Abstract
Background
The impact of body weight disorders on outcomes of patients undergoing cardiac surgery for infective endocarditis (IE) have been poorly studied. Obesity or malnutrition may significantly influence the course and prognosis of endocarditis, driven by distinct comorbidities and microbiological profiles. Hence, we investigated the impact of preoperative body mass index (BMI) on postoperative outcomes in a large multicentric cohort of surgically treated IE patients.
Methods
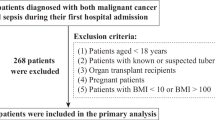
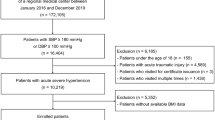
Data from the Clinical Multicenter Project for Analysis of Infective Endocarditis in Germany (CAMPAIGN) registry (n = 4917) was used for retrospective analysis. The patients were divided into four groups for comparison according to their BMI: (1) underweight (≤18.5 kg/m2), (2) normal-weight (18.6–24.9 kg/m2), (3) overweight (25.0–29.9 kg/m2), (4) obesity (≥30.0 kg/m2). Patients with incomplete data on body weight or height were excluded (n = 116). The primary outcomes were 30-day and 1-year mortality.
Results
The final study cohort comprised 4801 patients, including 133 underweight patients (2.8%), 1884 normal-weight patients (39.2%), 1797 patients with overweight (37.4%), and 987 patients with obesity (20.6%). The mean age in the entire cohort was 65.0 [54.0–73.0] years. Patients with obesity had more comorbidities, including hypertension (63.0%; p < 0.001), diabetes mellitus (45.7%, p < 0.001), coronary artery disease (29.5%; p < 0.001), previous cardiac surgery (32.2%, p < 0.012) and dialysis-dependent chronic kidney disease (11.6%, p < 0.001). Patients with obesity had the highest prevalence of staphylococcal endocarditis (33.4%; p < 0.001), while underweight patients had more streptococcal infection (22.0%; p < 0.001). Patients with obesity had the worst 30-day and 1-year mortality rates after surgery for IE (14.1% and 19.6%, p < 0.001 and p < 0.001 respectively).
Conclusions
IE patients with obesity present with comorbidities, higher 30-day mortality and lower 1-year survival rates, possibly linked to more frequent staphylococcal infections and comorbidities. This emphasises the need for early risk stratification, enhanced infection prevention and improved perioperative care in patients with obesity.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
Wahadat A, Deckers J, Budde R, van der Meer J, Natour E, Ten Oever J, et al. Implementation of the 2015 European Society of Cardiology guidelines for the management of infective endocarditis in the Netherlands. Neth Heart J. 2020;28:628–36.
Fryar, C. D., Ostchega, Y., Hales, C. M., Zhang, G. & Kruszon-Moran, D. (2017). Hypertension prevalence and control among adults: United States, 2015–2016.
Stival C, Lugo A, Odone A, Van den Brandt PA, Fernandez E, Tigova O, et al. Prevalence and correlates of overweight and obesity in 12 European countries in 2017–2018. Obes Facts. 2022;15:655–65.
Harris CM, Albaeni A, Wright S, Norris KC, editors. Obesity as a risk factor among hospitalized patients with infective endocarditis. Open Forum Infectious Diseases, Oxford: Oxford University Press US; 2019.
World Health Organization. WHO European regional obesity report 2022. WHO European Regional Obesity Report; 2022.
Schienkiewitz A, Kuhnert R, Blume M, Mensink GB. Overweight and obesity among adults in Germany–Results from GEDA 2019/2020-EHIS. J health Monit. 2022;7:21.
Weber C, Gassa A, Rokohl A, Sabashnikov A, Deppe A-C, Eghbalzadeh K, et al. Severity of presentation, not sex, increases risk of surgery for infective endocarditis. Ann Thorac Surg. 2019;107:1111–7.
de Sa DDC, Tleyjeh IM, Anavekar NS, Schultz JC, Thomas JM, Lahr BD, et al. Epidemiological trends of infective endocarditis: a population-based study in Olmsted County, Minnesota. Mayo Clin Proc. 2010;85:422–6.
Luehr M, Weber C, Misfeld M, Lichtenberg A, Tugtekin S-M, Diab M, et al. Virulence of Staphylococcus infection in surgically treated patients with endocarditis: a multicenter analysis. Ann Surg. 2023;277:e1364–e72.
Nguyen Q-S, Choi C, Khoche S. Obesity and its implications for cardiac surgery patients. Int Anesthesiol Clin. 2020;58:34–40.
O’Sullivan KE, Byrne JS, Hudson A, Murphy AM, Sadlier DM, Hurley JP. The effect of obesity on acute kidney injury after cardiac surgery. J Thorac cardiovasc Surg. 2015;150:1622–8.
Engel AM, McDonough S, Smith JM. Does an obese body mass index affect hospital outcomes after coronary artery bypass graft surgery?. Ann Thorac Surg. 2009;88:1793–800.
Krasivskyi I, Eghbalzadeh K, Ivanov B, Gerfer S, Großmann C, Sabashnikov A, et al. Impact of obesity on early in-hospital outcomes after coronary artery bypass grafting surgery in acute coronary syndrome: a propensity score matching analysis. J Clin Med. 2022;11:6805.
McAuley PA, Blair SN. Obesity paradoxes. J sports Sci. 2011;29:773–82.
Banack H, Stokes A. The ‘obesity paradox’may not be a paradox at all. Int J Obes. 2017;41:1162–3.
Johnson AP, Parlow JL, Whitehead M, Xu J, Rohland S, Milne B. Body mass index, outcomes, and mortality following cardiac surgery in Ontario, Canada. J Am Heart Assoc. 2015;4:e002140.
Bai L, Huang J, Wang D, Zhu D, Zhao Q, Li T, et al. Association of body mass index with mortality of sepsis or septic shock: an updated meta-analysis. J Intensive Care. 2023;11:27.
Gatti G, Perrotti A, Obadia JF, Duval X, Iung B, Alla F, et al. Simple scoring system to predict in-hospital mortality after surgery for infective endocarditis. J Am Heart Assoc. 2017;6:e004806.
Weber C, Petrov G, Luehr M, Aubin H, Tugtekin S-M, Borger MA, et al. Surgical results for prosthetic versus native valve endocarditis: a multicenter analysis. J Thorac cardiovasc Surg. 2021;161:609–19. e10.
Ostovar R, Schroeter F, Erb M, Kuehnel R-U, Hartrumpf M, Albes JM. Endocarditis: who is particularly at risk and why? Ten years analysis of risk factors for in-hospital mortality in infective endocarditis. Thorac Cardiovasc Surg. 2023;71:12–21.
Author information
Authors and Affiliations
Consortia
Contributions
AE, CW and ML conceived and supervised the study. AE, CW, SS, MM, MMC, MD, AP, SMT, PA and ML collected and analyzed data of patients with infective endocarditis. AE, CW and ML drafted the article. KM, TD, CH, AL, TW, MAB supervised data collection and interpreted data. SS, MM, MMC, MD, AP, SMT, HA, PA, KM, TD, CH, AL, TW and MAB revised the manuscript critically for important intellectual content. AE, CW and ML performed statistical analyses. All authors agreed to be accountable for their contributions of the work in ensuring that questions related to the accuracy or integrity of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
MAB discloses that his hospital receives speakers’ honoraria and/or consulting fees on his behalf from Edwards Lifesciences, Medtronic, Abbott, and Artivion. The remaining authors have no conflicts of interest or financial relationships with the industry to disclose.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Elderia, A., Weber, C., Saha, S. et al. Impact of preoperative body mass index on postoperative outcomes in infective endocarditis: a multicenter analysis of 4801 consecutive patients. Int J Obes 49, 2364–2371 (2025). https://doi.org/10.1038/s41366-025-01901-7
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41366-025-01901-7