Abstract
Objective
Obesity is a heterogeneous condition that leads to diverse cardiovascular and metabolic outcomes. This study aimed to identify the primary visceral fats contributing to metabolically unhealthy obesity and to investigate the characteristics of fat distribution associated with different obesity-related complications.
Methods
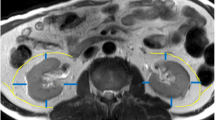
A retrospective analysis was conducted on fat-selective magnetic resonance images (MRI) from 319 individuals with a BMI ≥24 kg/m². Participants were categorized into four groups: solely obesity, T2DM, hypertension, and dyslipidemia, to examine differences in the distribution of hepatic, pancreatic, preperitoneal, mesenteric, and perirenal fat (PrFT). Correlation analyses were performed to elucidate relationships between visceral fat deposits and obesity-related characteristics. Logistic regression identified key fat deposition sites associated with common obesity-related complications. Additionally, the limitations of single-site fat measurements in capturing the heterogeneity of obesity were examined.
Results
PrFT exhibited the strongest correlation with blood pressure (r = 0.225 ~ 0.306, all p < 0.001) among all visceral fats, and the hypertensive individuals with obesity presented the highest PrFT. Hepatic fat showed the highest association with glucose metabolism (r = 0.188 ~ 0.407 all p < 0.01), as evidenced by higher hepatic fat content in the T2DM group compared to other groups. Risk of metabolic syndrome increased by 3.06-fold (95% CI:1.35–6.93, p = 0.007) and 6.79-fold (95% CI:2.45–18.83, p < 0.001) with moderate and severe fatty steatosis compared to those without hepatic steatosis. A 2.24-fold (95% CI:1.27–3.97, p = 0.006) increase in metabolic syndrome likelihood was observed for each 1 cm increment in PrFT.
Conclusions
Besides hepatic fat, perirenal fat is also a key determinant for metabolic syndrome. Patients with various metabolic abnormalities present distinct patterns of visceral fat distribution, which could be simply profiled by perirenal and hepatic fat quantification.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The datasets generated and analyzed during the current study are available from the corresponding authors on reasonable request.
References
Tanriover C, Copur S, Gaipov A, Ozlusen B, Akcan RE, Kuwabara M, et al. Metabolically healthy obesity: misleading phrase or healthy phenotype?. Eur J Intern Med. 2023;111:5–20.
Tsatsoulis A, Paschou SA. Metabolically healthy obesity: criteria, epidemiology, controversies, and consequences. Curr Obes Rep. 2020;9:109–20.
Mongraw-Chaffin M, Foster MC, Anderson CAM, Burke GL, Haq N, Kalyani RR, et al. Metabolically healthy obesity, transition to metabolic syndrome, and cardiovascular risk. J Am Coll Cardiol. 2018;71:1857–65.
Mayoral LPC, Andrade GM, Mayoral EPC, Huerta TH, Canseco SP, Rodal Canales FJ, et al. Obesity subtypes, related biomarkers & heterogeneity. Indian J Med Res. 2020;151:11–21.
Stability of metabolically healthy obesity over 8 years: the English Longitudinal Study of Ageing-PubMed. 2023. https://pubmed.ncbi.nlm.nih.gov/26286585/.
Gao M, Lv J, Yu C, Guo Y, Bian Z, Yang R, et al. Metabolically healthy obesity, transition to unhealthy metabolic status, and vascular disease in Chinese adults: a cohort study. PLoS Med. 2020;17:e1003351.
Eckel N, Li Y, Kuxhaus O, Stefan N, Hu FB, Schulze MB. Transition from metabolic healthy to unhealthy phenotypes and association with cardiovascular disease risk across BMI categories in 90 257 women (the Nurses’ Health Study): 30 year follow-up from a prospective cohort study. Lancet Diabetes Endocrinol. 2018;6:714–24.
Neeland IJ, Poirier P, Després JP. Cardiovascular and metabolic heterogeneity of obesity: clinical challenges and implications for management. Circulation. 2018;137:1391–406.
Hwang YC, Hayashi T, Fujimoto WY, Kahn SE, Leonetti DL, McNeely MJ, et al. Visceral abdominal fat accumulation predicts the conversion of metabolically healthy obese subjects to an unhealthy phenotype. Int J Obes. 2015;39:1365–70.
Kang YM, Jung CH, Cho YK, Jang JE, Hwang JY, Kim EH, et al. Visceral adiposity index predicts the conversion of metabolically healthy obesity to an unhealthy phenotype. PloS One. 2017;12:e0179635.
Neeland IJ, Ross R, Després JP, Matsuzawa Y, Yamashita S, Shai I, et al. Visceral and ectopic fat, atherosclerosis, and cardiometabolic disease: a position statement. Lancet Diabetes Endocrinol. 2019;7:715–25.
Cypess AM. Reassessing human adipose tissue. N Engl J Med. 2022;386:768–79.
Petrov MS, Taylor R. Intra-pancreatic fat deposition: bringing hidden fat to the fore. Nat Rev Gastroenterol Hepatol. 2021. https://www.nature.com/articles/s41575-021-00551-0.
Christensen RH, Hansen CS, Scholten BJ, Jensen MT, Pedersen BK, Schnohr P, et al. Epicardial and pericardial adipose tissues are associated with reduced diastolic and systolic function in type 2 diabetes. Diabetes Obes Metab. 2019;21:2006–11.
Bilski J, Mazur-Bialy A, Wojcik D, Surmiak M, Magierowski M, Sliwowski Z, et al. Role of obesity, mesenteric adipose tissue, and adipokines in inflammatory bowel diseases. Biomolecules. 2019;9:780.
Chinese Diabetes Society. Guideline for the prevention and treatment of type 2 diabetes mellitus in China (2020 edition). Chin J Diabetes. 2021;13:315–409.
Joint Committee for Guideline Revision. 2018 Chinese Guidelines for Prevention and Treatment of Hypertension-A report of the Revision Committee of Chinese Guidelines for Prevention and Treatment of Hypertension. J Geriatr Cardiol JGC. 2019;16:182–241.
Joint committee for guideline revision. 2016 Chinese guidelines for the management of dyslipidemia in adults. J Geriatr Cardiol JGC. 2018;15:1–29.
Chinese Medical Association Chinese Society of Endocrinology. Guideline for the diagnosis and management of hyperuricemia and gout in China (2019 edition). Chin J Endocrinol Metab. 2019;36:1–13.
Yang X, Li J, Hu D, Chen J, Li Y, Huang J, et al. Predicting the 10-year risks of atherosclerotic cardiovascular disease in Chinese population: the China-PAR Project (Prediction for ASCVD Risk in China). Circulation. 2016;134:1430–40.
Liu F, Li J, Chen J, Hu D, Li Y, Huang J, et al. Predicting lifetime risk for developing atherosclerotic cardiovascular disease in Chinese population: the China-PAR project. Sci Bull. 2018;63:779–87.
Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–47.
Liu KH, Chan YL, Chan WB, Chan JCN, Chu CWW. Mesenteric fat thickness is an independent determinant of metabolic syndrome and identifies subjects with increased carotid intima-media thickness. Diabetes Care. 2006;29:379–84.
Liu KH, Chu WCW, To KW, Ko FWS, Ng SSS, Ngai JCL, et al. Mesenteric fat thickness is associated with increased risk of obstructive sleep apnoea. Respirol Carlton Vic. 2014;19:92–7.
Liu KH, Kong APS, Chan JCN, Wing WC. Sonographic measurement of mesenteric fat thickness is a better predictor of aortic stiffness compared with conventional obesity indexes. Ultrasound Med Biol. 2023;49:599–606.
Boorsma EM, Sorimachi H, Ter Maaten JM, van Veldhuisen DJ, Omote K, Takahashi N, et al. Perirenal adipose tissue is associated with renal dysfunction and abnormal hemodynamics in patients with HFpEF. JACC Heart Fail. 2023;11:1463–5.
Chen X, Mao Y, Hu J, Han S, Gong L, Luo T, et al. Perirenal fat thickness is significantly associated with the risk for development of chronic kidney disease in patients with diabetes. Diabetes. 2021;70:2322–32.
Acknowledgements
The authors sincerely acknowledge the invaluable collaboration and support provided by all the members of the “3+N” multidisciplinary weight loss program, Medical Center for Comprehensive Weight Control, the Third Affiliated Hospital of Sun Yat-Sen University. The authors also wish to thank all subjects who participated in this study.
Funding
This study was funded by National Natural Science Foundation of China (Grant 82270886, Grant 82302222), Guangdong Basic and Applied Basic Research Foundation (Grant 2023A1515220121), Sci-Tech Research Development Program of Guangzhou City (202201020589) and Clinical Research 5010 Program (Grant 2023006), Fundamental Research Funds for the Central Universities, Sun Yat-sen University.
Author information
Authors and Affiliations
Contributions
Jie Zeng, Yixin Chen and Ting Zhang designed this study and drafted the manuscript. Yixin Chen, Ruomi Guo, Baoding Qin, Yang Yi conducted MRI and statistical analyses. Ruomi Guo offered technical support in MRI sequences. Wu Lin, Yuchan Wang, and Zijian Mo were responsible for the curation of clinical data, and the acquisition of consent from study subjects. Mengyin Cai and Guojun Shi were responsible for result verification. Yanming Chen, Jie Zeng, and Yanhua Zhu initiated this study, edited the manuscript, and supervised this research.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study protocols were approved by the ethics committee of the Third Affiliated Hospital of Sun Yat-sen University (Ethical approval number: II2023-075-02). All methods were performed in accordance with the relevant guidelines and regulations. Written informed consent was obtained from each participant.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, Y., Zhang, T., Qin, B. et al. Perirenal fat: a neglected fat depot shaping heterogeneity of obesity along with hepatic fat. Int J Obes 49, 2265–2272 (2025). https://doi.org/10.1038/s41366-025-01874-7
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41366-025-01874-7