Abstract
Background
Genetic predisposition to central adiposity is associated with metabolic dysfunction and obesity-related hypertension. This study investigated the association between genetic predisposition of general and central adiposity and systolic blood pressure (SBP) across body mass index (BMI) categories. Additionally, we explored whether, among females, the metabolic factors, triglyceride-to-HDL cholesterol (TG/HDL-C) ratio, glycated hemoglobin (HbA1c), and serum uric acid (SUA), modulate these relationships.
Methods
This cross-sectional study included 10,734 females from the Taiwan Biobank. Associations between polygenic score of body mass index (PGS-BMI), waist-circumference (PGS-WC), waist to hip ratio (PGS-WHR), waist to height ratio (PGS-WHtR) and SBP were assessed using multivariable generalized additive models (GAM). The strongest PGS was further examined for interaction and mediation effects with metabolic factors across BMI categories. Polygenic pathway analyses were also conducted to identify underlying biological mechanisms.
Results
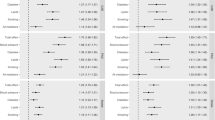
Among the four PGSs, PGS-WC showed the strongest association with SBP, particularly in females with normal weight (β = 0.026, 95% CI: 0.002–0.050; p_linear = 0.033; effective degree of freedom (edf) = 1.063; F = 3.201; p_smooth = 0.060) and overweight (β = –0.058, 95% CI: –0.095 to –0.021; p_linear = 0.002; edf = 2.272; F = 4.073; p_smooth = 0.006). The TG/HDL-C ratio significantly modulated this association across normal weight, overweight, and obesity categories in both interaction and mediation analyses. Polygenic pathway implicated biological processes including signal transduction, metabolism, immune regulation, and DNA repair.
Conclusion
These findings underscore the genetic influence of central adiposity on SBP regulation, particularly among females with normal weight and overweight. The TG/HDL-C ratio plays a key role in modulating this relationship, suggesting that metabolic risk-targeted interventions may enhance hypertension prevention and management in genetically susceptible populations.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The data that support the findings of this study are available from Taiwan Biobank, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are, however, available from the authors upon reasonable request and with permission from Taiwan Biobank. GWAS summary statistics for central adiposity had been submitted to the National Human Genome Research Institute—European Bioinformatics Institute (NHGRI-EBI) catalog with accession numbers GCST 90572795 for BMI, GCST 90572792 for WC, GSCT 90572793 for WHR, and GCST 90572794 for WHtR.
Code availability
The corresponding author (baich@tmu.edu.tw) will provide the codes used in this study upon request.
References
Bundy JD, Li C, Stuchlik P, Bu X, Kelly TN, Mills KT, et al. Systolic blood pressure reduction and risk of cardiovascular disease and mortality: a systematic review and network meta-analysis. JAMA Cardiol. 2017;2:775–81.
Ji H, Kim A, Ebinger JE, Niiranen TJ, Claggett BL, Bairey Merz CN, et al. Sex differences in blood pressure trajectories over the life course. JAMA Cardiol. 2020;5:19–26.
Cuspidi C, Gherbesi E, Sala C, Tadic M. Sex, gender, and subclinical hypertensiveorgan damage-heart. J Hum Hypertens. 2023;37:626–33.
Tadic M, Cuspidi C, Grassi G. The influence of sex on left ventricular remodeling in arterial hypertension. Heart Fail Rev. 2019;24:905–14.
Bruno RM, Varbiro S, Pucci G, Nemcsik J, Lonnebakken MT, Kublickiene K, et al. Vascular function in hypertension: does gender dimension matter? J Hum Hypertens. 2023;37:634–43.
Chuang SY, Chang HY, Tsai TY, Cheng HM, Pan WH, Chen CH. Isolated systolic hypertension and central blood pressure: implications from the national nutrition and health survey in Taiwan. J Clin Hypertens. 2021;23:656–64.
Chapman N, Ching SM, Konradi AO, Nuyt AM, Khan T, Twumasi-Ankrah B, et al. Arterial hypertension in women: state of the art and knowledge gaps. Hypertension. 2023;80:1140–9.
Reckelhoff JF. Mechanisms of sex and gender differences in hypertension. J Hum Hypertens. 2023;37:596–601.
Cornier MA, Despres JP, Davis N, Grossniklaus DA, Klein S, Lamarche B, et al. Assessing adiposity: a scientific statement from the American Heart Association. Circulation. 2011;124:1996–2019.
Chen J, Zuo H, Wu X, Zhang Y, Tan Q, Yu Z, et al. Diverse associations between adiposity and blood pressure among 80,000 multi-ethnic Chinese adults. BMC Public Health. 2023;23:298.
Gumilang RA, Fan YC, Wu SH, Bai CH. Adiposity indices and their higher predictive value for new-onset hypertension in metabolically healthy young women: findings from a population-based prospective cohort study. BMC Cardiovasc Disord. 2024;24:150.
Wong TJ, Yu T. Trends in the distribution of body mass index, waist circumference and prevalence of obesity among Taiwanese adults, 1993-2016. PLoS ONE. 2022;17:e0274134.
DeMarco VG, Aroor AR, Sowers JR. The pathophysiology of hypertension in patients with obesity. Nat Rev Endocrinol. 2014;10:364–76.
Shen L, Wang L, Hu Y, Liu T, Guo J, Shen Y, et al. Associations of the ages at menarche and menopause with blood pressure and hypertension among middle-aged and older Chinese women: a cross-sectional analysis of the baseline data of the China Health and Retirement Longitudinal Study. Hypertens Res. 2019;42:730–8.
Wu Z, Zhou D, Liu Y, Li Z, Wang J, Han Z, et al. Association of TyG index and TG/HDL-C ratio with arterial stiffness progression in a non-normotensive population. Cardiovasc Diabetol. 2021;20:134.
Bakhtiyari M, Schmidt N, Hadaegh F, Khalili D, Mansournia N, Asgari S, et al. Direct and indirect effects of central and general adiposity on cardiovascular diseases: the Tehran Lipid and Glucose Study. Eur J Prev Cardiol. 2018;25:1170–81.
Yao J, Zhang Y, Zhao J, Lin YP, Lu QY, Fan GJ. Correlation of obesity, dietary patterns, and blood pressure with uric acid: data from the NHANES 2017-2018. BMC Endocr Disord. 2022;22:196.
Wen W, Kato N, Hwang JY, Guo X, Tabara Y, Li H, et al. Genome-wide association studies in East Asians identify new loci for waist-hip ratio and waist circumference. Sci Rep. 2016;6:17958.
Sun C, Kovacs P, Guiu-Jurado E. Genetics of body fat distribution: comparative analyses in populations with European, Asian and African Ancestries. Genes (Basel) 2021;12:841.
Collister JA, Liu X, Clifton L. Calculating polygenic risk scores (PRS) in UK Biobank: a practical guide for epidemiologists. Front Genet. 2022;13:818574.
Johnson W, Norris T, Pearson N, Petherick ES, King JA, Willis SA, et al. Are associations of adulthood overweight and obesity with all-cause mortality, cardiovascular disease, and obesity-related cancer modified by comparative body weight at age 10 years in the UK Biobank study? Int J Obes. 2025;49:902–14.
Shi M, Chen W, Sun X, Bazzano LA, He J, Razavi AC, et al. Association of genome-wide polygenic risk score for body mass index with cardiometabolic health from childhood through midlife. Circ Genom Precis Med. 2022;15:e003375.
World Health Organization. Regional Office for the Western P. The Asia-Pacific perspective: redefining obesity and its treatment. Sydney: Health Communications Australia; 2000.
Wang TD, Chiang CE, Chao TH, Cheng HM, Wu YW, Wu YJ, et al. 2022 Guidelines of the Taiwan Society of Cardiology and the Taiwan Hypertension Society for the management of hypertension. Acta Cardiol Sin. 2022;38:225–325.
Choi SW, O’Reilly PF. PRSice-2: polygenic risk score software for biobank-scale data. Gigascience. 2019;8:giz082.
Liberzon A, Subramanian A, Pinchback R, Thorvaldsdottir H, Tamayo P, Mesirov JP. Molecular signatures database (MSigDB) 3.0. Bioinformatics. 2011;27:1739–40.
Cambia JM, Tsai JF, Daniele G, Lin SH, Chang YH, Yang CT, et al. Polygenic Mediation Analysis ofPsychological Resilience and Outcomes in Taiwanese Young Adults. J Genet Psychol. 2025; 1–19.
Alfons A, Ateş NY, Groenen PJF. A robust bootstrap test for mediation analysis. Organ Res Methods. 2021;25:591–617.
Saini S, Walia GK, Sachdeva MP, Gupta V. Genomics of body fat distribution. J Genet. 2021;100:32.
Choe EK, Shivakumar M, Lee SM, Verma A, Kim D. Dissecting the clinical relevance of polygenic risk score for obesity-a cross-sectional, longitudinal analysis. Int J Obes. 2022;46:1686–93.
Holmes MV, Pulit SL, Lindgren CM. Genetic and epigenetic studies of adiposity and cardiometabolic disease. Genome Med. 2017;9:82.
Tian T, Zhang J, Zhu Q, Xie W, Wang Y, Dai Y. Predicting value of five anthropometric measures in metabolic syndrome among Jiangsu Province, China. BMC Public Health. 2020;20:1317.
Zhang ZQ, Deng J, He LP, Ling WH, Su YX, Chen YM. Comparison of various anthropometric and body fat indices in identifying cardiometabolic disturbances in Chinese men and women. PLoS ONE. 2013;8:e70893.
Koenen M, Hill MA, Cohen P, Sowers JR. Obesity, adipose tissue and vascular dysfunction. Circ Res. 2021;128:951–68.
Sabbatini AR, Kararigas G. Estrogen-related mechanisms in sex differences of hypertension and target organ damage. Biol Sex Differ. 2020;11:31.
Wu YJ, Jiang CQ, Zhu T, Jin YL, Zhu F, Zhou BJ, et al. Obesity indicators as mediators of the association between age at menopause and blood pressure values. Hypertens Res. 2023;46:1100–9.
Zhang L, Li Y, Zhou W, Wang C, Dong X, Mao Z, et al. Mediation effect of BMI on the relationship between age at menarche and hypertension: the Henan Rural Cohort Study. J Hum Hypertens. 2020;34:448–56.
Baraskar K, Thakur P, Shrivastava R, Shrivastava VK. Female obesity: association with endocrine disruption and reproductive dysfunction. Obes Med. 2021;28:1003785.
Tzoulaki I, Elliott P, Kontis V, Ezzati M. Worldwide exposures to cardiovascular risk factors and associated health effects: current knowledge and data gaps. Circulation. 2016;133:2314–33.
Smith JA, Ware EB, Middha P, Beacher L, Kardia SL. Current applications of genetic risk scores to cardiovascular outcomes and subclinical phenotypes. Curr Epidemiol Rep. 2015;2:180–90.
Tatsumi Y, Nakao YM, Masuda I, Higashiyama A, Takegami M, Nishimura K, et al. Risk for metabolic diseases in normal weight individuals with visceral fat accumulation: a cross-sectional study in Japan. BMJ Open. 2017;7:e013831.
Lei L, Changfa W, Ting Y, Xiaoling Z, Yaqin W. Metabolically healthy transition and its association with body size change patterns among different adult age groups. Diab Res Clin Pr. 2022;192:110108.
Lui DTW, Ako J, Dalal J, Fong A, Fujino M, Horton A, et al. Obesity in the Asia-Pacific region: current perspectives. J Asian Pac Soc Cardiol. 2024;3:e21.
Taiwan Medical Association for the Study of Obesity. Evidence-based guideline on adult obesity prevention and management [Internet]. Taipei: Taiwan Medical Association for the Study of Obesity; 2023 [cited 2024 Dec 19]. Available from: https://www.hpa.gov.tw/File/Attach/10042/File_20342.pdf.
Busetto L, Dicker D, Frühbeck G, Halford JCG, Sbraccia P, Yumuk V, et al. A new framework for the diagnosis, staging and management of obesity in adults. Nat Med. 2024;30:2395–9.
Yuge H, Okada H, Hamaguchi M, Kurogi K, Murata H, Ito M, et al. Triglycerides/HDL cholesterol ratio and type 2 diabetes incidence: Panasonic Cohort Study 10. Cardiovasc Diabetol. 2023;22:308.
Han Y, Han X, Yin Y, Cao Y, Di H, Wu J, et al. Dose-response relationship of uric acid with fasting glucose, insulin, and insulin resistance in a United States cohort of 5,148 non-diabetic people. Front Med. 2022;9:905085.
Kawai T, Autieri MV, Scalia R. Adipose tissue inflammation and metabolic dysfunction in obesity. Am J Physiol Cell Physiol. 2021;320:C375–91.
Wang Y, Zhao X, Chen Y, Yao Y, Zhang Y, Wang N, et al. Visceral adiposity measures are strongly associated with cardiovascular disease among female participants in Southwest China: a population-based prospective study. Front Endocrinol. 2022;13:969753.
Luan D, Dadpey B, Zaid J, Bridge-Comer PE, DeLuca JH, Xia W, et al. Adipocyte-secreted IL-6 sensitizes macrophages to IL-4 signaling. Diabetes. 2023;72:367–74.
Rajapakse Niwanthi W, Giam B, Kuruppu S, Head Geoffrey A, Kaye David M. Impaired l-arginine-nitric oxide pathway contributes to the pathogenesis of resistant hypertension. Clin Sci. 2019;133:2061–7.
Zheng G, Jin J, Wang F, Zheng Q, Shao J, Yao J, et al. Association between atherogenic index of plasma and future risk of cardiovascular disease in individuals with cardiovascular-kidney-metabolic syndrome stages 0–3: a nationwide prospective cohort study. Cardiovasc Diabetol. 2025;24:22.
Lee SH, Park SY, Choi CS. Insulin resistance: from mechanisms to therapeutic strategies. Diab Metab J. 2022;46:15–37.
Fu L, Li Y, Cheng H, Xiong J, Xiao P, Dong H, et al. Role of inflammatory biomarkers in mediating causal effect of life course body composition on hypertension. Hypertens. 2025;82.
Acknowledgements
The authors express their sincere gratitude to Yen-Chun Fan (Department of Allied Health Education and Digital Learning, College of Nursing, National Taipei University of Nursing and Health Sciences) and Shang-Hao Wu (College of Public Health, Taipei Medical University) for their valuable contributions to this study. This research was supported by the National Science and Technology Council of Taiwan through Grant NSTC 113-2314-B-038-080-MY3.
Author information
Authors and Affiliations
Contributions
RAG contributed to the study design and methodology development, data analysis and interpretation of the results and wrote and approved the manuscript. CHB constructed the study design and analytical concept, obtained funding, and analyzed, critically revised, and approved the manuscript. All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Ethical clearance for this study was granted by the Institutional Board Review of Taipei Medical University, with the approval number N202104112. All individuals participating in the Taiwan Biobank provided informed consent before enrolling in the study. Data were retrieved and analyzed in accordance with Taiwan Biobank data safety regulations. This study was conducted in compliance with the STrengthening the REporting of Genetic Association Studies (STREGA) guidelines (see STREGA checklist in the Supplementary Materials).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gumilang, R.A., Bai, CH. Genetic impact of central adiposity on systolic blood pressure in females: interaction and mediation by TG/HDL-C, HbA1c, and uric acid across BMI categories. Int J Obes 49, 2521–2529 (2025). https://doi.org/10.1038/s41366-025-01917-z
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41366-025-01917-z