Abstract
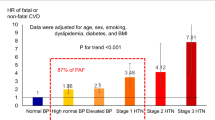
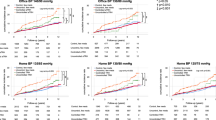
To investigate the association of blood pressure (BP) categories with total and premature cardiovascular disease (CVD) mortality in rural Chinese. The study included 14,539 adults ≥18 years in rural China. Baseline study visits were conducted in 2007–2008, and follow-up visits in 2013–2014. Data were collected by face-to-face questionnaire interview, and anthropometric and laboratory measurements. A sub-distribution hazards model was used to calculate adjusted sub-distribution hazard ratios (aSHRs) and 95% confidence intervals (CIs). During the 6-year follow-up, 257 total and 209 premature CVD deaths occurred. As compared with normal BP (systolic BP/diastolic BP (SBP/DBP) < 120/80 mmHg), for men and people aged ≥60 years, hypertension (SBP/DBP ≥ 140/90 mmHg) associated with total CVD mortality (aSHR 3.57, 95% CI 2.06–6.17; aSHR 2.15, 1.29–3.56) and premature CVD mortality (aSHR 4.41, 2.37–8.21; aSHR 2.31, 1.27–4.19). Also, as compared with normal BP, for men and people aged ≥60 years with high normal BP (SBP/DBP 120–139/80–89 mmHg), risk of total CVD mortality increased (aSHR 1.85, 1.05–3.28; aSHR 1.78, 1.05–3.04), as was premature CVD mortality (aSHR 1.89, 0.99–3.64; aSHR 1.91, 1.03–3.54). Among men and people aged ≥60 years in rural China, risk of total and premature CVD mortality was increased for those with high normal BP and hypertension. Prevention and treatment strategies for additional CVD risk reduction targeting men and elderly people with hypertension or even high normal BP are needed to reduce CVD mortality risk.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Ren Y, Liu Y, Sun X, Wang B, Zhao Y, Liu D, et al. Chocolate consumption and risk of cardiovascular diseases: a meta-analysis of prospective studies. Heart. 2018;105:49–55.
Joint Task Force for Guideline on the Assessment and Management of Cardiovascular Risk in China. Guideline on the assessment and management of cardiovascular risk in China. Chin J Prev Med. 2019;53:13–35.
World Health Organization. Global Health Observatory Data Repository. 2016. http://www.who.int/healthinfo/global_burden_disease/estimates/en/index1.html. Accessed 16 Oct 2018.
National Bureau of Statistics of China. China Statistical Yearbook. 2017. http://www.stats.gov.cn/tjsj/ndsj/2017/indexeh.htm. Accessed 26 June 2018.
The General Assembly. Political Declaration of the High-level Meeting of the General Assembly on the Prevention and Control of Non-communicable Diseases. 2012. http://www.who.int/nmh/events/un_ncd_summit2011/political_declaration_en.pdf. Accessed 22 Oct 2018.
World Health Organization. Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020. http://www.who.int/cardiovascular_diseases/15March2013UpdatedRevisedDraftActionPlanAPPROVEDBYADG.pdf). Accessed 22 Oct 2018.
Campbell NRC, Zhang X. Hypertension in China. Circulation. 2018;137:2357–9.
World Health Organization. Global Burden of Disease (GBD). 2017. http://www.healthdata.org/gbd/data-visualizations. Accessed 21 Oct 2018.
Perkovic V, Huxley R, Wu Y, Prabhakaran D, MacMahon S. The burden of blood pressure-related disease. Hypertension. 2007;50:991–7.
Talaei M, Hosseini N, Koh AS, Yuan JM, Koh WP. Association of “elevated blood pressure” and “stage 1 hypertension” with cardiovascular mortality among an asian population. J Am Heart Assoc. 2018;7:e008911.
He J, Gu D, Chen J, Wu X, Kelly TN, Huang JF, et al. Premature deaths attributable to blood pressure in China: a prospective cohort study. Lancet. 2009;374:1765–72.
Miura K, Daviglus ML, Dyer AR, Liu K, Garside DB, Stamler J, et al. Relationship of blood pressure to 25-year mortality due to coronary heart disease, cardiovascular diseases, and all causes in young adult men. Arch Intern Med. 2001;161:1501.
Huang Y, Su L, Cai X, Mai W, Wang S, Hu Y, et al. Association of all-cause and cardiovascular mortality with prehypertension: a meta-analysis. Am Heart J. 2014;167:160–8.
Bundy JD, Mills KT, Chen J, Li C, Greenland P, He J. Estimating the association of the 2017 and 2014 hypertension guidelines with cardiovascular events and deaths in US adults. JAMA Cardiol. 2018;3:572.
Huebner MPD, Wolkewitz MDSH, Enriquez-Sarano MMD, Schumacher MDRN. Competing risks need to be considered in survival analysis models for cardiovascular outcomes. J Thorac Cardiov Sur. 2017;153:1427–31.
Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94:496–509.
Ren Y, Liu Y, Sun X, Wang B, Zhao Y, Luo X, et al. Cohort study to determine the waist circumference cutoffs for predicting type 2 diabetes mellitus in rural China. Diabetes/Metab Res Rev. 2018;34:e3007.
Zhao Y, Zhang M, Luo X, Yin L, Pang C, Feng T, et al. Association of obesity categories and high blood pressure in a rural adult Chinese population. J Hum Hypertens. 2016;30:613–8.
Yi S, Mok Y, Ohrr H, Yi J, Yun YD, Park J, et al. Low systolic blood pressure and vascular mortality among more than 1 million Korean adults. Circulation. 2016;133:2381–90.
Bérard E, Bongard V, Haas B, Dallongeville J, Moitry M, Cottel D, et al. Score of adherence to 2016 european cardiovascular prevention guidelines predicts cardiovascular and all-cause mortality in the general population. Can J Cardiol. 2017;33:1298–304.
Lacey B, Lewington S, Clarke R, Kong XL, Chen Y, Guo Y, et al. Age-specific association between blood pressure and vascular and non-vascular chronic diseases in 0·5 million adults in China: a prospective cohort study. Lancet Glob Health. 2018;6:e641–9.
Greenberg JA. Removing confounders from the relationship between mortality risk and systolic blood pressure at low and moderately increased systolic blood pressure. J Hypertens. 2003;21:49–56.
Kikuya M, Ohkubo T, Asayama K, Metoki H, Obara T, Saito S, et al. Ambulatory blood pressure and 10-year risk of cardiovascular and noncardiovascular mortality: the Ohasama study. Hypertension. 2005;45:240–5.
Glynn RJ, Field TS, Hebert PR, Taylor JO, Hennekens CH, Rosner B, et al. Evidence for a positive linear relation between blood pressure and mortality in elderly people. Lancet. 1995;345:825–9.
Staessen J, Bulpitt C, Clement D, De Leeuw P, Fagard R, Fletcher A, et al. Relation between mortality and treated blood pressure in elderly patients with hypertension: report of the European Working Party on High Blood Pressure in the Elderly. BMJ. 1989;298:1552–6.
Wildman R, Muntner P, Reynolds K, McGinn AP, Rajpathak S, Wylie-Rosett J. et al. The obese without cardiometabolic risk factor clustering and the normal weight with cardiometabolic risk factor clustering. Arch Intern Med. 2008;168:1617–24.
Gu D, He J, Duan X, Reynolds K, Wu X, Chen J, et al. Body weight and mortality among men and women in China. JAMA. 2006;295:776–83.
Craig CL, Marshall AL, SJ STR MM, Bauman AE, Booth ML, Ainsworth BE. et al. International Physical Activity Questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–95.
Perloff D, Grim C, Flack J, Frohlich ED, Hill M, McDonald M, et al. Human blood pressure determination by sphygmomanometry. Circulation. 1993;88:2460–70.
Bairaktari E, Hatzidimou K, Tzallas C, Vini M, Katsaraki A, Tselepis A, et al. Estimation of LDL cholesterol based on the Friedewald formula and on apo B levels. Clin Biochem. 2000;33:549–55.
Liu LS. Hypertension WGOT. 2018 Chinese guidelines for prevention and treatment of hypertension-a report of the revision committee of chinese guidelines for prevention and treatment of hypertension. J Geriatr Cardiol. 2019;16:182.
Gray RJ. A class of k-sample tests for comparing the cumulative incidence of a competing risk. Ann Stat. 1988;16:1141–54.
Ikeda A, Iso H, Yamagishi K, Inoue M, Tsugane S. Blood pressure and the risk of stroke, cardiovascular disease, and all-cause mortality among Japanese: the JPHC study. Am J Hypertens. 2009;22:273–80.
Vlachopoulos C, Ioakeimidis N, Miner M, Aggelis A, Pietri P, Terentes-Printzios D, et al. Testosterone deficiency: a determinant of aortic stiffness in men. Atherosclerosis. 2014;233:278–83.
Grandas OH, Mountain DH, Kirkpatrick SS, Cassada DC, Stevens SL, Freeman MB, et al. Regulation of vascular smooth muscle cell expression and function of matrix metalloproteinases is mediated by estrogen and progesterone exposure. J Vasc Surg. 2009;49:185–91.
Guzik TJ, Hoch NE, Brown KA, McCann LA, Rahman A, Dikalov S, et al. Role of the T cell in the genesis of angiotensin II induced hypertension and vascular dysfunction. J Exp Med. 2007;204:2449–60.
Russ TC, Stamatakis E, Hamer M, Starr JM, Kivimaki M, Batty GD. Association between psychological distress and mortality: individual participant pooled analysis of 10 prospective cohort studies. BMJ. 2012;345:e4933.
Nambiar L, LeWinter MM, VanBuren PC, Dauerman HL. Decade-long temporal trends in U.S. hypertension-related cardiovascular mortality. J Am Coll Cardiol. 2020;75:2644–6.
Lewington S, Lacey B, Clarke R, Guo Y, Kong XL, Yang L, et al. The burden of hypertension and associated risk for cardiovascular mortality in China. JAMA Intern Med. 2016;176:524.
Huang M, Liu S. Ending the epidemics of cardiovascular diseases: time is now to integrate both population and individual strategies for prevention. Sci Bull. 2018;63:735–6.
Atasoy S, Johar H, Peters A, Ladwig K. Association of hypertension cut-off values with 10-year cardiovascular mortality and clinical consequences: a real-world perspective from the prospective MONICA/KORA study. Eur Heart J. 2019;40:732–8.
Sepanlou SG, Newson RB, Poustchi H, Malekzadeh MM, Asl PR, Etemadi A, et al. Cardiovascular disease deaths and years of life lost attributable to non-optimal systolic blood pressure and hypertension in Northeastern Iran. Arch Iran Med. 2015;18:144–52.
Yano Y, Stamler J, Garside DB, Daviglus ML, Franklin SS, Carnethon MR, et al. Isolated systolic hypertension in young and middle-aged adults and 31-year risk for cardiovascular mortality. J Am Coll Cardiol. 2015;65:327–35.
Oh J, Allison MA, Barrett-Connor E. Different impacts of hypertension and diabetes mellitus on all-cause and cardiovascular mortality in community-dwelling older adults. J Hypertens. 2017;35:55–62.
Mendy A. Association of urinary nitrate with lower prevalence of hypertension and stroke and with reduced risk of cardiovascular mortality. Circulation. 2018;137:2295–7.
Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387:957–67.
Poulter NR, Prabhakaran D, Caulfield M. Hypertension. Lancet. 2015;386:801–12.
Acknowledgements
The investigators are grateful to the dedicated participants and all research staff of the study.
Funding
This study was supported by the National Natural Science Foundation of China (grant numbers 81373074, 81402752, and 81673260); the Natural Science Foundation of Guangdong Province (grant number 2017A030313452); the Medical Research Foundation of Guangdong Province (grant number A2017181); and the Science and Technology Development Foundation of Shenzhen (grant numbers JCYJ20140418091413562, JCYJ20160307155707264, JCYJ20170302143855721, and JCYJ20170412110537191).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Liu, L., Liu, Y., Ren, Y. et al. Deaths from total and premature cardiovascular disease associated with high normal blood pressure and hypertension in rural Chinese men and elderly people. J Hum Hypertens 35, 741–750 (2021). https://doi.org/10.1038/s41371-020-0379-4
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41371-020-0379-4