Abstract
Aim
To comprehensively investigate the long-term risk of all-cause mortality associated with general and central obesity in patients with inflammatory bowel disease (IBD).
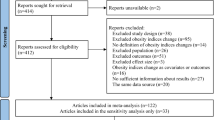
Methods
Overall, 5107 IBD patients [mean age 57.0 (SD: 8.0) years; 51.7% female] were included in the prospective cohort. General obesity was assessed using body mass index (BMI), while central obesity was evaluated using hip circumference, waist circumference (WC), waist-to-hip ratio (WHR), weight-adjusted waist index (WWI), conicity index (CI) and A Body Shape Index (ABSI). Primary outcome was all-cause death. Cox proportional hazards models were employed to examine the associations.
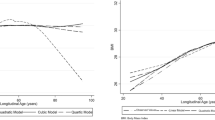
Results
During a median of 14.6 years’ follow-up, 591 all-cause deaths occurred. At baseline, 1681(32.9%), 2229(43.6%), 1161(22.7%) and 36(0.70%) patients were BMI-defined normal, overweight, obesity and underweight. Underweight individuals had a 2.22-fold increased mortality risk than those with normal BMI (HR = 3.22, 95% CI:1.70–6.11), while null associations were observed for overweight or obesity. As for central obesity, individuals with the highest quartiles of WC (HR = 1.34, 1.02–1.76), WHR (HR = 1.56, 1.13–2.15), WWI (HR = 1.64, 1.24–2.16), CI (HR = 1.72, 1.28–2.30) and ABSI (HR = 1.64, 1.23–2.20) had a 34%, 56%, 64%, 72% and 64% greater mortality risk versus the lowest quartiles, with significant dose-response relationships (all P values < 0.05).
Conclusions
Central obesity and underweight, rather than general obesity, are associated with an increased risk of all-cause mortality in IBD patients. These findings underscore the importance of adequate nutrition and reduced visceral adiposity for long-term prognosis improvement of IBD patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The data underlying this study are available in the paper and in its online supplementary material. The data will be shared on reasonable request to the corresponding author.
References
Kaplan GG, Windsor JW. The four epidemiological stages in the global evolution of inflammatory bowel disease. Nat Rev Gastroenterol Hepatol. 2021;18:56–66.
Rogler G, Singh A, Kavanaugh A, Rubin DT. Extraintestinal manifestations of inflammatory bowel disease: current concepts, treatment, and implications for disease management. Gastroenterology. 2021;161:1118–32.
Wang R, Li Z, Liu S, Zhang D. Global, regional and national burden of inflammatory bowel disease in 204 countries and territories from 1990 to 2019: a systematic analysis based on the Global Burden of Disease Study 2019. BMJ Open. 2023;13:e065186.
Fang H, Berg E, Cheng X, Shen W. How to best assess abdominal obesity. Curr Opin Clin Nutr Metab Care. 2018;21:360–5.
Nagayama D, Fujishiro K, Watanabe Y, Yamaguchi T, Suzuki K, Saiki A et al. A Body Shape Index (ABSI) as a variant of conicity index not affected by the obesity paradox: a cross-sectional study using arterial stiffness parameter. J Pers Med. 2022;12:2014.
Park Y, Kim NH, Kwon TY, Kim SG. A novel adiposity index as an integrated predictor of cardiometabolic disease morbidity and mortality. Sci Rep. 2018;8:16753.
Singh S, Dulai PS, Zarrinpar A, Ramamoorthy S, Sandborn WJ. Obesity in IBD: epidemiology, pathogenesis, disease course and treatment outcomes. Nat Rev Gastroenterol Hepatol. 2017;14:110–21.
Flores A, Burstein E, Cipher DJ, Feagins LA. Obesity in inflammatory bowel disease: a marker of less severe disease. Dig Dis Sci. 2015;60:2436–45.
Lynn AM, Harmsen WS, Tremaine WJ, Bazerbachi F, Dayyeh BKA, Loftus EV. Su1887 Impact of Obesity on Future IBD Related Complications in a Population-Based Cohort of Crohn’s Disease (CD) and Ulcerative Colitis (UC) Patients. Gastroenterology. 2018;154:S620.
Johnson AM, Harmsen WS, Aniwan S, Tremaine WJ, Abu Dayyeh BK, Loftus EV. Prevalence and impact of obesity on disease-specific outcomes in a population-based cohort of patients with ulcerative colitis. J Crohns Colitis. 2021;15:1816–23.
Erhayiem B, Dhingsa R, Hawkey CJ, Subramanian V. Ratio of visceral to subcutaneous fat area is a biomarker of complicated Crohn’s disease. Clin Gastroenterol Hepatol. 2011;9:684–7.e1.
Sehgal P, Su S, Zech J, Nobel Y, Luk L, Economou I, et al. Visceral adiposity independently predicts time to flare in inflammatory bowel disease but body mass index does not. Inflamm Bowel Dis. 2024;30:594–601.
Harper JW, Sinanan MN, Zisman TL. Increased body mass index is associated with earlier time to loss of response to infliximab in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2013;19:2118–24.
Jain A, Limketkai BN, Hutfless S. Mo1243 The effect of obesity on post-surgical complications during hospitalizations for inflammatory bowel disease: a nationwide analysis. Gastroenterology. 2014;146:S-595–6.
Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015;12:e1001779.
WHO. Obesity and overweight. 2024:Obesity and overweight fact sheet from WHO providing key facts and information on causes, health consequences, double burden of disease, prevention, WHO response. WHO; 2024.
Li F, Ramirez Y, Yano Y, Daniel CR, Sharma SV, Brown EL, et al. The association between inflammatory bowel disease and all-cause and cause-specific mortality in the UK Biobank. Ann Epidemiol. 2023;88:15–22.
Marrie RA, Graff LA, Fisk JD, Patten SB, Bernstein CN. The relationship between symptoms of depression and anxiety and disease activity in IBD over time. Inflamm Bowel Dis. 2021;27:1285–93.
Mikocka-Walus A, Pittet V, Rossel J, von Känel R. Symptoms of depression and anxiety are independently associated with clinical recurrence of inflammatory bowel disease. Clin Gastroenterol Hepatol. 2016;14:829–35.e1.
Massironi S, Viganò C, Palermo A, Pirola L, Mulinacci G, Allocca M, et al. Inflammation and malnutrition in inflammatory bowel disease. Lancet Gastroenterol Hepatol. 2023;8:579–90.
Singer-Englar T, Barlow G, Mathur R. Obesity, diabetes, and the gut microbiome: an updated review. Expert Rev Gastroenterol Hepatol. 2019;13:3–15.
Lv Y, Zhang Y, Li X, Gao X, Ren Y, Deng L, et al. Body mass index, waist circumference, and mortality in subjects older than 80 years: a Mendelian randomization study. Eur Heart J. 2024;45:2145–54.
Uko V, Vortia E, Achkar J, Karakas P, Fiocchi C, Worley S, et al. Impact of abdominal visceral adipose tissue on disease outcome in pediatric Crohn’s disease. Inflamm Bowel Dis. 2014;20:2286–91.
Tchernof A, Després J. Pathophysiology of human visceral obesity: an update. Physiol Rev. 2013;93:359–404.
Mondanelli G, Albini E, Orecchini E, Pallotta MT, Belladonna ML, Ricci G, et al. Pathogenetic interplay between IL-6 and tryptophan metabolism in an experimental model of obesity. Front Immunol. 2021;12:713989.
Friedman J. The long road to leptin. J Clin Investig. 2016;126:4727–34.
Meijnikman AS, Gerdes VE, Nieuwdorp M, Herrema H. Evaluating causality of gut microbiota in obesity and diabetes in humans. Endocr Rev. 2018;39:133–53.
Lavelle A, Sokol H. Gut microbiota-derived metabolites as key actors in inflammatory bowel disease. Nat Rev Gastroenterol Hepatol. 2020;17:223–37.
Lloyd-Price J, Arze C, Ananthakrishnan AN, Schirmer M, Avila-Pacheco J, Poon TW, et al. Multi-omics of the gut microbial ecosystem in inflammatory bowel diseases. Nature. 2019;569:655–62.
Martínez-Domínguez SJ, García-Mateo S, Gargallo-Puyuelo CJ, Gallego-Llera B, Callau P, Mendi C, et al. Inflammatory bowel disease is an independent risk factor for metabolic dysfunction-associated steatotic liver disease in lean individuals. Inflamm Bowel Dis. 2024;30:1274–83.
Dreesen E, Verstockt B, Bian S, de Bruyn M, Compernolle G, Tops S, et al. Evidence to support monitoring of vedolizumab trough concentrations in patients with inflammatory bowel diseases. Clin Gastroenterol Hepatol. 2018;16:1937–46.e8.
Mulinacci G, Pirola L, Gandola D, Ippolito D, Viganò C, Laffusa A, et al. Ultrasound muscle assessment for sarcopenia detection in inflammatory bowel disease: a prospective study. U Eur Gastroenterol J. 2024;12:562–73.
Funding
This work was supported by the National Key Research and Development Program of China (No. 2022YFC3602100 and 2022YFC3602104), Beijing Nova Program (No. 20230484349) and Beijing Hospitals Authority Innovation Studio of Young Staff (No. 202303). None of the funding organizations had any role in the design and conduct of the study; in the collection, analysis and interpretation of the data; in the preparation, review and approval of the manuscript.
Author information
Authors and Affiliations
Contributions
SSW and ZRY designed the study. QZ and YTW drafted the manuscript. QZ and YTW analyzed the data. SSW and QZ verified the analysis. SL, STZhu, PL, STZhang and ZRY interpreted the results, incorporated comments for the co-authors and finalized the manuscript. All authors approved the final version of the paper.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, Q., Wang, Y., Liu, S. et al. Mortality risk associated with general and central obesity in inflammatory bowel disease patients: a long-term prospective cohort study. Int J Obes 49, 2303–2310 (2025). https://doi.org/10.1038/s41366-025-01879-2
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41366-025-01879-2