Abstract
Objectives
The association between obesity and cholelithiasis has been identified. However, the causal relationship between age-specific childhood obesity and adult cholelithiasis remains unclear. In addition, the biological basis for the association between childhood obesity and adult cholelithiasis is poorly understood, which poses a challenge for preventing adult cholelithiasis in specific biological pathways.
Methods
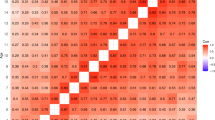
Summary statistics of genome-wide association studies (GWASs) of childhood age-specific body mass index (BMI) at 12 time points and adult cholelithiasis derived from FinnGen were used in this study, with the former covering data from birth to 8 years. Linkage disequilibrium score regression (LDSC) analyses were used to assess the genetic correlations of age-specific childhood BMI to cholelithiasis. Two-sample Mendelian randomization (MR) and multivariable Mendelian randomization (MVMR) analyses were utilized to explore the causal associations. As downstream analyses, summary-based Mendelian randomization (SMR) analyses, transcriptome-wide association studies (TWAS), and Bayesian colocalization were conducted to discover the shared transcriptomic signals. The GWAS summary statistics of cholelithiasis from the UK Biobank were used for sensitivity analyses.
Results
LDSC analyses revealed significant genetic correlations between 11 age-specific childhood BMIs and adult cholelithiasis (except for birth BMI). Two-sample MR and MVMR analyses indicated causal relationships between birth BMI and BMI at 8 months, 1.5 years, 7 years, and 8 years after birth and adult cholelithiasis. SMR, TWAS, and colocalization analyses identified MLXIPL as the strongest overlapping signal between age-specific BMI and adult cholelithiasis.
Conclusion
This study provides new evidence on the relationships between childhood obesity and adult cholelithiasis, highlighting the role of early intervention for obesity in childhood at key time points. MLXIPL gene expression was identified as a potential biological pathway, suggesting potential therapeutic targets and precise intervention strategies for childhood obesity and adult cholelithiasis.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
GWAS summary statistics for 12 age-specific BMIs are available at: https://www.fhi.no/en/studies/moba/for-forskere-artikler/gwas-data-from-moba/. GWAS summary statistics for cholelithiasis from the FinnGen is available at: https://finngen.gitbook.io/documentation. GWAS summary statistics for cholelithiasis from the UKB is available at: https://www.leelabsg.org/resources. GWAS summary statistics for adolescent BMI is available at: EGG (Early Growth Genetics) Consortium. The eQTL summary data for GTEx are available at: https://yanglab.westlake.edu.cn/software/smr/#DataResource. The eQTL summary data for eQTLGen Consortium is available at: https://eqtlgen.org/cis-eqtls.html.The tissue weights for GTEx are available at: http://gusevlab.org/projects/fusion/.
References
Lammert F, Gurusamy K, Ko CW, Miquel J-F, Méndez-Sánchez N, Portincasa P, et al. Gallstones. Nat Rev Dis Prim. 2016;2:16024.
Wang X, Yu W, Jiang G, Li H, Li S, Xie L, et al. Global epidemiology of gallstones in the 21st Century: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2024;22:1586–95.
Stinton LM, Myers RP, Shaffer EA. Epidemiology of gallstones. Gastroenterol Clin. 2010;39:157–69.
Aerts R, Penninckx F. The burden of gallstone disease in Europe. Aliment Pharmacol Therapeutics. 2003;18:49–53.
Russo MW, Wei JT, Thiny MT, Gangarosa LM, Brown A, Ringel Y, et al. Digestive and liver diseases statistics, 2004. Gastroenterology. 2004;126:1448–53.
Beckingham IJ. ABC of diseases of liver, pancreas, and biliary system. Gallstone disease. BMJ (Clinical research ed). 2001;322:91–4.
Schafmayer C, Hartleb J, Tepel J, Albers S, Freitag S, Völzke H, et al. Predictors of gallstone composition in 1025 symptomatic gallstones from Northern Germany. BMC Gastroenterol. 2006;6:36.
Stinton LM, Shaffer EA. Epidemiology of gallbladder disease: cholelithiasis and cancer. Gut Liver. 2012;6:172–87.
Koller T, Kollerova J, Hlavaty T, Huorka M, Payer J. Cholelithiasis and markers of nonalcoholic fatty liver disease in patients with metabolic risk factors. Scand J Gastroenterol. 2012;47:197–203.
Bortnichak EA, Freeman DH Jr., Ostfeld AM, Castelli WP, Kannel WB, Feinleib M, et al. The association between cholesterol cholelithiasis and coronary heart disease in Framingham, Massachusetts. Am J Epidemiol. 1985;121:19–30.
Frybova B, Drabek J, Lochmannova J, Douda L, Hlava S, Zemkova D, et al. Cholelithiasis and choledocholithiasis in children; risk factors for development. PloS One. 2018;13:e0196475.
Fradin K, Racine AD, Belamarich PF. Obesity and symptomatic cholelithiasis in childhood: epidemiologic and case-control evidence for a strong relation. J Pediatr Gastroenterol Nutr. 2014;58:102–6.
Hendarto H, Akbar F, Muzakki J, Amri R, Nugraha S, Adlani H. Obesity, dyslipidemia, and diabetes mellitus as risk factors in cholelithiasis. Electron J Gen Med. 2023;20:em549.
Chen L, Yang H, Li H, He C, Yang L, Lv G. Insights into modifiable risk factors of cholelithiasis: a Mendelian randomization study. Hepatology. 2022;75:785–96.
Kharga B, Sharma BK, Singh VK, Nishant K, Bhutia P, Tamang R, et al. Obesity not necessary, risk of symptomatic cholelithiasis increases as a function of BMI. J Clin Diagnostic Res. 2016;10:Pc28–pc32.
Khera AV, Chaffin M, Wade KH, Zahid S, Brancale J, Xia R, et al. Polygenic prediction of weight and obesity trajectories from birth to adulthood. Cell. 2019;177:587–96.e9.
Yuan S, Ruan X, Sun Y, Fu T, Zhao J, Deng M, et al. Birth weight, childhood obesity, adulthood obesity and body composition, and gastrointestinal diseases: a Mendelian randomization study. Obesity. 2023;31:2603–14.
Xu X, Gao J, Sun J, Liu R, Chen W. The role of metabolic factors in the association between obesity and cholelithiasis: a two-step, two-sample multivariable Mendelian randomization study. Clinics. 2024;79:100520.
Zheng J, Erzurumluoglu AM, Elsworth BL, Kemp JP, Howe L, Haycock PC, et al. LD Hub: a centralized database and web interface to perform LD score regression that maximizes the potential of summary level GWAS data for SNP heritability and genetic correlation analysis. Bioinformatics. 2017;33:272–9.
Davey Smith G, Hemani G. Mendelian randomization: genetic anchors for causal inference in epidemiological studies. Hum Mol Genet. 2014;23:R89–R98.
Sanderson E, Glymour MM, Holmes MV, Kang H, Morrison J, Munafò MR, et al. Mendelian randomization. Nat Rev Methods Primers. 2022;2.
Zhu Z, Zhang F, Hu H, Bakshi A, Robinson MR, Powell JE, et al. Integration of summary data from GWAS and eQTL studies predicts complex trait gene targets. Nat Genet. 2016;48:481–7.
Gusev A, Ko A, Shi H, Bhatia G, Chung W, Penninx BW, et al. Integrative approaches for large-scale transcriptome-wide association studies. Nat Genet. 2016;48:245–52.
Wu Y, Broadaway KA, Raulerson CK, Scott LJ, Pan C, Ko A, et al. Colocalization of GWAS and eQTL signals at loci with multiple signals identifies additional candidate genes for body fat distribution. Hum Mol Genet. 2019;28:4161–72.
Zhu Z, Hasegawa K, Camargo CA Jr., Liang L. Investigating asthma heterogeneity through shared and distinct genetics: insights from genome-wide cross-trait analysis. J Allergy Clin Immunol. 2021;147:796–807.
Luo S, Zheng MH, Wong VW, Au Yeung SL. Drug-target Mendelian randomisation applied to metabolic dysfunction-associated steatotic liver disease: opportunities and challenges. eGastroenterology. 2024;2:e100114.
Skrivankova VW, Richmond RC, Woolf BAR, Yarmolinsky J, Davies NM, Swanson SA, et al. Strengthening the reporting of observational studies in epidemiology using Mendelian randomization: the STROBE-MR statement. JAMA. 2021;326:1614–21.
Magnus P, Birke C, Vejrup K, Haugan A, Alsaker E, Daltveit AK, et al. Cohort profile update: the Norwegian Mother and Child Cohort Study (MoBa). Int J Epidemiol. 2016;45:382–8.
Helgeland Ø, Vaudel M, Sole-Navais P, Flatley C, Juodakis J, Bacelis J, et al. Characterization of the genetic architecture of infant and early childhood body mass index. Nat Metab. 2022;4:344–58.
Kurki MI, Karjalainen J, Palta P, Sipilä TP, Kristiansson K, Donner KM, et al. FinnGen provides genetic insights from a well-phenotyped isolated population. Nature. 2023;613:508–18.
Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015;12:e1001779.
Grotzinger AD, Fuente J, Privé F, Nivard MG, Tucker-Drob EM. Pervasive downward bias in estimates of liability-scale heritability in genome-wide association study meta-analysis: a simple solution. Biol Psychiatry. 2023;93:29–36.
Burrows K, Heiskala A, Bradfield JP, Balkhiyarova Z, Ning L, Boissel M, et al. A framework for conducting GWAS using repeated measures data with an application to childhood BMI. Nat Commun. 2024;15:10067.
Bulik-Sullivan B, Finucane HK, Anttila V, Gusev A, Day FR, Loh PR, et al. An atlas of genetic correlations across human diseases and traits. Nat Genet. 2015;47:1236–41.
Davey Smith G, Hemani G. Mendelian randomization: genetic anchors for causal inference in epidemiological studies. Hum Mol Genet. 2014;23:R89–98.
Burgess S, Cronjé HT. Incorporating biological and clinical insights into variant choice for Mendelian randomisation: examples and principles. eGastroenterology. 2024;2:e100042.
Burgess S, Thompson SG. Avoiding bias from weak instruments in Mendelian randomization studies. Int J Epidemiol. 2011;40:755–64.
Burgess S, Scott RA, Timpson NJ, Davey Smith G, Thompson SG. Using published data in Mendelian randomization: a blueprint for efficient identification of causal risk factors. Eur J Epidemiol. 2015;30:543–52.
Perry BI, Burgess S, Jones HJ, Zammit S, Upthegrove R, Mason AM, et al. The potential shared role of inflammation in insulin resistance and schizophrenia: a bidirectional two-sample mendelian randomization study. PLoS Med. 2021;18:e1003455.
Bowden J, Davey Smith G, Burgess S. Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol. 2015;44:512–25.
Bowden J, Davey Smith G, Haycock PC, Burgess S. Consistent estimation in Mendelian randomization with some invalid instruments using a weighted Median Estimator. Genet Epidemiol. 2016;40:304–14.
Wu Y, Zeng J, Zhang F, Zhu Z, Qi T, Zheng Z, et al. Integrative analysis of omics summary data reveals putative mechanisms underlying complex traits. Nat Commun. 2018;9:918.
Kia DA, Zhang D, Guelfi S, Manzoni C, Hubbard L, Reynolds RH, et al. Identification of candidate Parkinson disease genes by integrating genome-wide association study, expression, and epigenetic data sets. JAMA Neurol. 2021;78:464–72.
Reilly JJ, Armstrong J, Dorosty AR, Emmett PM, Ness A, Rogers I, et al. Early life risk factors for obesity in childhood: cohort study. BMJ. 2005;330:1357.
Ståhlberg D, Rudling M, Angelin B, Björkhem I, Forsell P, Nilsell K, et al. Hepatic cholesterol metabolism in human obesity. Hepatology. 1997;25:1447–50.
Mathus-Vliegen EM, Van Ierland-Van Leeuwen ML, Terpstra A. Determinants of gallbladder kinetics in obesity. Digest Dis Sci. 2004;49:9–16.
Wang HH, Liu M, Clegg DJ, Portincasa P, Wang DQ. New insights into the molecular mechanisms underlying effects of estrogen on cholesterol gallstone formation. Biochim Biophys Acta. 2009;1791:1037–47.
Kansra AR, Lakkunarajah S, Jay MS. Childhood and adolescent obesity: a review. 2021;8:2020.
Su Y, Zhang Y, Chai Y, Xu J. Autoimmune diseases and their genetic link to bronchiectasis: insights from a genetic correlation and Mendelian randomization study. Front Immunol. 2024;15:1343480.
Gluckman PD, Hanson MAJElooh, disease. The developmental origins of health and disease. 2006:1–7.
Lacagnina S. The Developmental Origins of Health and Disease (DOHaD). Am J Lifestyle Med. 2020;14:47–50.
Wadhwa PD, Buss C, Entringer S, Swanson JM. Developmental origins of health and disease: brief history of the approach and current focus on epigenetic mechanisms. Semin Reprod Med. 2009;27:358–68.
Chmurzynska A. Fetal programming: link between early nutrition, DNA methylation, and complex diseases. Nutr Rev. 2010;68:87–98.
Gluckman PD, Hanson MA, Cooper C, Thornburg KL. Effect of in utero and early-life conditions on adult health and disease. N Engl J Med. 2008;359:61–73.
Aris IM, Block JP. Childhood obesity interventions—going beyond the individual. JAMA Pediatr. 2022;176:e214388–e.
Kooner JS, Chambers JC, Aguilar-Salinas CA, Hinds DA, Hyde CL, Warnes GR, et al. Genome-wide scan identifies variation in MLXIPL associated with plasma triglycerides. Nat Genet. 2008;40:149–51.
Smelt AH. Triglycerides and gallstone formation. Clin Chim Acta. 2010;411:1625–31.
Nicolopoulos K, Mulugeta A, Zhou A, Hyppönen E. Association between habitual coffee consumption and multiple disease outcomes: a Mendelian randomisation phenome-wide association study in the UK Biobank. Clin Nutr. 2020;39:3467–76.
Chen VL, Du X, Chen Y, Kuppa A, Handelman SK, Vohnoutka RB, et al. Genome-wide association study of serum liver enzymes implicates diverse metabolic and liver pathology. Nat Commun. 2021;12:816.
Acknowledgements
We express our gratitude to the patients and investigators who have contributed to MoBa Cohort, the FinnGen Consortium, the UK Biobank (UKB), the Genotype-Tissue Expression Project (GTEx), the eQTLGen Consortium and the Early Growth Genetics Consortium.
Funding
This study was supported by the Sichuan Provincial Science and Technology Support Program (2023YFH0097, Yu Tong).
Author information
Authors and Affiliations
Contributions
Lihua Liu, Writing - original draft, Conceptualization, Formal analysis, Validation. Lu Zhang, Supervision, Writing –review & editing. Yiwen Liao, Formal analysis, Investigation. Xin Jin, Resources, Validation. Yunzhu Chen, Resources, Software. Tian Yang, Visualization. Xingxing Li, Supervision. Yuheng Cao, Validation. Chuan Yu, Supervision. Chenghan Xiao, Methodology, Conceptualization. Zhenmi Liu, Writing - review & editing, Supervision. Yu Tong, Writing –review & editing, Supervision. All authors reviewed and approved the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study adheres to the STROBE-MR guidelines. Each included GWAS was conducted with institutional review board approval and informed participant consent. The MoBa study protocol was approved by the administrative board of the Norwegian Institute of Public Health, with data collection authorized by the Norwegian Data Protection Agency and the Regional Committee for Medical Research Ethics (approval number: 2012/67). The UK Biobank received ethics approval from the North West Multi-Centre Research Ethics Committee. The FinnGen GWAS data were approved by the Coordinating Ethics Committee of the Hospital District of Helsinki and Uusimaa (HUS; approval number: HUS/990/2017). The GWAS data for adolescent BMI from the EGG Consortium were obtained from ethically approved studies, with each contributing cohort receiving approval from its respective local ethics committee. Other datasets used (GTEx, eQTLGen, and tissue weight data) are publicly available summary-level data generated from studies conducted under appropriate ethical approvals and informed consent. No new ethical approval was required for this analysis.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, L., Zhang, L., Liao, Y. et al. Age-specific childhood obesity and adult cholelithiasis: association and shared transcriptomic bases. Int J Obes 49, 2295–2302 (2025). https://doi.org/10.1038/s41366-025-01877-4
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41366-025-01877-4