Abstract
Introduction
While the classification of metabolically healthy individuals with obesity remains uncertain, recent research links central obesity to thromboembolism and cardiovascular disease, potentially indicating a hypercoagulable state in some individuals with obesity. This study investigates coagulation and inflammation differences between obesity and normal-weight phenotypes.
Methods
225 adult women, participants were subjected to clinical examinations, and biochemical assessments. These assessments classified participants into four distinct phenotypes, namely MHNW (individuals with Metabolically Healthy Normal Weight), MUNW (individuals with Metabolically Unhealthy Normal Weight), MHO (individuals with Metabolically Healthy Obesity), and MUO (individuals with Metabolically Unhealthy Obesity), based on a combination of body mass index (BMI) and metabolic criteria. Subsequently, hemostatic proteins and interleukin levels were compared.
Results
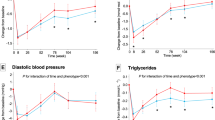
Among 225 female patients, the MHO group was younger, with higher measurements like visceral fat and BMI, while MUO had the highest values in homeostatic model assessment for insulin resistance (HOMA-IR), triglycerides and low-density lipoprotein cholesterol (LDL-c). Coagulation proteins showed normal levels. However, MHNW had significantly lower FV, and groups without obesity (MHNW and MUNW) had lower FVIII and FIX. FXII in MHNW did not significantly differ. Inflammatory markers revealed IL-6 negatively correlated with PC and AT but positively with FVIII and FIX. IL-10 negatively correlated with FII, FV, FVII, FXI, and FXII, while TNF-α and IL-1 positively correlated with FVIII and FIX.
Conclusion
This study challenges the MUNW metric, revealing metabolic marker elevations in women without obesity. Additionally, MHO individuals exhibited pro-coagulant protein increases compared to MUO, suggesting limited clinical utility in categorizing the broader population with obesity. Our exploratory findings highlight how the interplay between metabolic health and body size phenotypes could challenge conventional frameworks for assessing health risk.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets analyzed during the current study are not publicly available due to ethical and institutional restrictions. However, they are available from the corresponding author upon request and with approval from the institutional ethics committee. No custom code was generated for this analysis.
References
Barquera S, Campos-Nonato I, Aguilar-Salinas C, Lopez-Ridaura R, Arredondo A, Rivera-Dommarco J. Diabetes in Mexico: cost and management of diabetes and its complications and challenges for health policy. Glob Health. 2013;9:3.
DiBonaventura MD, Meincke H, Le Lay A, Fournier J, Bakker E, Ehrenreich A. Obesity in Mexico: prevalence, comorbidities, associations with patient outcomes, and treatment experiences. Diabetes Metab Syndr Obes Targets Ther. 2017;ume 11:1–10.
April-Sanders AK, Rodriguez CJ. Metabolically healthy obesity redefined. JAMA Netw Open. 2021;4:e218860.
Mongraw-Chaffin M, Foster MC, Anderson CAM, Burke GL, Haq N, Kalyani RR, et al. Metabolically healthy obesity, transition to metabolic syndrome, and cardiovascular risk. J Am Coll Cardiol. 2018;71:1857–65.
Blüher M. Metabolically healthy obesity. Endocr Rev. 2020;41:bnaa004.
Beijers HJBH, Ferreira I, Spronk HMH, Bravenboer B, Dekker JM, Nijpels G, et al. Body composition as determinant of thrombin generation in plasma: the Hoorn study. Arterioscler Thromb Vasc Biol. 2010;30:2639–47.
Romano M, Guagnano MT, Pacini G, Vigneri S, Falco A, Marinopiccoli M, et al. Association of inflammation markers with impaired insulin sensitivity and coagulative activation in obese healthy women. J Clin Endocrinol Metab. 2003;88:5321–6.
Zheng H, Sechi LA, Navarese EP, Casu G, Vidili G. Metabolic dysfunction-associated steatotic liver disease and cardiovascular risk: a comprehensive review. Cardiovasc Diabetol. 2024;23:346.
Chandler WL, Rodgers GM, Sprouse JT, Thompson AR. Elevated hemostatic factor levels as potential risk factors for thrombosis. Arch Pathol Lab Med. 2002;126:1405–14.
Ding C, Chan Z, Magkos F. Lean, but not healthy: the ‘metabolically obese, normal-weight’ phenotype. Curr Opin Clin Nutr Metab Care. 2016;19:408–17.
Balcázar-Hernandez L, Basurto L, Manuel-Apolinar L, Vega-García S, Basurto-Acevedo N, Martínez-Murillo C, et al. Pattern of adiponectin, osteocalcin, irisin, FGF-21, and MCP-1 according to the body size phenotype: could they be markers of metabolic health in mexican-mestizo middle-aged women?. Metabolites. 2021;11:771.
Karelis AD, Rabasa-Lhoret R. Inclusion of C-reactive protein in the identification of metabolically healthy but obese (MHO) individuals. Diabetes Metab. 2008;34:183–4.
Li X, Wang X, Li H, Li Y, Guo Y. Seminal plasma lipidomics profiling to identify signatures of Kallmann syndrome. Front Endocrinol. 2021;12:692690.
Karelis A, Brochu M, Rabasa-Lhoret R. Can we identify metabolically healthy but obese individuals (MHO)?. Diabetes Metab. 2004;30:569–72.
Tanriover C, Copur S, Gaipov A, Ozlusen B, Akcan RE, Kuwabara M, et al. Metabolically healthy obesity: misleading phrase or healthy phenotype?. Eur J Intern Med. 2023;111:5–20.
Stefan N. Metabolically Healthy And Unhealthy Normal Weight And Obesity. Endocrinol Metab. 2020;35:487–93.
Mahamat-Saleh Y, Rinaldi S, Kaaks R, Biessy C, Gonzalez-Gil EM, Murphy N, et al. Metabolically defined body size and body shape phenotypes and risk of postmenopausal breast cancer in the European Prospective Investigation into Cancer and Nutrition. Cancer Med. 2023;12:12668–82.
Meloni A, Cadeddu C, Cugusi L, Donataccio MP, Deidda M, Sciomer S, et al. Gender differences and cardiometabolic risk: the importance of the risk factors. Int J Mol Sci. 2023;24:1588.
Tsalamandris S, Antonopoulos AS, Oikonomou E, Papamikroulis G-A, Vogiatzi G, Papaioannou S, et al. The role of inflammation in diabetes: current concepts and future perspectives. Eur Cardiol Rev. 2019;14:50–59.
Misra A, Gopalan H, Jayawardena R, Hills AP, Soares M, Reza-Albarrán AA, et al. Diabetes in developing countries. J Diabetes. 2019;11:522–39.
Abdesselam A, Zidoum H, Zadjali F, Hedjam R, Al-Ansari A, Bayoumi R, et al. Estimate of the HOMA-IR cut-off value identifying subjects at risk of insulin resistance using a machine learning approach. Sultan Qaboos Univ Med J SQUMJ. 2021;21:604–12.
Basurto L, Díaz A, Rodriguez A, Robledo A, Vega S, Garcia-Vega J, et al. Circulating levels of plasminogen activator inhibitor-1 are associated with metabolic syndrome rather than with menopause. Gynecol Endocrinol. 2019;35:909–12.
Lupattelli G, De Vuono S, Boni M, Helou R, Raffaele Mannarino M, Rita Roscini A, et al. Insulin resistance and not bmi is the major determinant of early vascular impairment in patients with morbid obesity. J Atheroscler Thromb. 2013;20:924–33.
Basurto L, Sánchez L, Díaz A, Valle M, Robledo A, Martínez-Murillo C. Differences between metabolically healthy and unhealthy obesity in PAI-1 level. Thromb Res. 2019;180:110–4.
Kim J, Montagnani M, Chandrasekran S, Quon MJ. Role of lipotoxicity in endothelial dysfunction. Heart Fail Clin. 2012;8:589–607.
Hadi HAR, Suwaidi JA. Endothelial dysfunction in diabetes mellitus. Vasc Health Risk Manag. 2007;3:853–76.
The Emerging Risk Factors Collaboration*. Major lipids, apolipoproteins, and risk of vascular disease. JAMA. 2009;302:1993.
Freiberg JJ. Nonfasting triglycerides and risk of ischemic stroke in the general population. JAMA. 2008;300:2142.
Nordestgaard BG, Benn M, Schnohr P, Tybjærg-Hansen A. Nonfasting triglycerides and risk of myocardial infarction, ischemic heart disease, and death in men and women. JAMA. 2007;298:299.
Essilfie G, Shavelle DM, Tun H, Platt K, Kobayashi R, Mehra A, et al. Association of elevated triglycerides and acute myocardial infarction in young Hispanics. Cardiovasc Revasc Med. 2016;17:510–4.
Medina-Leyte DJ, Zepeda-García O, Domínguez-Pérez M, González-Garrido A, Villarreal-Molina T, Jacobo-Albavera L. Endothelial dysfunction, inflammation and coronary artery disease: potential biomarkers and promising therapeutical approaches. Int J Mol Sci. 2021;22:3850.
Kim NH, Kim JH, Kim YJ, Yoo HJ, Kim HY, Seo JA, et al. Clinical and metabolic factors associated with development and regression of nonalcoholic fatty liver disease in nonobese subjects. Liver Int. 2014;34:604–11.
Theofilis P, Vordoni A, Nakas N, Kalaitzidis RG. Endothelial dysfunction in nonalcoholic fatty liver disease: a systematic review and meta-analysis. Life. 2022;12:718.
Zhang Y, Vittinghoff E, Pletcher MJ, Allen NB, Zeki Al Hazzouri A, Yaffe K, et al. Associations of blood pressure and cholesterol levels during young adulthood with later cardiovascular events. J Am Coll Cardiol. 2019;74:330–41.
Abdullah SM, Defina LF, Leonard D, Barlow CE, Radford NB, Willis BL, et al. Long-term association of low-density lipoprotein cholesterol with cardiovascular mortality in individuals at low 10-year risk of atherosclerotic cardiovascular disease: results from the cooper center longitudinal study. Circulation. 2018;138:2315–25.
Ference BA, Ginsberg HN, Graham I, Ray KK, Packard CJ, Bruckert E, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J. 2017;38:2459–72.
Kornblith LZ, Howard B, Kunitake R, Redick B, Nelson M, Cohen MJ, et al. Obesity and clotting: Body mass index independently contributes to hypercoagulability after injury. J Trauma Acute Care Surg. 2015;78:30–38.
Janac JM, Zeljkovic A, Jelic-Ivanovic ZD, Dimitrijevic-Sreckovic VS, Vekic J, Miljkovic MM, et al. Increased oxidized high-density lipoprotein/high-density lipoprotein–cholesterol ratio as a potential indicator of disturbed metabolic health in overweight and obese individuals. Lab Med. 2020;51:24–33.
Laczkovics C, Grafenhofer H, Kaider A, Quehenberger P, Simanek R, Mannhalter C, et al. Risk of recurrence after a first venous thromboembolic event in young women. Haematologica. 2007;92:1201–7.
Heit JA, Silverstein MD, Mohr DN, Petterson TM, Lohse CM, O’Fallon WM, et al. The epidemiology of venous thromboembolism in the community. Thromb Haemost. 2001;86:452–63.
Eichinger S. Overweight, obesity, and the risk of recurrent venous thromboembolism. Arch Intern Med. 2008;168:1678.
Folsom AR, Conlan MG, Davis CE, Wu KK. Relations between hemostasis variables and cardiovascular risk factors in middle-aged adults. Ann Epidemiol. 1992;2:481–94.
Reid HL, Vigilance J, Wright-Pascoe RA, Choo-Kang E. The influence of persistent hyperglycaemia on hyperfibrinogenaemia and hyperviscosity in diabetes mellitus. West Indian Med J. 2000;49:281–4.
Osende JI, Badimon JJ, Fuster V, Herson P, Rabito P, Vidhun R, et al. Blood thrombogenicity in type 2 diabetes mellitus patients is associated with glycemic control. J Am Coll Cardiol. 2001;38:1307–12.
Bruno G. Association of fibrinogen with glycemic control and albumin excretion rate in patients with non-insulin-dependent diabetes mellitus. Ann Intern Med. 1996;125:653.
Boden G, Vaidyula VR, Homko C, Cheung P, Rao AK. Circulating tissue factor procoagulant activity and thrombin generation in patients with type 2 diabetes: effects of insulin and glucose. J Clin Endocrinol Metab. 2007;92:4352–8.
Lemkes BA, Hermanides J, Devries JH, Holleman F, Meijers JCM, Hoekstra JBL. Hyperglycemia: a prothrombotic factor?. J Thromb Haemost. 2010;8:1663–9.
Domingueti CP, Dusse LMS, Carvalho MDG, De Sousa LP, Gomes KB, Fernandes AP. Diabetes mellitus: the linkage between oxidative stress, inflammation, hypercoagulability and vascular complications. J Diabetes Complic. 2016;30:738–45.
Nieuwdorp M, Van Haeften TW, Gouverneur MCLG, Mooij HL, Van Lieshout MHP, Levi M, et al. Loss of endothelial glycocalyx during acute hyperglycemia coincides with endothelial dysfunction and coagulation activation in vivo. Diabetes. 2006;55:480–6.
Bester J, Pretorius E. Effects of IL-1β, IL-6 and IL-8 on erythrocytes, platelets and clot viscoelasticity. Sci Rep. 2016;6:32188.
Ku D-H, Arkel Y, Paidas M, Lockwood C. Circulating levels of inflammatory cytokines (IL-1β and TNF-α), resistance to activated protein C, thrombin and fibrin generation in uncomplicated pregnancies. Thromb Haemost. 2003;90:1074–9.
Grignani G, Maiolo A. Cytokines and hemostasis. Haematologica. 2000;85:967–72.
Song JW, Song KS, Choi JR, Kim SY, Rhee J-H. Plasma level of IL-6 and its relationship to procoagulant and fibrinolytic markers in acute ischemic stroke. Yonsei Med J. 2006;47:201.
Ott LW, Resing KA, Sizemore AW, Heyen JW, Cocklin RR, Pedrick NM, et al. Tumor necrosis factor-α- and interleukin-1-induced cellular responses: coupling proteomic and genomic information. J Proteome Res. 2007;6:2176–85.
Hamad OA, Nilsson PH, Wouters D, Lambris JD, Ekdahl KN, Nilsson B. Complement component C3 binds to activated normal platelets without preceding proteolytic activation and promotes binding to complement receptor 1. J Immunol. 2010;184:2686–92.
Pajkrt D, van der Poll T, Levi M, Cutler DL, Affrime MB, van den Ende A, et al. Interleukin-10 inhibits activation of coagulation and fibrinolysis during human endotoxemia. Blood. 1997;89:2701–5.
Steen EH, Wang X, Balaji S, Butte MJ, Bollyky PL, Keswani SG. The role of the anti-inflammatory cytokine interleukin-10 in tissue fibrosis. Adv Wound Care. 2020;9:184–98.
Wang B, Zhuang R, Luo X, Yin L, Pang C, Feng T, et al. Prevalence of metabolically healthy obese and metabolically obese but normal weight in adults worldwide: a meta-analysis. Horm Metab Res. 2015;47:839–45.
Basto-Abreu A, López-Olmedo N, Rojas-Martínez R, Aguilar-Salinas CA, Moreno-Banda GL, Carnalla M, et al. Prevalencia de prediabetes y diabetes en México: Ensanut 2022. Salud Pública México. 2023;65:s163–s168.
Author information
Authors and Affiliations
Contributions
MM Valle: Data Collection, methodology, writing original draft preparation; A Robledo and S O’Leary: Data processing, writing original draft preparation; E Reyes, J Gaspar, C Martínez-Murillo: Writing—Reviewing and editing; E Rosales and Vega-García S: Methodology; L Basurto: Data collection, methodology, obtaining financing, data processing, project administration, writing original draft preparation.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was conducted in accordance with the Declaration of Helsinki and applicable institutional and national regulations. The protocol and consent materials were reviewed and approved by the Ethics and Research Committee of the Mexican Social Security Institute (IMSS). All participants were adults and only de-identified data were analyzed. The study involved minimal risk, and no clinical interventions were performed. No identifiable images or personal data are included in this manuscript.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Valle, M.M., Robledo, A., O’Leary, S. et al. Cardiovascular risk factors associated with BMI and metabolic health phenotypes based on measures of coagulation factors. Int J Obes 49, 2530–2537 (2025). https://doi.org/10.1038/s41366-025-01915-1
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41366-025-01915-1