, Suzuki Y, Fujiu K, Matsuoka S, et al. Age-specific relation of cardiovascular health metrics with incident cardiovascular disease. Am J Cardiol. 2022;177:34–39.
Ramírez PC, de Oliveira Máximo R, Capra de Oliveira D, de Souza AF, Marques Luiz M, Bicigo Delinocente ML, et al. Dynapenic abdominal obesity as a risk factor for metabolic syndrome in individual 50 years of age or older: English Longitudinal Study of Ageing. J Nutr Health Aging. 2023;27:1188–95.
Acknowledgements
We thank the faculties from the UK Biobank Access Management Team for helping us in the data preparation (Application Number 170605).
Funding
This work was supported by the National Natural Science Foundation of China (Nos. 82304251 and 82371597).
Author information
Authors and Affiliations
Contributions
NNW, TRW, and XCJ contributed to the design of study, conducted study, and drafted the initial manuscript. YPW, JWF, YLN, and CYZ revised the manuscript. CJY and ZXF assisted in analyzing the data. XZS and YLY were involved in study supervision. All authors read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
All participants in UK biobank received written informed consent and ethical approval from the North West Multi-Centre Research Ethics Committee. The resource application number for this study is 170605. The study was conducted in accordance with the Declaration of Helsinki, and all methods were performed in accordance with the UK Biobank Ethics and Governance Framework.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, N., Wang, T., Jia, X. et al. Dynapenic obesity associated with incidence and progression trajectory of cardiometabolic diseases: a prospective cohort study. Int J Obes 49, 1820–1828 (2025). https://doi.org/10.1038/s41366-025-01831-4
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41366-025-01831-4