Abstract
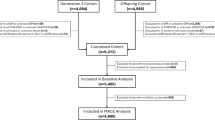
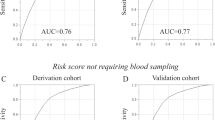
Hypertension is still a common chronic disease worldwide and seriously affects human health. Aim of this study was to investigate the association between tricarboxylic acid (TCA) cycle-related metabolites and hypertension in older adults. A total of 1127 community-dwelling older adults were included in this cross-sectional analysis, of whom 609 were assigned to the hypertension group and 518 to the no-hypertension group. Plasma concentrations of 8 TCA cycle-related metabolites (citrate, cis-aconitate, isocitrate, 2-oxoglutarate, succinate, maleate, fumarate, and malate) were determined by gas chromatography–triple quadrupole mass spectrometry. Multivariate logistic regression was used to assess the association between these metabolites and hypertension risk. After adjustment for covariates, we found that the increased plasma concentrations of 2-oxoglutarate and malate were significantly associated with hypertension. These two associations remained unchanged after using the false discovery rate (FDR)-adjustment method (both FDR-adjusted P-trend <0.05). In stratified analysis, these two associations were not modified by overweight, physical activity, and current drinking (all P-interaction >0.05). In the multivariate diagnostic model, the inclusion of these two metabolites modestly and significantly improved the diagnosis of hypertension (AUC = 0.64, 95% CI: 0.60–0.67). These results indicated that plasma 2-oxoglutarate and malate might be the candidate metabolic markers of hypertension among older adults. However, further longitudinal and experimental studies are necessary to confirm this finding.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the corresponding author.
References
Zhang M, Shi Y, Zhou B, Huang Z, Zhao Z, Li C, et al. Prevalence, awareness, treatment, and control of hypertension in China, 2004-18: findings from six rounds of a national survey. BMJ. 2023;380:e071952.
Oliveros E, Patel H, Kyung S, Fugar S, Goldberg A, Madan N, et al. Hypertension in older adults: Assessment, management, and challenges. Clin Cardiol. 2020;43:99–107.
Wang Z, Wang S, Lin H, Wang C, Gao D. Prevalence of hypertension and related risk factors in older Chinese population: a meta-analysis. Front Public Health. 2024;12:1320295.
Franklin SS, Larson MG, Khan SA, Wong ND, Leip EP, Kannel WB, et al. Does the relation of blood pressure to coronary heart disease risk change with aging? The Framingham Heart Study. Circulation. 2001;103:1245–9.
Qiu W, Cai A, Nie Z, Wang J, Ou Y, Feng Y. Cardiometabolic factors and population risks of cardiovascular disease in community-dwelling adults with varied blood pressure statuses. Diab Obes Metab. 2024;26:3261–71.
Li K, Gao L, Jiang Y, Jia J, Li J, Fan F, et al. Association of cardiovascular events with central systolic blood pressure: A systemic review and meta-analysis. J Clin Hypertens. 2024;26:747–56.
Bullo M, Papandreou C, Garcia-Gavilan J, Ruiz-Canela M, Li J, Guasch-Ferre M, et al. Tricarboxylic acid cycle related-metabolites and risk of atrial fibrillation and heart failure. Metab Clin Exp. 2021;125:154915.
Santos JL, Ruiz-Canela M, Razquin C, Clish CB, Guasch-Ferre M, Babio N, et al. Circulating citric acid cycle metabolites and risk of cardiovascular disease in the PREDIMED study. Nutr Metab Cardiovasc Dis NMCD. 2023;33:835–43.
Haas J, Frese KS, Sedaghat-Hamedani F, Kayvanpour E, Tappu R, Nietsch R, et al. Energy Metabolites as Biomarkers in Ischemic and Dilated Cardiomyopathy. Int J Mol Sci. 2021;22:1999.
Doenst T, Nguyen TD, Abel ED. Cardiac metabolism in heart failure: implications beyond ATP production. Circulation Res. 2013;113:709–24.
Nelson SE, Ament Z, Wolcott Z, Gerszten RE, Kimberly WT. Succinate links atrial dysfunction and cardioembolic stroke. Neurology. 2019;92:e802–e10.
Juraschek SP, Bower JK, Selvin E, Subash Shantha GP, Hoogeveen RC, Ballantyne CM, et al. Plasma lactate and incident hypertension in the atherosclerosis risk in communities study. Am J Hypertens. 2015;28:216–24.
Crawford SO, Ambrose MS, Hoogeveen RC, Brancati FL, Ballantyne CM, Young JH. Association of lactate with blood pressure before and after rapid weight loss. Am J Hypertens. 2008;21:1337–42.
Wu W, Jiang S, Zhao Q, Zhang K, Wei X, Zhou T, et al. Associations of environmental exposure to metals with the risk of hypertension in China. Sci Total Environ. 2018;622-623:184–91.
Hu MJ, He JL, Tong XR, Yang WJ, Zhao HH, Li GA, et al. Associations between essential microelements exposure and the aggressive clinicopathologic characteristics of papillary thyroid cancer. Biometals Int J role Met Ions Biol Biochem Med. 2021;34:909–21.
Merino J, Leong A, Liu CT, Porneala B, Walford GA, von Grotthuss M, et al. Metabolomics insights into early type 2 diabetes pathogenesis and detection in individuals with normal fasting glucose. Diabetologia. 2018;61:1315–24.
Osuna-Prieto FJ, Martinez-Tellez B, Ortiz-Alvarez L, Di X, Jurado-Fasoli L, Xu H, et al. Elevated plasma succinate levels are linked to higher cardiovascular disease risk factors in young adults. Cardiovasc Diabetol. 2021;20:151.
Muller OJ, Heckmann MB, Ding L, Rapti K, Rangrez AY, Gerken T, et al. Comprehensive plasma and tissue profiling reveals systemic metabolic alterations in cardiac hypertrophy and failure. Cardiovasc Res. 2019;115:1296–305.
Guo Y, Chen SF, Zhang YR, Wang HF, Huang SY, Chen SD, et al. Circulating metabolites associated with incident myocardial infarction and stroke: A prospective cohort study of 90 438 participants. J Neurochem. 2022;162:371–84.
Calderon-Santiago M, Priego-Capote F, Galache-Osuna JG, Luque de Castro MD. Method based on GC-MS to study the influence of tricarboxylic acid cycle metabolites on cardiovascular risk factors. J Pharm Biomed Anal. 2013;74:178–85.
Mouton AJ, Li X, Hall ME, Hall JE. Obesity, Hypertension, and Cardiac Dysfunction: Novel Roles of Immunometabolism in Macrophage Activation and Inflammation. Circulation Res. 2020;126:789–806.
Passacquale G, Di Giosia P, Ferro A. The role of inflammatory biomarkers in developing targeted cardiovascular therapies: lessons from the cardiovascular inflammation reduction trials. Cardiovasc Res. 2016;109:9–23.
Gao S, Zhao J, Liu X, Liu L, Chen R. Metabolomics reveals serum metabolic signatures in H-type hypertension based on mass spectrometry multi-platform. Eur J Clin Investig. 2023;53:e14063.
Wu N, Yang M, Gaur U, Xu H, Yao Y, Li D. Alpha-Ketoglutarate: Physiological Functions and Applications. Biomolecules Therapeutics. 2016;24:1–8.
Shi M, He J, Li C, Lu X, He WJ, Cao J, et al. Metabolomics study of blood pressure salt-sensitivity and hypertension. Nutr Metab Cardiovasc Dis. 2022;32:1681–92.
Wawrzyniak R, Gresner P, Lewicka E, Macioszek S, Furga A, Zieba B, et al. Metabolomics Meets Clinics: A Multivariate Analysis of Plasma and Urine Metabolic Signatures in Pulmonary Arterial Hypertension. J Proteome Res. 2024;23:2795–804.
An D, Zeng Q, Zhang P, Ma Z, Zhang H, Liu Z, et al. Alpha-ketoglutarate ameliorates pressure overload-induced chronic cardiac dysfunction in mice. Redox Biol. 2021;46:102088.
Gyanwali B, Lim ZX, Soh J, Lim C, Guan SP, Goh J, et al. Alpha-Ketoglutarate dietary supplementation to improve health in humans. Trends Endocrinol Metab TEM. 2022;33:136–46.
Cheng T, Wang H, Hu Y. The causal effects of genetically determined human blood metabolites on the risk of atrial fibrillation. Front Cardiovasc Med. 2023;10:1211458.
Sanchez-Gimenez R, Peiro OM, Bonet G, Carrasquer A, Fragkiadakis GA, Bullo M, et al. TCA cycle metabolites associated with adverse outcomes after acute coronary syndrome: mediating effect of renal function. Front Cardiovasc Med. 2023;10:1157325.
Edosuyi O, Adesuyi A, Choi M, Igbe I, Oyekan A. Malate reduced blood pressure and exerted differential effects on renal hemodynamics; role of the nitric oxide system and renal epithelial sodium channels (E(Na)C). Eur J Pharmacol. 2023;938:175441.
Hou E, Sun N, Zhang F, Zhao C, Usa K, Liang M, et al. Malate and Aspartate Increase L-Arginine and Nitric Oxide and Attenuate Hypertension. Cell Rep. 2017;19:1631–9.
Rinschen MM, Palygin O, El-Meanawy A, Domingo-Almenara X, Palermo A, Dissanayake LV, et al. Accelerated lysine metabolism conveys kidney protection in salt-sensitive hypertension. Nat Commun. 2022;13:4099.
Cuthbertson I, Morrell NW, Caruso P. BMPR2 Mutation and Metabolic Reprogramming in Pulmonary Arterial Hypertension. Circulation Res. 2023;132:109–26.
Martinez-Reyes I, Chandel NS. Mitochondrial TCA cycle metabolites control physiology and disease. Nat Commun. 2020;11:102.
Funding
This work was supported by the Project of Special Foundation for Science and Technology Development of Central Government Guiding Locals (grant number: 202007d07050008), and the Scientific Research Project for Health Commission of Anhui Province (grant number: AHWJ2021a026).
Author information
Authors and Affiliations
Contributions
Qi-Rong Qin: Conceptualization, Funding acquisition, Data curation, Writing - original draft. Jian Chen: Conceptualization, Project administration. Wen-Lei Hu, Jian-Jun Liu, Meng-Yu Liu: Investigation, Data curation. Fen Huang: Conceptualization, Methodology, Project administration. Ming-Jun Hu: Conceptualization, Methodology, Formal analysis, Writing - review & editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Bioethics Committee of Ma’anshan Center for Disease Control (No. 2020001).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Qin, QR., Chen, J., Hu, WL. et al. Association of tricarboxylic acid cycle related-metabolites with hypertension in older adults: a community-based cross-sectional study. J Hum Hypertens 39, 51–57 (2025). https://doi.org/10.1038/s41371-024-00976-5
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41371-024-00976-5