Abstract
Background
As climate change raises global temperatures, there remains a notable gap in understanding the body’s mechanisms of heat stress defense exhibited by Heat Shock Protein (HSP) within the populations.
Objective
This study aims to investigate the expression level of HSP70 in response to indoor heat exposure among vulnerable populations in both urban and rural settings.
Methods
A comparative cross-sectional was conducted among 108 participants from urban and rural areas in Klang Valley, Malaysia. The study included face-to-face interviews, indoor heat exposure monitoring, and thermal stress classification using the Universal Thermal Climate Index (UTCI). HSP70 gene and protein expressions were analyzed using reverse-transcription quantitative polymerase chain reaction (RT-qPCR) and HSP70 High Sensitivity Enzyme-linked Immunosorbent Assay (ELISA), respectively.
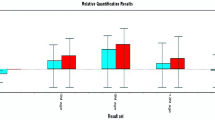
Results
Urban areas experienced signficantly higher UTCI heat exposure levels than rural areas (p < 0.001). In response to heat stress, vulnerable populations in urban areas exhibited higher HSP70 gene relative expression and HSP70 protein expression. A significant mean difference in the plasma HSP70 protein expression was observed between the two groups (p < 0.001). The linear mixed model (LMM) revealed a significant association between UTCI heat exposure levels and HSP70 gene and protein expression in both groups (p < 0.001).
Impact
-
While previous studies have examined cellular responses to heat stress in healthy individuals within controlled experimental settings, our study uniquely focuses on vulnerable individuals in actual environmental conditions. This is crucial for establishing baseline information on the ability of these populations to adapt to climate change and surrounding temperatures. Such information is essential for building resilient communities and preventing fatal incidents such as heat stroke during extreme heat events. By highlighting the differences between urban and rural populations, this study provides critical information for policymakers and health practitioners to design location-specific and population-specific heat stress mitigation strategies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Muhammad MKI, Hamed MM, Harun S, Sa’adi Z, Sammen SS, Al Ansari N, et al. Heatwaves in Peninsular Malaysia: a spatiotemporal analysis. Sci Rep. 2024;14:4255. https://doi.org/10.1038/s41598-024-53960-x
Suparta W, Yatim ANM. Characterization of heat waves: a case study for Peninsular Malaysia. Geographia Technica. 2019;14:146–55. https://doi.org/10.21163/GT_2019.141.11
Tang KHD. Climate change in Malaysia: Trends, contributors, impacts, mitigation, and adaptations. Sci Total Environ. 2019;650:1858–71. https://doi.org/10.1016/j.scitotenv.2018.09.316
Yatim ANM, Latif MT, Ahamad F, Khan MF, Nadzir MSM, Juneng L. Observed Trends in Extreme Temperature over the Klang Valley, Malaysia. Adv Atmos Sci. 2019;36:1355–70. https://doi.org/10.1007/s00376-019-9075-0
Deng Q, Zhao J, Liu W, Li Y. Heatstroke at home: prediction by thermoregulation modeling. Build Environ. 2018;137:147–56. https://doi.org/10.1016/j.buildenv.2018.04.017
Centers for Disease Control and Prevention (CDC). Protecting vulnerable groups from extreme heat. Centers for Disease Control and Prevention; 2017. https://www.cdc.gov/disasters/extremeheat/specificgroups.html. Accessed March 2023.
Morris KI, Chan A, Morris KJK, Ooi MCG, Oozeer MY, Abakr YA, et al. Urbanisation and urban climate of a tropical conurbation, Klang Valley, Malaysia. Urban Climate. 2017;19:54–71. https://doi.org/10.1016/j.uclim.2016.12.002
Zander KK, Mathew S. Estimating economic losses from perceived heat stress in urban Malaysia. Ecol Econ. 2019;159:84–90. https://doi.org/10.1016/j.ecolecon.2019.01.023
Department of Occupational, Safety and Health Malaysia (DOSH). Guideline on heat stress management at workplace. Department of Occupational, Safety and Health, Malaysia; 2016. https://www.dosh.gov.my/index.php/legislation/guidelines/industrial-hygiene-1/2017-guidelines-heat-stress-management-at-workplace/file. Accessed May 2023.
Ponomarenko M, Stepanenko I, Kolchanov N. Heat shock proteins. In: Brenner’s encyclopedia of genetics; 2013. p. 402–5 https://doi.org/10.1016/b978-0-12-374984-0.00685-9
Radons J. The human HSP70 family of chaperones: where do we stand? Cell Stress Chaperones. 2016;21:379–404. https://doi.org/10.1007/s12192-016-0676-6
Sharma D, Masison DC. Hsp70 structure, function, regulation, and influence on yeast prions. Protein Pept Lett. 2009;16:571–81. https://doi.org/10.2174/092986609788490230
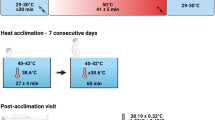
Nava R, Zuhl MN. Heat acclimation-induced intracellular HSP70 in humans: a meta-analysis. Cell Stress Chaperones. 2020;25:35–45. https://doi.org/10.1007/s12192-019-01059-y
Zurawlew MJ, Walsh NP, Fortes MB, Potter C. Post-exercise hot water immersion induces heat acclimation and improves endurance exercise performance in the heat. Scand J Med Sci Sports. 2016;26:745–54. https://doi.org/10.1111/sms.12638
Miller DJ, Fort PE. Heat shock proteins regulatory role in neurodevelopment. Front Neurosci. 2018;12:821 https://doi.org/10.3389/fnins.2018.00821
Rout PK, Kaushik R, Ramachandran N. Differential expression pattern of heat shock protein 70 gene in tissues and heat stress phenotypes in goats during peak heat stress period. Cell Stress Chaperones. 2016;21:645–51. https://doi.org/10.1007/s12192-016-0689-1
Iba T, Helms J, Levi M, Levy JH. Inflammation, coagulation, and cellular injury in heat-induced shock. Inflamm Res. 2023;72:463–73. https://doi.org/10.1007/s00011-022-01687-8
Iba T, Connors JM, Levi M, Levy JH. Heatstroke-induced coagulopathy: Biomarkers, mechanistic insights, and patient management. E Clin Med. 2022;44:101276 https://doi.org/10.1016/j.eclinm.2022.101276
Ou Y, Wang F, Zhao J, Deng Q. Risk of heatstroke in healthy elderly during heatwaves: A thermoregulatory modeling study. Build Environ. 2023;237:110324 https://doi.org/10.1016/j.buildenv.2023.110324
Nayak SG, Shrestha S, Kinney PL, Ross Z, Sheridan SC, Pantea CI, et al. Development of a heat vulnerability index for New York State. Public Health. 2018;161:127–37. https://doi.org/10.1016/j.puhe.2017.09.006
Min JY, Lee HS, Choi YS, Min KB. Association between income levels and prevalence of heat- and cold-related illnesses in Korean adults. BMC Public Health. 2021;21:1264 https://doi.org/10.1186/s12889-021-11227-4
Peng B, Williams S, Loughnan M, Lloyd G, Hansen A, Kjellstrom T, et al. The effects of extreme heat on human mortality and morbidity in Australia: implications for public health. Asia Pac J Public Health. 2011;23:27–36. https://doi.org/10.1177/1010539510391644
Muhamad SN, How V, Lim FL, Akim AM, Karuppiah K, Shabri NSAM. Assessment of heat stress contributing factors in the indoor environment among vulnerable populations in Klang Valley using principal component analysis (PCA). Sci Rep. 2024;14:24013 https://doi.org/10.1038/s41598-024-75132-7. Published 2024 Oct 14
Campbell HA, Akerman AP, Kissling LS, et al. Acute physiological and psychophysical responses to different modes of heat stress. Exp Physiol. 2022;107:429–40. https://doi.org/10.1113/EP089992
Malaysian Meteorological Department (MetMalaysia). Southwest monsoon report: Kuala Lumpur monsoon activity centre. Ministry of Natural Resources, Environment and Climate Change. 2023. https://www.met.gov.my/data/research/KLMAC_SW.pdf. Accessed Nov 2024.
ISO 7243. Hot environments—Estimation of the heat stress on working man, based on the WBGT-index (wet bulb globe temperature). 1989. https://www.iso.org/standard/13895.html.
Nurhartonosuro IM, Mohd Tamrin SB, Mohd Suadi Nata DH, Karuppiah K, Ng YG. Comparison of indices to estimate heat exposure to human: a review in tropical regions. Malays J Med Health Sci. 2022;18:303–15. ISSN 2636-9346
Blazejczyk K, Broede P, Fiala D, Havenith G, Holmer I, Jendritzky G, et al. Principles of the new Universal Thermal Climate Index (UTCI) and its application to bioclimatic research in European scale. Misc Geogr. 2010;14:91–102. https://doi.org/10.2478/mgrsd-2010-0009
Qiagen. QIAamp RNA Blood Mini Kit Handbook. 2021. https://www.qiagen.com/us/products/discovery-and-translational-research/dna-rna-purification/rna-purification/total-rna/qiaamp-rna-blood-mini-kit.
Srivastava K, Narang R, Bhatia J, Saluja D. Expression of heat shock protein 70 gene and its correlation with inflammatory markers in essential hypertension. PLoS ONE. 2016;11:e0151060 https://doi.org/10.1371/journal.pone.0151060
Bustin SA. Absolute quantification of mRNA using real-time reverse transcription polymerase chain reaction assays. J Mol Endocrinol. 2000;25:169–93. https://doi.org/10.1677/jme.0.0250169
Tukaj S, Mantej J, Sobala M, Potrykus K, Sitko K. Autologous extracellular Hsp70 exerts a dual role in rheumatoid arthritis. Cell Stress Chaperones. 2020;25:1105–10. https://doi.org/10.1007/s12192-020-01114-z
Abcam. HSP70 High Sensitivity ELISA Kit (ab133061) Protocol. 2019. https://www.abcam.com/products/elisa/hsp70-high-sensitivity-elisa-kit-ab133061.html
Kyriazos T, Poga M. Dealing with multicollinearity in factor analysis: the problem, detections, and solutions. Open J Stat. 2023;13:404–24. https://doi.org/10.4236/ojs.2023.133020
Almalki AFY, Arabdin M, Khan A. The role of heat shock proteins in cellular homeostasis and cell survival. Cureus. 2021;13:e18316 https://doi.org/10.7759/cureus.18316
Alharbi BM, Albinhassan TH, Alzahrani RA, Bouchama A, Mohammad S, Alomari AA, et al. Profiling the Hsp70 chaperone network in heat-induced proteotoxic stress models of human neurons. Biology. 2023;12:416 https://doi.org/10.3390/biology12030416
Gibson OR, Mee JA, Tuttle JA, Taylor L, Watt PW, Maxwell NS. Isothermic and fixed-intensity heat acclimation methods induce similar heat adaptation following short and long-term timescales. J Therm Biol. 2015;49-50:55–65. https://doi.org/10.1016/j.jtherbio.2015.02.005
Lee BJ, Mackenzie RW, Cox V, James RS, Thake CD. Human Monocyte heat shock protein 72 responses to acute hypoxic exercise after 3 days of exercise heat acclimation. Biomed Res Int. 2015;2015:849809 https://doi.org/10.1155/2015/849809
Zheng X, Krakowiak J, Patel N, Beyzavi A, Ezike J, Khalil A, et al. Dynamic control of Hsf1 during heat shock by a chaperone switch and phosphorylation. eLife. 2016;5:e18638 https://doi.org/10.7554/eLife.18638
Krakowiak J, Zheng X, Patel N, Feder ZA, Anandhakumar J, Valerius K, et al. Hsf1 and Hsp70 constitute a two-component feedback loop that regulates the yeast heat shock response. eLife. 2018;7:e31668 https://doi.org/10.7554/eLife.31668
Lee BJ, Sukri NM, Ogden H, Vine C, Thake CD, Turner JE, et al. A comparison of two commercially available ELISA methods for the quantification of human plasma heat shock protein 70 during rest and exercise stress. Cell Stress Chaperones. 2015;20:917–26. https://doi.org/10.1007/s12192-015-0610-3
Gibson OR, Taylor L, Watt PW, Maxwell NS. Heat acclimation attenuates physiological strain and the HSP72, but not HSP90, mRNA response to acute normobaric hypoxia. J Appl Physiol. 2015;119:889–99. https://doi.org/10.1152/japplphysiol.00332.2015
Lee BJ, Miller A, James RS, Thake CD. Cross acclimation between heat and hypoxia: heat acclimation improves cellular tolerance and exercise performance in acute normobaric hypoxia. Front Physiol. 2016;7:78 https://doi.org/10.3389/fphys.2016.00078
Heathcote SL, Hassmen P, Zhou S, Stevens CJ. Passive heating: reviewing practical heat acclimation strategies for endurance athletes. Front Physiol. 2018;9:1851 https://doi.org/10.3389/fphys.2018.01851
Dokladny K, Myers OB, Moseley PL. Heat shock response and autophagy—cooperation and control. Autophagy. 2015;11:200–13. https://doi.org/10.1080/15548627.2015.1009776
Gibson OR, Taylor L, Watt PW, Maxwell NS. Cross-adaptation: heat and cold adaptation to improve physiological and cellular responses to hypoxia. Sports Med. 2017;47:1751–68. https://doi.org/10.1007/s40279-017-0717-z
Bouchama A, Rashid M, Malik SS, Mahri SA, Yassin Y, Abdullah M, et al. Whole genome transcriptomic reveals heat stroke molecular signatures in humans. J Physiol. 2023;601:2407–23. https://doi.org/10.1113/JP284031
Williams AA, Spengler JD, Catalano P, Allen JG, Cedeno-Laurent JG. Building vulnerability in a changing climate: indoor temperature exposures and health outcomes in older adults living in public housing during an extreme heat event in Cambridge, MA. Int J Environ Res Public Health. 2019;16:2373 https://doi.org/10.3390/ijerph16132373
Foster J, Hodder SG, Lloyd AB, Havenith G. Individual responses to heat stress: implications for hyperthermia and physical work capacity. Front Physiol. 2020;11:541483 https://doi.org/10.3389/fphys.2020.541483
Butler-Dawson J, Johnson RJ, Krisher L, Jaramillo D, Cruz A, Pilloni D, et al. A longitudinal assessment of heat exposure and biomarkers of kidney function on heat shock protein 70 and antibodies among agricultural workers. BMC Nephrol. 2024;25:277.
Acknowledgements
The authors thank Mrs. Amrina Mohd Amin and Mrs. Safarina Mohamad Ismuddin for their assistance during the field sampling and laboratory work.
Funding
This work was funded by the Ministry of Higher Education (Malaysia), under the Fundamental Research Grant Scheme (FRGS), (FRGS/1/2020/SKK06/UPM/02/1).
Author information
Authors and Affiliations
Contributions
SNM prepared the original draft of the manuscript. VH administered the project and designed the experiments. SNM and NSAMS involved in data collection, methodology, data extraction and data analysis. The manuscript was supervised, reviewed and edited by VH, AMA, FLL, and KK. All authors approved the final version of this manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
This study obtained ethical clearance from Ethics Committee for Research Involving Human Subjects of Universiti Putra Malaysia (UPM) (Ref. No.: JKEUPM-2022-222). Written consent was obtained from participants and parents or guardians for minors before proceeding with the data and samples collection. All data collection methods were performed in accordance with the respective ethical guidelines.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Muhamad, S.N., Md Akim, A., Lim, F.L. et al. Heat stress-induced heat shock protein 70 (HSP70) expressions among vulnerable populations in urban and rural areas Klang Valley, Malaysia. J Expo Sci Environ Epidemiol 35, 839–847 (2025). https://doi.org/10.1038/s41370-025-00764-4
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41370-025-00764-4