Abstract
Objectives
To identify the association between body size and atherogenic risk index (Total Cholesterol/High Density Lipoprotein (TC/HDL) ratio) associated with ischemic heart disease (IHD).
Methods
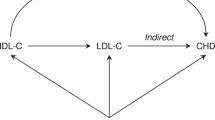
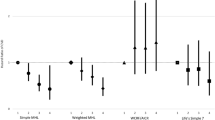
Allometric models were used to reveal the association between body size and social behaviours associated with TC:HDL based on the effect sizes obtained from the log-transformed allometric models. Mediation analysis was used to explain why moderate (MPA) or vigorous physical activity (VPA) were strongly associated with body size dimensions or directly associated with TC/HDL.
Results
An allometric model for the atherogenic risk index (TC/HDL) ratio identified waist circumference (WC) and smoking as having the strongest association (strongest effect sizes) with cholesterol-related indices and hence IHD. A strong negative exponent or effect associated with height was also identified, suggesting that taller individuals will inherently have lower cholesterol-related indices. The mediation analysis identified that MPA and VPA were both strongly associated with reducing WC but only VPA was directly associated with the TC/HDL.
Conclusions
These results confirm that taller, non-smokers who have smaller WC are more likely to have a lower atherogenic risk index (TC/HDL) ratio and hence be at reduced risk of IHD. Participation in regular moderate activity to reduce their WC is not necessarily or directly associated with lower atherogenic risk index (TC/HDL) and hence a lower risk of IHD. Being taller with smaller WC, possibly but not necessarily due to taking MVPA, was associated with a lower atherogenic risk index (TC/HDL-C) ratio and hence have lower risk of IHD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Data are available upon reasonable request from the authors of the manuscript.
References
Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139:e1082–e143.
Reiner Z, Catapano AL, De Backer G, Graham I, Taskinen MR, Wiklund O, et al. ESC/EAS Guidelines for the management of dyslipidaemias: the Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Eur Heart J. 2011;32:1769–818.
Assmann G, Davignon J, Fernandez-Cruz A, Gotto AM Jr, Jacotot B, Lewis B, et al. HDL cholesterol profile in 1988. Rev Clin Esp. 1989;184:421–30.
Tall AR. HDL in morbidity and mortality: a 40+ year perspective. Clin Chem. 2021;67:19–23.
Toth PP, Barter PJ, Rosenson RS, Boden WE, Chapman MJ, Cuchel M, et al. High-density lipoproteins: a consensus statement from the National Lipid Association. J Clin Lipidol. 2013;7:484–525.
Palmer GroverSA, Coupal CS. L. Serum lipid screening to identify high-risk individuals for coronary death. The results of the Lipid Research Clinics prevalence cohort. Arch Intern Med. 1994;154:679–84.
Garrison CastelliWP, Wilson RJ, Abbott PW, Kalousdian RD, Kannel S. WB. Incidence of coronary heart disease and lipoprotein cholesterol levels. The Framingham Study. JAMA. 1986;256:2835–8.
Lemieux I, Lamarche B, Couillard C, Pascot A, Cantin B, Bergeron J, et al. Total cholesterol/HDL cholesterol ratio vs LDL cholesterol/HDL cholesterol ratio as indices of ischemic heart disease risk in men: the Quebec Cardiovascular Study. Arch Intern Med. 2001;161:2685–92.
Lamarche B, Moorjani S, Lupien PJ, Cantin B, Bernard PM, Dagenais GR, et al. Apolipoprotein A-I and B levels and the risk of ischemic heart disease during a five-year follow-up of men in the Quebec cardiovascular study. Circulation. 1996;94:273–8.
Jeppesen J, Hein HO, Suadicani P, Gyntelberg F. Relation of high TG-low HDL cholesterol and LDL cholesterol to the incidence of ischemic heart disease. An 8-year follow-up in the Copenhagen Male Study. Arterioscler Thromb Vasc Biol. 1997;17:1114–20.
Perini W, Snijder MB, Peters RJ, Kunst AE, van Valkengoed IG. Estimation of cardiovascular risk based on total cholesterol versus total cholesterol/high-density lipoprotein within different ethnic groups: the HELIUS study. Eur J Prev Cardiol. 2019;26:1888–96.
Zhou D, Liu X, Lo K, Huang Y, Feng Y. The effect of total cholesterol/high-density lipoprotein cholesterol ratio on mortality risk in the general population. Front Endocrinol. 2022;13:1012383.
Millan J, Pinto X, Munoz A, Zuniga M, Rubies-Prat J, Pallardo LF, et al. Lipoprotein ratios: physiological significance and clinical usefulness in cardiovascular prevention. Vasc Health Risk Manag. 2009;5:757–65.
Ledoux M, Lambert J, Reeder BA, Despres JP. Correlation between cardiovascular disease risk factors and simple anthropometric measures. Canadian Heart Health Surveys Research Group. CMAJ. 1997;157:S46–53.
Ledoux M, Lambert J, Reeder BA, Despres JP. A comparative analysis of weight to height and waist to hip circumference indices as indicators of the presence of cardiovascular disease risk factors. Canadian Heart Health Surveys Research Group. CMAJ. 1997;157:S32–8.
Friedrich M, Goluch-Koniuszy Z. The effectiveness of nutritional education among women aged 60-85 on the basis of anthropometric parameters and lipid profiles. Rocz Panstw Zakl Hig. 2017;68:253–60.
Nevill AM, Duncan MJ, Lahart IM, Sandercock GR. Scaling waist girth for differences in body size reveals a new improved index associated with cardiometabolic risk. Scand J Med Sci Sports. 2017;27:1470–6.
Elsadek Seaoud EAM, Amin MI, Abdelbasit MS. Total cholesterol/high-density lipoprotein cholesterol and low-density lipoprotein cholesterol/high-density lipoprotein cholesterol as predictors of coronary artery calcification assessed by multidetector computed tomography coronary angiography. ARYA Atheroscler. 2022;18:1–7.
Goldbourt U, Yaari S, Cohen-Mandelzweig L, Neufeld HN. High-density lipoprotein cholesterol: correlation with biochemical, anthropometric, behavioral, and clinical parameters in 6500 Israeli men. Prev Med. 1986;15:569–81.
Henriksson KM, Lindblad U, Agren B, Nilsson-Ehle P, Rastam L. Associations between body height, body composition and cholesterol levels in middle-aged men. the coronary risk factor study in southern Sweden (CRISS). Eur J Epidemiol. 2001;17:521–6.
Liu Y, Tong G, Tong W, Lu L, Qin X. Can body mass index, waist circumference, waist-hip ratio and waist-height ratio predict the presence of multiple metabolic risk factors in Chinese subjects? BMC Public Health. 2011;11:35.
Oliveira-Santos J, Santos R, Moreira C, Abreu S, Lopes L, Agostinis-Sobrinho C, et al. Associations between anthropometric indicators in early life and low-grade inflammation, insulin resistance and lipid profile in adolescence. Nutr Metab Cardiovasc Dis. 2019;29:783–92.
Sultan N, Nawaz M, Sultan A, Fayaz M. Waist hip ratio as an index for identifying women with raised TC/HDL ratios. J Ayub Med Coll Abbottabad. 2004;16:38–41.
Ashwell M, Hsieh SD. Six reasons why the waist-to-height ratio is a rapid and effective global indicator for health risks of obesity and how its use could simplify the international public health message on obesity. Int J Food Sci Nutr. 2005;56:303–7.
Orsatti FL, Nahas EA, Nahas-Neto J, Maesta N, Padoani NP, Orsatti CL. Anthropometric measures: predictors of non-transmissible chronic diseases in postmenopausal women in the Southeast region of Brazil. Rev Bras Ginecol Obstet. 2008;30:182–9.
Lee CMY, Huxley RR, Wildman RP, Woodward M. Indices of abdominal obesity are better discriminators of cardiovascular risk factors than BMI: a meta-analysis. J Clin Epidemiol. 2008;61:646–53.
Xu C, Yang X, Zu S, Han S, Zhang Z, Zhu G. Association between serum lipids, blood pressure, and simple anthropometric measures in an adult Chinese population. Arch Med Res. 2008;39:610–7.
Aldrich J. Correlations genuine and spurious in Pearson and Yule. Stat Sci. 1995;10:364–76.
Nevill AM, Bryant E, Wilkinson K, Gomes TN, Chaves R, Pereira S, et al. Can waist circumference provide a new “third” dimension to BMI when predicting percentage body fat in children? Insights using allometric modelling. Pediatr Obes. 2019;14:e12491.
Maeda K, Noguchi Y, Fukui T. The effects of cessation from cigarette smoking on the lipid and lipoprotein profiles: a meta-analysis. Prev Med. 2003;37:283–90.
Rimm EB, Williams P, Fosher K, Criqui M, Stampfer MJ. Moderate alcohol intake and lower risk of coronary heart disease: meta-analysis of effects on lipids and haemostatic factors. BMJ. 1999;319:1523–8.
Brien SE, Ronksley PE, Turner BJ, Mukamal KJ, Ghali WA. Effect of alcohol consumption on biological markers associated with risk of coronary heart disease: systematic review and meta-analysis of interventional studies. BMJ. 2011;342:d636.
Bays HE, Toth PP, Kris-Etherton PM, Abate N, Aronne LJ, Brown WV, et al. Obesity, adiposity, and dyslipidemia: a consensus statement from the National Lipid Association. J Clin Lipidol. 2013;7:304–83.
Clifton PM. Diet, exercise and weight loss and dyslipidaemia. Pathology. 2019;51:222–6.
Handelsman Y, Jellinger PS, Guerin CK, Bloomgarden ZT, Brinton EA, Budoff MJ, et al. Consensus Statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the Management of Dyslipidemia and Prevention of Cardiovascular Disease Algorithm—2020 Executive Summary. Endocr Pract. 2020;26:1196–224.
Mann S, Beedie C, Jimenez A. Differential effects of aerobic exercise, resistance training and combined exercise modalities on cholesterol and the lipid profile: review, synthesis and recommendations. Sports Med. 2014;44:211–21.
Mendoza MF, Lavie CJ. Clinical associations between exercise and lipoproteins. Curr Opin Lipidol. 2022;33:364–73.
Kelley GA, Kelley KS, Roberts S, Haskell W. Efficacy of aerobic exercise and a prudent diet for improving selected lipids and lipoproteins in adults: a meta-analysis of randomized controlled trials. BMC Med. 2011;9:74.
Wood G, Taylor E, Ng V, Murrell A, Patil A, van der Touw T, et al. Determining the effect size of aerobic exercise training on the standard lipid profile in sedentary adults with three or more metabolic syndrome factors: a systematic review and meta-analysis of randomised controlled trials. Br J Sports Med. 2021;56:1032–41.
NatCen. National Diet and Nutrition Survey Years 1-11, 2008-2019. [data collection]. In: University of Cambridge MEU, NatCen Social Research, editor. 19th Edition. ed: UK Data Service, 2023 [Accessed 10 November 2023]; 2023.
Mindell J, Stamatakis E, Brage S. Measuring energy expenditure in NDNS 2008–2012. London: UCL; 2009.
Besson H, Brage S, Jakes RW, Ekelund U, Wareham NJ. Estimating physical activity energy expenditure, sedentary time, and physical activity intensity by self-report in adults. Am J Clin Nutr. 2010;91:106–14.
Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DR Jr, Tudor-Locke C, et al. 2011 Compendium of physical activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43:1575–81.
IPSOS.MORI. Active Lives Survey: Year 1 Technical Report. 2017.
Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502.
Nevill AM, Holder RL. Scaling, normalizing, and per ratio standards: an allometric modeling approach. J Appl Physiol. 1995;79:1027–31.
Kodama S, Tanaka S, Saito K, Shu M, Sone Y, Onitake F, et al. Effect of aerobic exercise training on serum levels of high-density lipoprotein cholesterol: a meta-analysis. Arch Intern Med. 2007;167:999–1008.
O’Rourke HP, MacKinnon DP. Reasons for testing mediation in the absence of an intervention effect: a research imperative in prevention and intervention research. J Stud Alcohol Drugs. 2018;79:171–81.
Valente MJ, Pelham WE, Smyth H, MacKinnon DP. Confounding in statistical mediation analysis: what it is and how to address it. J Couns Psychol. 2017;64:659–71.
Lin Q, Nuttall AK, Zhang Q, Frank KA. How do unobserved confounding mediators and measurement error impact estimated mediation effects and corresponding statistical inferences? Introducing the R package ConMed for sensitivity analysis. Psychol Methods. 2023;28:339–58.
Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychol Methods. 2002;7:422–45.
Igartua JJ, Hayes AF. Mediation, moderation, and conditional process analysis: concepts, computations, and some common confusions. Span J Psychol. 2021;24:e49.
Nevill AM, Lang JJ, Tomkinson GR. What is the optimal anthropometric index/ratio associated with two key measures of cardio-metabolic risk associated with hypertension and diabetes?. Int J Obes. 2022;46:1304–10.
Adejumo EN, Adejumo AO, Azenabor A, Ekun AO, Enitan SS, Adebola OK, et al. Anthropometric parameter that best predict metabolic syndrome in South west Nigeria. Diabetes Metab Syndr. 2019;13:48–54.
Wang S, Wang S, Jiang S, Ye Q. An anthropometry-based nomogram for predicting metabolic syndrome in the working population. Eur J Cardiovasc Nurs. 2020;19:223–9.
Sagun G, Oguz A, Karagoz E, Filizer AT, Tamer G, Mesci B. Application of alternative anthropometric measurements to predict metabolic syndrome. Clinics. 2014;69:347–53.
Al-Shami I, Alkhalidy H, Alnaser K, Mukattash TL, Al Hourani H, Alzboun T, et al. Assessing metabolic syndrome prediction quality using seven anthropometric indices among Jordanian adults: a cross-sectional study. Sci Rep. 2022;12:21043.
Li Y, Zheng R, Li S, Cai R, Ni F, Zheng H, et al. Association between four anthropometric indexes and metabolic syndrome in US adults. Front Endocrinol. 2022;13:889785.
Nevill AM, Duncan MJ, Myers T. BMI is dead; long live waist-circumference indices: but which index should we choose to predict cardio-metabolic risk?. Nutr Metab Cardiovasc Dis. 2022;32:1642–50.
Akyuz A. Exercise and coronary heart disease, advances in experimental medicine and biology. In: Xiao J, editor. Physical exercise for human health. 1288. (Springer, 2020).
Mertens E, Clarys P, Lefevre J, Charlier R, Knaeps S, Deforche B. Longitudinal study on the association between cardiorespiratory fitness, anthropometric parameters and blood lipids. J Phys Act Health. 2016;13:467–73.
Jensen M, Ryan D, Apovian C, Ard J, Comuzzie A, Donato K, et al. Obesity Society 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation. 2014;129:S102–38.
Barone Gibbs B, Hivert MF, Jerome GJ, Kraus WE, Rosenkranz SK, Schorr EN, et al. Physical activity as a critical component of first-line treatment for elevated blood pressure or cholesterol: who, what, and how?: A scientific statement From the American Heart Association. Hypertension. 2021;78:e26–e37.
Knaeps S, Bourgois JG, Charlier R, Mertens E, Lefevre J, Wijndaele K. Ten-year change in sedentary behaviour, moderate-to-vigorous physical activity, cardiorespiratory fitness and cardiometabolic risk: independent associations and mediation analysis. Br J Sports Med. 2018;52:1063–8.
Welty FK. Dietary treatment to lower cholesterol and triglyceride and reduce cardiovascular risk. Curr Opin Lipidol. 2020;31:206–31.
Author information
Authors and Affiliations
Contributions
Conceptualisation (AN, MD, GS), Methodology (AN, MD, GS), Statistical Analysis (AN, GS), Writing Manuscript (AN, MD, GS), Editing (AN, MD, GS).
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nevill, A.M., Duncan, M.J. & Sandercock, G. Modelling the direct and indirect associations between anthropometric and behavioural factors when predicting atherogenic risk index (TC/HDL-C) ratio. Int J Obes 49, 1856–1863 (2025). https://doi.org/10.1038/s41366-025-01835-0
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41366-025-01835-0