Abstract
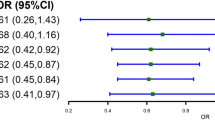
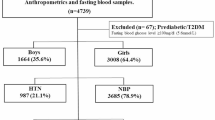
To explore the relationship between serum folic acid (FA) or Vitamin B12 (VB12) and elevated BP in children and adolescents. Both a nested case control and a cohort study were designed to explore the relationship between serum folic acid (FA) or Vitamin B12 (VB12) and elevated blood pressure (BP). All the included participants were from primary school. A total of 326 subjects (116:210) in nested case control were from an established cohort. And 270 participants without hypertension at baseline and followed in 2019 in cohort. FA and VB12 levels were lower in the elevated BP group than in the control group, and homocysteine level was higher than that in the control group. In the elevated BP group, overweight/obese children had lower FA than overweight/obese children in the normal BP group. FA was positively correlated with high-density lipoprotein (HDL) and Apo lipoprotein A (APOA), but negatively correlated with triglyceride (TG). FA was significantly correlated with elevated BP in children and adolescents (β = –0.353, P = 0.032), after adjusting VB12, and homocysteine (HCY), and the interaction effect of FA*HCY was significant. Both systolic and diastolic BP levels were statistically lower in the FA high exposure group than in the FA low exposure group in the cohort study. This study found that FA and vitamin B12 deficiency in childhood was correlated with elevated BP levels, which may affect BP by regulating lipid levels, and confirmed the importance of maintaining high levels of FA and vitamin B12 in childhood either by diet or supplementation.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
Data are available from Xiaohua Liang (contact via xiaohualiang@hospital.cqmu.edu.cn, or liangxiaohua666@sina.com).
References
Fuchs FD, Whelton PK. High blood pressure and cardiovascular disease. Hypertension (Dallas, Tex. : 1979). 2020;75:285–92.
Song P, Zhang Y, Yu J, Zha M, Zhu Y, Rahimi K, et al. Global prevalence of hypertension in children: a systematic review and meta-analysis. JAMA Pediatr. 2019;173:1154–63.
Zhao Y, Wang L, Xue B, Wang Y. Associations between general and central obesity and hypertension among children: The Childhood Obesity Study in China Mega-Cities. Scientific reports. 2017;7:16895.
Liang X, Xiao L, Luo Y, Xu J. Prevalence and risk factors of childhood hypertension in urban-rural areas of china: a cross-sectional study. Int J Hypertens. 2020;2020:2374231.
Liang X, Chen M, Qu P, Hao G, Huang Y, Chen J, et al. The association of vitamin A and vitamin D with hypertension in children: a case-control study. Int J Hypertens. 2018;2018:9295147.
Wang Y, Liu L, Jin Z, Zhang D. [Advances in metabolic engineering for vitamins production]. Sheng Wu Gong Cheng Xue Bao. 2021;37:1748–70.
Czernichow S, Blacher J, Hercberg S. Antioxidant vitamins and blood pressure. Curr Hypertension Rep. 2004;6:27–30.
Latic N, Erben RG. Vitamin D and cardiovascular disease, with emphasis on hypertension, atherosclerosis, and heart failure. Int J Mol Sci. 2020;1-15.
McMullan CJ, Borgi L, Curhan GC, Fisher N, Forman JP. The effect of vitamin D on renin-angiotensin system activation and blood pressure: a randomized control trial. J Hypertens. 2017;35:822–9.
Lee Y, Park S. Serum folate levels and hypertension. Sci Rep. 2022;12:10071.
Tzoulaki I, Patel CJ, Okamura T, Chan Q, Brown IJ, Miura K, et al. A nutrient-wide association study on blood pressure. Circulation. 2012;126:2456–64.
Schutte AE, van Rooyen JM, Huisman HW, Kruger HS, Malan NT, De Ridder JH, et al. Dietary risk markers that contribute to the aetiology of hypertension in black South African children: the THUSA BANA study. J Hum Hypertens. 2003;17:29–35.
Tamai Y, Wada K, Tsuji M, Nakamura K, Sahashi Y, Watanabe K, et al. Dietary intake of vitamin B12 and folic acid is associated with lower blood pressure in Japanese preschool children. Am J Hypertens. 2011;24:1215–21.
Silva LL, Fawzi WW, Cardoso MA. Group EW. Serum folate and vitamin B12 status in young Brazilian children. Public health nutrition. 2019;22:1223–31.
Liang X, Xiao L, Luo Y, Xu J. Prevalence and risk factors of childhood hypertension from birth through childhood: a retrospective cohort study. J Hum Hypertens. 2020;34:151–64.
Feng Y, Bi Y, Tang X, Zhang P, Tong J, Peng X, et al. Protective effects of appropriate amount of nuts intake on childhood blood pressure level: a cross-sectional study. Front Med (Lausanne). 2021;8:793672.
Tong J, Ren Y, Liu F, Liang F, Tang X, Huang D, et al. The impact of PM2.5 on the growth curves of children’s obesity indexes: a prospective cohort study. Front Public Health. 2022;10:843622.
Liang X, Chen J, An X, Liu F, Liang F, Tang X, et al. The impact of PM2.5 on children’s blood pressure growth curves: a prospective cohort study. Environ Int. 2022;158:107012.
Fan H, Yan Y, Mi J. Updating blood pressure references for Chinese children aged 3–17 years. Chin J Hypertens. 2017;25:428–35.
Tamura T, Kuriyama N, Koyama T, Ozaki E, Matsui D, Kadomatsu Y, et al. Association between plasma levels of homocysteine, folate, and vitamin B(12), and dietary folate intake and hypertension in a cross-sectional study. Scientific reports. 2020;10:18499.
Dufficy L, Naumovski N, Ng X, Blades B, Yates Z, Travers C, et al. G80A reduced folate carrier SNP influences the absorption and cellular translocation of dietary folate and its association with blood pressure in an elderly population. Life sciences. 2006;79:957–66.
Forman JP, Rimm EB, Stampfer MJ, Curhan GC. Folate intake and the risk of incident hypertension among US women. JAMA. 2005;293:320–9.
Shen M, Tan H, Zhou S, Retnakaran R, Smith GN, Davidge ST, et al. Serum folate shows an inverse association with blood pressure in a cohort of Chinese women of childbearing age: a cross-sectional study. PloS one. 2016;11:e0155801.
Pogribny IP, Kutanzi K, Melnyk S, de, Conti A, Tryndyak V, et al. Strain-dependent dysregulation of one-carbon metabolism in male mice is associated with choline- and folate-deficient diet-induced liver injury. FASEB J. 2013;27:2233–43.
Ued FV, Mathias MG, Toffano RBD, Barros TT, Almada M, Salomao RG et al. Vitamin B2 and folate concentrations are associated with ARA, EPA and DHA fatty acids in red blood cells of Brazilian children and adolescents. Nutrients. 2019;1-17.
Adaikalakoteswari A, Jayashri R, Sukumar N, Venkataraman H, Pradeepa R, Gokulakrishnan K, et al. Vitamin B12 deficiency is associated with adverse lipid profile in Europeans and Indians with type 2 diabetes. Cardiovasc Diabetol. 2014;13:129.
Chew TW, Jiang X, Yan J, Wang W, Lusa AL, Carrier BJ, et al. Folate intake, MTHFR genotype, and sex modulate choline metabolism in mice. The Journal of nutrition. 2011;141:1475–81.
Ghosh S, Sinha JK, Putcha UK, Raghunath M. Severe but not moderate vitamin B12 deficiency impairs lipid profile, induces adiposity, and leads to adverse gestational outcome in female C57BL/6 mice. Front Nutr. 2016;3:1.
Liang X, Tang X, Xi B, Qu P, Ren Y, Hao G. Abdominal obesity-related lipid metabolites may mediate the association between obesity and glucose dysregulation. Pediatric research. 2023;93:183–8.
Antoniades C, Shirodaria C, Leeson P, Baarholm OA, Van-Assche T, Cunnington C, et al. MTHFR 677 C>T Polymorphism reveals functional importance for 5-methyltetrahydrofolate, not homocysteine, in regulation of vascular redox state and endothelial function in human atherosclerosis. Circulation. 2009;119:2507–15.
Antoniades C, Shirodaria C, Warrick N, Cai S, de Bono J, Lee J, et al. 5-methyltetrahydrofolate rapidly improves endothelial function and decreases superoxide production in human vessels: effects on vascular tetrahydrobiopterin availability and endothelial nitric oxide synthase coupling. Circulation. 2006;114:1193–201.
Li Q, Youn JY, Siu KL, Murugesan P, Zhang Y, Cai H. Knockout of dihydrofolate reductase in mice induces hypertension and abdominal aortic aneurysm via mitochondrial dysfunction. Redox Biol. 2019;24:101185.
Wang H, Mueller NT, Li J, Sun N, Huo Y, Ren F, et al. Association of maternal plasma folate and cardiometabolic risk factors in pregnancy with elevated blood pressure of offspring in childhood. Am J Hypertens. 2017;30:532–40.
Papandreou D, Malindretos P, Arvanitidou M, Makedou A, Rousso I. Homocysteine lowering with folic acid supplements in children: effects on blood pressure. Int J Food Sci Nutr. 2010;61:11–7.
Pravenec M, Kozich V, Krijt J, Sokolova J, Zidek V, Landa V, et al. Folate deficiency is associated with oxidative stress, increased blood pressure, and insulin resistance in spontaneously hypertensive rats. Am J Hypertens. 2013;26:135–40.
Acknowledgements
We would like to acknowledge the laboratory support of the Ministry of Education Key Laboratory of Child Development and Disorders and all of the staff members of the 6 elementary schools in the two regions.
Funding
This work was supported by the Project of Chongqing Science and Technology Bureau (No. CSTB2023NSCQ-MSX0181, No.CSTC2021jscx-gksb-N0001), the Natural Science Foundation Project (No. 82373590), the National Clinical Research Center for Child Health and Disorders (NCRCCHD-2022-GP-01), Program for Youth Innovation in Future Medicine from Chongqing Medical University (No.W0088), National key research and development project (No.2017YFC0211705), Intelligent Medicine Project (No.ZHYX202109). The funders had no role in the whole study research process, including study design, the data collection, and analysis, the decision to publish, or the preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
XH: Conceptualization, Methodology, Writing—Review & Editing; DC: Revision, Writing—Review & Editing; YB: Investigation, Supervision; YH: Investigation, Supervision; TY: Revision, Investigation, Supervision; QL: Investigation, Supervision; GM: Investigation, Supervision; JS: Investigation, Supervision; LC: Validation, Resources; YW: Validation, Resources; XZ: Writing—Original Draft, Review & Editing; XP: Review & Editing; MF: Review & Editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The Institutional Review Board at the Children’s Hospital of Chongqing Medical University gave its approval for the study. Informed consent to participate in this study was provided by all of the children and their parents/guardians.
Consent for publication
All authors critically reviewed and approved the publication of the final paper.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liang, X., Huang, D., Bi, Y. et al. The impact of folic acid/VB12 deficiency on essential hypertension in children and adolescents: from a nested case-control and a cohort study. J Hum Hypertens 38, 844–850 (2024). https://doi.org/10.1038/s41371-024-00955-w
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41371-024-00955-w