Abstract
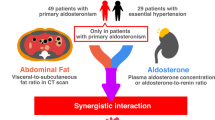
Primary aldosteronism (PA) is a common cause of secondary hypertension and is associated with worse cardiovascular outcomes. The elevated aldosterone in PA leads to left ventricular (LV) remodeling and dysfunction. In recent decades, clinical studies have demonstrated worse LV remodeling including increased LV mass and cardiac fibrosis in patients with PA compared to patients with essential hypertension. Several mechanisms may explain the process of aldosterone-induced LV remodeling, including directly profibrotic and hypertrophic effects of aldosterone on myocardium, increased reactive oxygen species and profibrotic molecules, dysregulation of extracellular matrix metabolism, endothelium dysfunction and circulatory macrophages activation. LV remodeling causes LV diastolic and systolic dysfunction, which may consequently lead to clinical complications such as heart failure, atrial fibrillation, ischemic heart disease, and other vascular events. Adequate treatment with adrenalectomy or medical therapy can improve LV remodeling and dysfunction in PA patients. In this review, we discuss the mechanisms of aldosterone-induced LV remodeling and provide an up-to-date review of clinical research about LV remodeling-related heart structural changes, cardiac dysfunction, and their clinical impacts on patients with PA.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Rossi GP. Prevalence and diagnosis of primary aldosteronism. Curr Hypertens Rep. 2010;12:342–8.
Milliez P, Girerd X, Plouin PF, Blacher J, Safar ME, Mourad JJ. Evidence for an increased rate of cardiovascular events in patients with primary aldosteronism. J Am Coll Cardiol. 2005;45:1243–8.
Catena C, Colussi G, Nadalini E, Chiuch A, Baroselli S, Lapenna R, et al. Cardiovascular outcomes in patients with primary aldosteronism after treatment. Arch Intern Med. 2008;168:80–5.
Reincke M, Fischer E, Gerum S, Merkle K, Schulz S, Pallauf A, et al. Observational study mortality in treated primary aldosteronism: the German Conn’s registry. Hypertension (Dallas, Tex: 1979). 2012;60:618–24.
Savard S, Amar L, Plouin PF, Steichen O. Cardiovascular complications associated with primary aldosteronism: a controlled cross-sectional study. Hypertension (Dallas, Tex: 1979). 2013;62:331–6.
Mulatero P, Monticone S, Bertello C, Viola A, Tizzani D, Iannaccone A, et al. Long-term cardio- and cerebrovascular events in patients with primary aldosteronism. J Clin Endocrinol Metab. 2013;98:4826–33.
Monticone S, D’Ascenzo F, Moretti C, Williams TA, Veglio F, Gaita F, et al. Cardiovascular events and target organ damage in primary aldosteronism compared with essential hypertension: a systematic review and meta-analysis. The lancet. Lancet Diabet Endocrinol. 2018;6:41–50.
Wu VC, Wang SM, Chang CH, Hu YH, Lin LY, Lin YH, et al. Long term outcome of Aldosteronism after target treatments. Sci Rep. 2016;6:32103.
Chen ZW, Huang KC, Lee JK, Lin LC, Chen CW, Chang YY, et al. Aldosterone induces left ventricular subclinical systolic dysfunction: a strain imaging study. J Hypertens. 2018;36:353–60.
Lin Y-H, Lin L-Y, Chen A, Wu X-M, Lee J-K, Su T-C, et al. Adrenalectomy improves increased carotid intima-media thickness and arterial stiffness in patients with aldosterone producing adenoma. Atherosclerosis. 2012;221:154–9.
Liao CW, Lin LY, Hung CS, Lin YT, Chang YY, Wang SM, et al. Time course and factors predicting arterial stiffness reversal in patients with aldosterone-producing adenoma after adrenalectomy: prospective study of 102 patients. Sci Rep. 2016;6:20862.
Rossi GP, Sacchetto A, Visentin P, Canali C, Graniero GR, Palatini P, et al. Changes in left ventricular anatomy and function in hypertension and primary aldosteronism. Hypertension. 1996;27:1039–45.
Rossi GP, Sacchetto A, Pavan E, Palatini P, Graniero GR, Canali C, et al. Remodeling of the left ventricle in primary aldosteronism due to Conn’s adenoma. Circulation. 1997;95:1471–8.
Matsumura K, Fujii K, Oniki H, Oka M, Iida M. Role of aldosterone in left ventricular hypertrophy in hypertension. Am J Hypertens. 2006;19:13–8.
Tanabe A, Naruse M, Naruse K, Hase M, Yoshimoto T, Tanaka M, et al. Left ventricular hypertrophy is more prominent in patients with primary aldosteronism than in patients with other types of secondary hypertension. Hypertension Res. 1997;20:85–90.
Rossi GP, Di Bello V, Ganzaroli C, Sacchetto A, Cesari M, Bertini A, et al. Excess ldosterone Is Associated with Alterations of Myocardial Texture in Primary Aldosteronism. Hypertension. 2002;40:23–27.
Kozakova M, Buralli S, Palombo C, Bernini G, Moretti A, Favilla S, et al. Myocardial ultrasonic backscatter in hypertension: relation to aldosterone and endothelin. Hypertension (Dallas, Tex: 1979). 2003;41:230–6.
Cohn JN, Ferrari R, Sharpe N. Cardiac remodeling-concepts and clinical implications: a consensus paper from an international forum on cardiac remodeling. Behalf of an International Forum on Cardiac Remodeling. J Am Coll Cardiol. 2000;35:569–82.
Azevedo PS, Polegato BF, Minicucci MF, Paiva SA, Zornoff LA. Cardiac remodeling: concepts, clinical impact, pathophysiological mechanisms and pharmacologic treatment. Arquivos Brasileiros de Cardiologia. 2016;106:62–9.
González A, Ravassa S, López B, Moreno MU, Beaumont J, José GS, et al. Myocardial Remodeling in Hypertension. Hypertension (Dallas, Tex: 1979). 2018;72:549–58.
Sutton MG, Sharpe N. Left ventricular remodeling after myocardial infarction: pathophysiology and therapy. Circulation. 2000;101:2981–8.
Brilla CG, Pick R, Tan LB, Janicki JS, Weber KT. Remodeling of the rat right and left ventricles in experimental hypertension. Circulation Res. 1990;67:1355–64.
Brilla CG, Weber KT. Reactive and reparative myocardial fibrosis in arterial hypertension in the rat. Cardiovasc Res. 1992;26:671–7.
Brilla CG, Weber KT. Mineralocorticoid excess, dietary sodium, and myocardial fibrosis. J Lab Clin Med. 1992;120:893–901.
Catena C, Colussi G, Novello M, Verheyen ND, Bertin N, Pilz S, et al. Dietary salt intake is a determinant of cardiac changes after treatment of primary aldosteronism: a prospective study. Hypertension. 2016;68:204–12.
Pimenta E, Gordon RD, Stowasser M. Salt, aldosterone and hypertension. J Hum Hypertens. 2013;27:1–6.
Okoshi MP, Yan X, Okoshi K, Nakayama M, Schuldt AJ, O’Connell TD, et al. Aldosterone directly stimulates cardiac myocyte hypertrophy. J Card Fail. 2004;10:511–8.
Gros R, Ding Q, Armstrong S, O’Neil C, Pickering JG, Feldman RD. Rapid effects of aldosterone on clonal human vascular smooth muscle cells. Am J Physiol Cell Physiol. 2007;292:C788–94.
Lopez N, Diez J, Fortuno MA. Differential hypertrophic effects of cardiotrophin-1 on adult cardiomyocytes from normotensive and spontaneously hypertensive rats. J Mol Cell Cardiol. 2006;41:902–13.
Lopez-Andres N, Martin-Fernandez B, Rossignol P, Zannad F, Lahera V, Fortuno MA, et al. A role for cardiotrophin-1 in myocardial remodeling induced by aldosterone. Am J Physiol Heart Circ Physiol. 2011;301:H2372–82.
Weber KT, Brilla CG. Pathological hypertrophy and cardiac interstitium. Fibros Renin-Angiotensin-Aldosterone Syst Circ. 1991;83:1849–65.
Lacolley P, Labat C, Pujol A, Delcayre C, Benetos A, Safar M. Increased carotid wall elastic modulus and fibronectin in aldosterone-salt-treated rats: effects of eplerenone. Circulation. 2002;106:2848–53.
Greene EL, Kren S, Hostetter TH. Role of aldosterone in the remnant kidney model in the rat. J Clin Investig. 1996;98:1063–8.
Sun Y, Zhang J, Lu L, Chen SS, Quinn MT, Weber KT. Aldosterone-induced inflammation in the rat heart: role of oxidative stress. Am J Pathol. 2002;161:1773–81.
Park YM, Park MY, Suh YL, Park JB. NAD(P)H oxidase inhibitor prevents blood pressure elevation and cardiovascular hypertrophy in aldosterone-infused rats. Biochem Biophys Res Commun. 2004;313:812–7.
Chou CH, Hung CS, Liao CW, Wei LH, Chen CW, Shun CT, et al. IL-6 trans-signalling contributes to aldosterone-induced cardiac fibrosis. Cardiovasc Res. 2018;114:690–702.
Brown NJ. Aldosterone and vascular inflammation. Hypertension. 2008;51:161–7.
Leopold JA, Dam A, Maron BA, Scribner AW, Liao R, Handy DE, et al. Aldosterone impairs vascular reactivity by decreasing glucose-6-phosphate dehydrogenase activity. Nat Med. 2007;13:189–97.
Liao CW, Lin YT, Wu XM, Chang YY, Hung CS, Wu VC, et al. The relation among aldosterone, galectin-3, and myocardial fibrosis: a prospective clinical pilot follow-up study. J Investig Med. 2016;64:1109–13.
Fiebeler A, Schmidt F, Muller DN, Park JK, Dechend R, Bieringer M, et al. Mineralocorticoid receptor affects AP-1 and nuclear factor-kappab activation in angiotensin II-induced cardiac injury. Hypertension. 2001;37:787–93.
Lother A, Berger S, Gilsbach R, Rosner S, Ecke A, Barreto F, et al. Ablation of mineralocorticoid receptors in myocytes but not in fibroblasts preserves cardiac function. Hypertension. 2011;57:746–54.
Bienvenu LA, Morgan J, Rickard AJ, Tesch GH, Cranston GA, Fletcher EK, et al. Macrophage mineralocorticoid receptor signaling plays a key role in aldosterone-independent cardiac fibrosis. Endocrinology. 2012;153:3416–25.
Caprio M, Newfell BG, la Sala A, Baur W, Fabbri A, Rosano G, et al. Functional mineralocorticoid receptors in human vascular endothelial cells regulate intercellular adhesion molecule-1 expression and promote leukocyte adhesion. Circ Res. 2008;102:1359–67.
Brown NJ. Contribution of aldosterone to cardiovascular and renal inflammation and fibrosis. Nat Rev Nephrol. 2013;9:459–69.
Calvier L, Miana M, Reboul P, Cachofeiro V, Martinez-Martinez E, de Boer RA, et al. Galectin-3 mediates aldosterone-induced vascular fibrosis. Arterioscler Thromb Vasc Biol. 2013;33:67–75.
Liao CW, Chou CH, Wu XM, Chen ZW, Chen YH, Chang YY, et al. Interleukin-6 plays a critical role in aldosterone-induced macrophage recruitment and infiltration in the myocardium. Biochim Biophys Acta Mol Basis Dis. 2020;1866:165627.
Brilla CG, Zhou G, Matsubara L, Weber KT. Collagen metabolism in cultured adult rat cardiac fibroblasts: response to angiotensin II and aldosterone. J Mol Cell Cardiol. 1994;26:809–20.
Somanna NK, Yariswamy M, Garagliano JM, Siebenlist U, Mummidi S, Valente AJ, et al. Aldosterone-induced cardiomyocyte growth, and fibroblast migration and proliferation are mediated by TRAF3IP2. Cell Signal. 2015;27:1928–38.
Rude MK, Duhaney TA, Kuster GM, Judge S, Heo J, Colucci WS, et al. Aldosterone stimulates matrix metalloproteinases and reactive oxygen species in adult rat ventricular cardiomyocytes. Hypertension. 2005;46:555–61.
Hung CS, Chou CH, Liao CW, Lin YT, Wu XM, Chang YY, et al. Aldosterone induces tissue inhibitor of Metalloproteinases-1 expression and further contributes to collagen accumulation: from clinical to bench studies. Hypertension. 2016;67:1309–20.
Arlt W, Lang K, Sitch AJ, Dietz AS, Rhayem Y, Bancos I, et al. Steroid metabolome analysis reveals prevalent glucocorticoid excess in primary aldosteronism. JCI Insight. 2017;2:e93136.
van Uum SH, Hermus AR, Smits P, Thien T, Lenders JW. The role of 11β-hydroxysteroid dehydrogenase in the pathogenesis of hypertension. Cardiovasc Res. 1998;38:16–24.
Funder JW. Aldosterone and mineralocorticoid receptors-physiology and pathophysiology. Int J Mol Sci. 2017;18:1032.
Slight S, Ganjam VK, Weber KT. Species diversity of 11β-hydroxysteroid dehydrogenase in the cardiovascular system. J Lab Clin Med. 1994;124:821–6.
Mihailidou AS, Loan LeTY, Mardini M, Funder JW. Glucocorticoids activate cardiac mineralocorticoid receptors during experimental myocardial infarction. Hypertension. 2009;54:1306–12.
McQUARRIE EP, Freel EM, Mark PB, Fraser R, Patel RK, Dargie HG, et al. Urinary corticosteroid excretion predicts left ventricular mass and proteinuria in chronic kidney disease. Clin Sci. 2012;123:285–94.
Adolf C, Kohler A, Franke A, Lang K, Riester A, Low A, et al. Cortisol Excess in Patients With Primary Aldosteronism Impacts Left Ventricular Hypertrophy. J Clin Endocrinol Metab. 2018;103:4543–52.
Suzuki T, Abe H, Nagata S, Saitoh F, Iwata S, Ashizawa A, et al. Left ventricular structural characteristics in unilateral renovascular hypertension and primary aldosteronism. Am J Cardiol. 1988;62:1224–7.
Denolle T, Chatellier G, Julien J, Battaglia C, Luo P, Plouin PF. Left ventricular mass and geometry before and after etiologic treatment in renovascular hypertension, aldosterone-producing adenoma, and pheochromocytoma. Am J Hypertens. 1993;6:907–13.
Shigematsu Y, Hamada M, Okayama H, Hara Y, Hayashi Y, Kodama K, et al. Left ventricular hypertrophy precedes other target-organ damage in primary aldosteronism. Hypertension. 1997;29:723–7.
Goldkorn R, Yurenev A, Blumenfeld J, Fishman D, Devereux RB. Echocardiographic comparison of left ventricular structure and function in hypertensive patients with primary aldosteronism and essential hypertension. Am J hypertension. 2002;15:340–5.
Catena C, Colussi G, Lapenna R, Nadalini E, Chiuch A, Gianfagna P, et al. Long-term cardiac effects of adrenalectomy or mineralocorticoid antagonists in patients with primary aldosteronism. Hypertension. 2007;50:911–8.
Morillas P, Castillo J, Quiles J, Nunez D, Guillen S, Bertomeu-Gonzalez V, et al. [Prevalence of primary aldosteronism in hypertensive patients and its effect on the heart]. Rev Esp Cardiol. 2008;61:418–21.
Muiesan ML, Salvetti M, Paini A, Agabiti-Rosei C, Monteduro C, Galbassini G, et al. Inappropriate left ventricular mass in patients with primary aldosteronism. Hypertension. 2008;52:529–34.
Iacobellis G, Petramala L, Cotesta D, Pergolini M, Zinnamosca L, Cianci R, et al. Adipokines and cardiometabolic profile in primary hyperaldosteronism. J Clin Endocrinol Metab. 2010;95:2391–8.
Lin YH, Huang KH, Lee JK, Wang SM, Yen RF, Wu VC, et al. Factors influencing left ventricular mass regression in patients with primary aldosteronism post adrenalectomy. J Renin Angiotensin Aldosterone Syst. 2011;12:48–53.
Lin YH, Lee HH, Liu KL, Lee JK, Shih SR, Chueh SC, et al. Reversal of myocardial fibrosis in patients with unilateral hyperaldosteronism receiving adrenalectomy. Surgery. 2011;150:526–33.
Lin YH, Wang SM, Wu VC, Lee JK, Kuo CC, Yen RF, et al. The association of serum potassium level with left ventricular mass in patients with primary aldosteronism. Eur J Clin Investig. 2011;41:743–50.
Pimenta E, Gordon RD, Ahmed AH, Cowley D, Leano R, Marwick TH, et al. Cardiac dimensions are largely determined by dietary salt in patients with primary aldosteronism: results of a case-control study. J Clin Endocrinol Metab. 2011;96:2813–20.
Curione M, Petramala L, Savoriti C, Verrenti M, Baiocco E, Salvatore S, et al. Electrical and Myocardial Remodeling in Primary Aldosteronism. Front Cardiovasc Med. 2014;1:7.
Cesari M, Letizia C, Angeli P, Sciomer S, Rosi S, Rossi GP. Cardiac remodeling in patients with primary and secondary aldosteronism: a tissue doppler study. Circ Cardiovasc Imaging. 2016;9:e004815.
Yang Y, Zhu LM, Xu JZ, Tang XF, Gao PJ. Comparison of left ventricular structure and function in primary aldosteronism and essential hypertension by echocardiography. Hypertens Res. 2017;40:243–50.
Lin YH, Wu XM, Lee HH, Lee JK, Liu YC, Chang HW, et al. Adrenalectomy reverses myocardial fibrosis in patients with primary aldosteronism. J Hypertens. 2012;30:1606–13.
Liao MT, Wu XM, Chang CC, Liao CW, Chen YH, Lu CC, et al. The Association between Glomerular Hyperfiltration and Left Ventricular Structure and Function in Patients with Primary Aldosteronism. Int J Med Sci. 2015;12:369–77.
Hung CS, Ho YL, Chang YY, Wu VC, Wu XM, Lee JK, et al. Twenty-four-hour urinary aldosterone predicts inappropriate left ventricular mass index in patients with primary aldosteronism. ScientificWorldJournal. 2013;2013:294594.
Frustaci A, Letizia C, Verardo R, Grande C, Francone M, Sansone L, et al. Primary aldosteronism-associated cardiomyopathy: Clinical-pathologic impact of aldosterone normalization. Int J Cardiol. 2019;292:141–7.
Rossi GP, Di Bello V, Ganzaroli C, Sacchetto A, Cesari M, Bertini A, et al. Excess aldosterone is associated with alterations of myocardial texture in primary aldosteronism. Hypertension. 2002;40:23–7.
Galetta F, Bernini G, Franzoni F, Bacca A, Fivizzani I, Tocchini L, et al. Cardiac remodeling in patients with primary aldosteronism. J Endocrinol Investig. 2009;32:739–45.
Freel EM, Mark PB, Weir RA, McQuarrie EP, Allan K, Dargie HJ, et al. Demonstration of blood pressure-independent noninfarct myocardial fibrosis in primary aldosteronism: a cardiac magnetic resonance imaging study. Circ Cardiovasc Imaging. 2012;5:740–7.
Su MY, Wu VC, Yu HY, Lin YH, Kuo CC, Liu KL, et al. Contrast-enhanced MRI index of diffuse myocardial fibrosis is increased in primary aldosteronism. J Magn Reson Imaging. 2012;35:1349–55.
Lee HH, Hung CS, Wu XM, Wu VC, Liu KL, Wang SM, et al. Myocardial ultrasound tissue characterization of patients with primary aldosteronism. Ultrasound Med Biol. 2013;39:54–61.
Grytaas MA, Sellevag K, Thordarson HB, Husebye ES, Lovas K, Larsen TH. Cardiac magnetic resonance imaging of myocardial mass and fibrosis in primary aldosteronism. Endocr Connect. 2018;7:413–24.
Lin YH, Shiau YC, Yen RF, Lin LC, Wu CC, Ho YL, et al. The relation between myocardial cyclic variation of integrated backscatter and serum concentrations of procollagen propeptides in hypertensive patients. Ultrasound Med Biol. 2004;30:885–91.
Hung CS, Chou CH, Wu XM, Chang YY, Wu VC, Chen YH, et al. Circulating tissue inhibitor of matrix metalloproteinase-1 is associated with aldosterone-induced diastolic dysfunction. J Hypertens. 2015;33:1922–30.
Hattori T, Murase T, Sugiura Y, Nagasawa K, Takahashi K, Ohtake M, et al. Effects of salt status and blockade of mineralocorticoid receptors on aldosterone-induced cardiac injury. Hypertens Res. 2014;37:125–33.
Habibi J, DeMarco VG, Ma L, Pulakat L, Rainey WE, Whaley-Connell AT, et al. Mineralocorticoid receptor blockade improves diastolic function independent of blood pressure reduction in a transgenic model of RAAS overexpression. Am J Physiol Heart Circ Physiol. 2011;300:H1484–91.
Stoddard MF, Pearson AC, Kern MJ, Ratcliff J, Mrosek DG, Labovitz AJ. Influence of alteration in preload on the pattern of left ventricular diastolic filling as assessed by Doppler echocardiography in humans. Circulation. 1989;79:1226–36.
Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. Eur J Echocardiogr. 2009;10:165–93.
Paulus WJ, Tschope C, Sanderson JE, Rusconi C, Flachskampf FA, Rademakers FE, et al. How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the Heart Failure and Echocardiography Associations of the European Society of Cardiology. Eur heart J. 2007;28:2539–50.
Ommen SR, Nishimura RA, Appleton CP, Miller FA, Oh JK, Redfield MM, et al. Clinical utility of Doppler echocardiography and tissue Doppler imaging in the estimation of left ventricular filling pressures: a comparative simultaneous Doppler-catheterization study. Circulation. 2000;102:1788–94.
Liao CW, Chen A, Lin YT, Chang YY, Wang SM, Wu VC, et al. The Relation Between the Degree of Left Ventricular Mass Regression and Serum Potassium Level Change in Patients With Primary Aldosteronism After Adrenalectomy. J Investig Med. 2015;63:816–20.
Galderisi M, Petrocelli A, Alfieri A, Garofalo M, de Divitiis O. Impact of ambulatory blood pressure on left ventricular diastolic dysfunction in uncomplicated arterial systemic hypertension. Am J Cardiol. 1996;77:597–601.
Chang YY, Liao CW, Tsai CH, Chen CW, Pan CT, Chen ZW, et al. Left ventricular dysfunction in patients with primary aldosteronism: a propensity score-matching follow-up study with tissue doppler imaging. J Am Heart Assoc. 2019;8:e013263.
Tseng WY, Liao TY, Wang JL. Normal systolic and diastolic functions of the left ventricle and left atrium by cine magnetic resonance imaging. J Cardiovasc Magn Reson. 2002;4:443–57.
Indra T, Holaj R, Strauch B, Rosa J, Petrak O, Somloova Z, et al. Long-term effects of adrenalectomy or spironolactone on blood pressure control and regression of left ventricle hypertrophy in patients with primary aldosteronism. J Renin Angiotensin Aldosterone Syst. 2015;16:1109–17.
Yoshitomi Y, Nishikimi T, Abe H, Yoshiwara F, Suzuki T, Ashizawa A, et al. Comparison of changes in cardiac structure after treatment in secondary hypertension. Hypertension. 1996;27:319–23.
Rossi GP, Cesari M, Cuspidi C, Maiolino G, Cicala MV, Bisogni V, et al. Long-term control of arterial hypertension and regression of left ventricular hypertrophy with treatment of primary aldosteronism. Hypertension (Dallas, Tex: 1979). 2013;62:62–9.
Arabidze GG, Chikhladze NM, Sergakova LM, Iarovaia EB. [Left ventricular myocardial structure and function in patients with primary aldosteronism]. Ter Arkh. 1999;71:13–9.
Rossi GP, Sacchetto A, Pavan E, Scognamiglio R, Pietra M, Pessina AC. Left ventricular systolic function in primary aldosteronism and hypertension. J Hypertens. 1998;16:2075–7.
Liao M-T, Wu X-M, Chang C-C, Liao C-W, Chen Y-H, Lu C-C, et al. The Association between Glomerular Hyperfiltration and Left Ventricular Structure and Function in Patients with Primary Aldosteronism. Int J Med Sci. 2015;12:369–77.
Hung C-S, Wu X-M, Chen C-W, Chen Y-H, Wu V-C, Liao C-W, et al. The relationship among cardiac structure, dietary salt and aldosterone in patients with primary aldosteronism. Oncotarget. 2017;8:73187–97.
Gaddam K, Corros C, Pimenta E, Ahmed M, Denney T, Aban I, et al. Rapid Reversal of Left Ventricular Hypertrophy and Intracardiac Volume Overload in Patients With Resistant Hypertension and Hyperaldosteronism. Hypertension (Dallas, Tex: 1979). 2010;55:1137–42.
Pellerin D, Sharma R, Elliott P, Veyrat C. Tissue Doppler, strain, and strain rate echocardiography for the assessment of left and right systolic ventricular function. Heart (Br Card Soc). 2003;89:iii9–17.
Choi EY, Ha JW, Yoon SJ, Shim CY, Seo HS, Park S, et al. Increased plasma aldosterone-to-renin ratio is associated with impaired left ventricular longitudinal functional reserve in patients with uncomplicated hypertension. J Am Soc Echocardiogr: Off Publ Am Soc Echocardiogr. 2008;21:251–6.
Hidaka T, Shiwa T, Fujii Y, Nishioka K, Utsunomiya H, Ishibashi K, et al. Impact of aldosterone-producing adenoma on cardiac structures in echocardiography. J Echocardiogr. 2013;11:123–9.
Krzesinski P, Uzieblo-Zyczkowska B, Gielerak G, Stanczyk A, Kurpaska M, Piotrowicz K. Global longitudinal two-dimensional systolic strain is associated with hemodynamic alterations in arterial hypertension. J Am Soc Hypertens. 2015;9:680–9.
Mayet J, Ariff B, Wasan B, Chapman N, Shahi M, Senior R, et al. Midwall myocardial shortening in athletic left ventricular hypertrophy. Int J Cardiol. 2002;86:233–8.
Sitia S, Tomasoni L, Turiel M. Speckle tracking echocardiography: a new approach to myocardial function. World J Cardiol. 2010;2:1–5.
Kouzu H, Yuda S, Muranaka A, Doi T, Yamamoto H, Shimoshige S, et al. Left ventricular hypertrophy causes different changes in longitudinal, radial, and circumferential mechanics in patients with hypertension: a two-dimensional speckle tracking study. J Am Soc Echocardiogr: Off Publ Am Soc Echocardiogr. 2011;24:192–9.
Boulestreau R, Cremer A, Delarche N, Gosse P. [Alteration of left ventricular longitudinal systolic function in 2D-strain in primary aldosteronism: A new target organ damage marker]. Annales de Cardiologie et d’angeiologie. 2018;67:315–20.
Wang D, Xu JZ, Chen X, Chen Y, Shao S, Zhang W, et al. Speckle-Tracking Echocardiographic Layer-Specific Strain Analysis on Subclinical Left Ventricular Dysfunction in Patients With Primary Aldosteronism. Am J Hypertens. 2019;32:155–62.
Catena C, Colussi GL, Marzano L, Sechi LA. Predictive factors of left ventricular mass changes after treatment of primary aldosteronism. Horm Metab Res. 2012;44:188–93.
Wu VC, Yang SY, Lin JW, Cheng BW, Kuo CC, Tsai CT, et al. Kidney impairment in primary aldosteronism. Clin Chim Acta. 2011;412:1319–25.
Borlaug BA, Paulus WJ. Heart failure with preserved ejection fraction: pathophysiology, diagnosis, and treatment. Eur heart J. 2011;32:670–9.
Katz AM, Rolett EL. Heart failure: when form fails to follow function. Eur heart J. 2016;37:449–54.
Hoit BD. Left atrial size and function: role in prognosis. J Am Coll Cardiol. 2014;63:493–505.
Reil JC, Hohl M, Selejan S, Lipp P, Drautz F, Kazakow A, et al. Aldosterone promotes atrial fibrillation. Eur heart J. 2012;33:2098–108.
Wang D, Xu JZ, Chen X, Xu TY, Zhang W, Li Y, et al. Left atrial myocardial dysfunction in patients with primary aldosteronism as assessed by speckle-tracking echocardiography. J Hypertens. 2019;37:2032–40.
Monticone S, Burrello J, Tizzani D, Bertello C, Viola A, Buffolo F, et al. Prevalence and Clinical Manifestations of Primary Aldosteronism Encountered in Primary Care Practice. J Am Coll Cardiol. 2017;69:1811–20.
Huang WC, Chen YY, Lin YH, Chen L, Lin PC, Lin YF, et al. Incidental Congestive Heart Failure in Patients With Aldosterone-Producing Adenomas. J Am Heart Assoc. 2019;8:e012410.
Verdecchia P, Carini G, Circo A, Dovellini E, Giovannini E, Lombardo M, et al. Left ventricular mass and cardiovascular morbidity in essential hypertension: the MAVI study. J Am Coll Cardiol. 2001;38:1829–35.
Nadruz W. Myocardial remodeling in hypertension. J Hum Hypertens. 2015;29:1–6.
Verdecchia P, Angeli F, Achilli P, Castellani C, Broccatelli A, Gattobigio R, et al. Echocardiographic left ventricular hypertrophy in hypertension: marker for future events or mediator of events? Curr Opin Cardiol. 2007;22:329–34.
Chen ZW, Tsai CH, Pan CT, Chou CH, Liao CW, Hung CS, et al. Endothelial Dysfunction in Primary Aldosteronism. Int J Mol Sci. 2019;20:5214.
Murata M, Kitamura T, Tamada D, Mukai K, Kurebayashi S, Yamamoto T, et al. Plasma aldosterone level within the normal range is less associated with cardiovascular and cerebrovascular risk in primary aldosteronism. J Hypertens. 2017;35:1079–85.
Ohno Y, Sone M, Inagaki N, Yamasaki T, Ogawa O, Takeda Y, et al. Prevalence of cardiovascular disease and its risk factors in primary aldosteronism: a multicenter study in Japan. Hypertension (Dallas, Tex: 1979). 2018;71:530–7.
Chang YH, Chung SD, Wu CH, Chueh JS, Chen L, Lin PC. et al.Surgery decreases the long-term incident stroke risk in patients with primary aldosteronism. Surgery. 2020;167:367–77.
Hundemer GL, Curhan GC, Yozamp N, Wang M, Vaidya A. Cardiometabolic outcomes and mortality in medically treated primary aldosteronism: a retrospective cohort study. Lancet Diabetes Endocrinol. 2018;6:51–59.
Hundemer GL, Curhan GC, Yozamp N, Wang M, Vaidya A. Incidence of Atrial Fibrillation and Mineralocorticoid Receptor Activity in Patients With Medically and Surgically Treated Primary Aldosteronism. JAMA Cardiol. 2018;3:768–74.
Tsioufis C, Tsiachris D, Dimitriadis K, Stougiannos P, Missovoulos P, Kakkavas A, et al. Myocardial and aortic stiffening in the early course of primary aldosteronism. Clin Cardiol. 2008;31:431–6.
Bernini G, Bacca A, Carli V, Carrara D, Materazzi G, Berti P, et al. Cardiovascular changes in patients with primary aldosteronism after surgical or medical treatment. J Endocrinol Investig. 2012;35:274–80.
Tarazi RC, Ibrahim MM, Bravo EL, Dustan HP. Hemodynamic Characteristics of Primary Aldosteronism. N Engl J Med. 1973;289:1330–5.
Lin YH, Huang KH, Lee JK, Wang SM, Yen RF, Wu VC, et al. Factors influencing left ventricular mass regression in patients with primary aldosteronism post adrenalectomy. J Renin-Angiotensin-Aldosterone Syst. 2011;12:48–53.
Liao CW, Chen A, Lin YT, Chang YY, Wang SM, Wu VC, et al. The relation between the degree of left ventricular mass regression and serum potassium level change in patients with primary aldosteronism after adrenalectomy. J Investig Med: Off Publ Am Fed Clin Res. 2015;63:816–20.
Acknowledgements
This research was supported by grants from the Ministry of Science and Technology (MOST 105-2314-B-002-122-MY3, MOST 106-2314-B-002-169-MY3 and MOST 107-2314-B-002 -264 -MY3), National Taiwan University Hospital (NTUH 107-A141, 108-A141, 109-A141, 108-N01, 108-S4382, UN108-37), and the Excellent Translational Medicine Research Projects of National Taiwan University College of Medicine, and National Taiwan University Hospital (109C 101-43).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tsai, CH., Pan, CT., Chang, YY. et al. Left ventricular remodeling and dysfunction in primary aldosteronism. J Hum Hypertens 35, 131–147 (2021). https://doi.org/10.1038/s41371-020-00426-y
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41371-020-00426-y
This article is cited by
-
Bilateral adrenal artery embolization for the treatment of idiopathic hyperaldosteronism: A proof-of-principle single center study
Hypertension Research (2025)
-
The effect of spironolactone in reducing the risk of postoperative atrial fibrillation in patients undergoing coronary artery bypass graft surgery: randomized single-blind placebo-controlled study
General Thoracic and Cardiovascular Surgery (2025)
-
The relationship between tissue inhibitor of metalloproteinases-1 and KCNJ5 mutation in aldosterone-producing adenoma patients
Hypertension Research (2025)
-
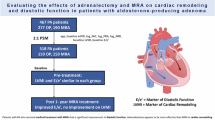
Evaluating the effects of adrenalectomy and mineralocorticoid receptor antagonist on cardiac remodeling and diastolic function in patients with aldosterone-producing adenoma
Hypertension Research (2025)
-
Recent progress in unraveling cardiovascular complications associated with primary aldosteronism: a succinct review
Hypertension Research (2024)