Abstract
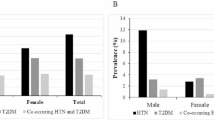
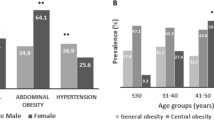
Hypertension, often referred to as a “silent killer,” due to its lack of obvious symptoms but can lead to devastating complications such as cardiovascular disease and stroke, particularly when left unmanaged. This highlights the importance of early screening of elevated blood pressure. The aim of this study is to determine the prevalence of elevated blood pressure (prehypertension) and hypertension among undergraduate university students, along with the associated risk factors. We recruited 344 randomly selected undergraduate students for a cross-sectional study. Blood pressure (BP) measurements were taken following best practice guidelines. In addition, body mass index (BMI) was measured, while other risk factors were collected through a questionnaire. Out of all participants, 36% exhibited elevated blood pressure, with the following breakdown: 15% (n = 51) had prehypertension, 18% (n = 62) had stage 1 hypertension, and 3% (n = 10) had stage 2 hypertension. The prevalence of hypertension and prehypertension was significantly higher among male students (52.7 and 100%, respectively) compared to female students (47.3, and 0% respectively). Significant correlations were found between blood pressure, BMI, and physical activity levels (P ≤ 0.001 and P ≤ 0.011, respectively). Our findings reveal a concerning prevalence of prehypertension and, to a greater extent, hypertension among undergraduate university students. Elevated blood pressure levels were strongly correlated with male gender, BMI, and physical activity levels. These results warrant further large-scale investigation and underscore the urgent need to raise awareness about this significant health risk in the younger population.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
Public data is not applicable to this study. Study data are available from the corresponding author upon reasonable request.
References
World Health Organization. (2023). Global report on hypertension: The race against a silent killer. World Health Organization. https://www.who.int/publications/i/item/9789240081062.
American Heart Association. Know your risk factors for high blood pressure. 2023. https://www.heart.org/en/health-topics/high-blood-pressure/know-your-risk-factors-for-high-blood-pressure.
Centers for Disease Control and Prevention. High blood pressure. 2023 https://www.cdc.gov/bloodpressure/facts.htm.
Hirsch L, & Zieve D (Eds.). Essential hypertension. In: StatPearls. StatPearls Publishing; 2023. https://www.ncbi.nlm.nih.gov/books/NBK539859/.
Cleveland Clinic. Secondary hypertension. 2019. https://my.clevelandclinic.org/health/diseases/21128-secondary-hypertension.
Mayo Clinic. High blood pressure (hypertension). 2023. https://www.mayoclinic.org/diseases-conditions/high-blood-pressure/symptoms-causes/syc-20373410.
World Health Organization. First WHO report details devastating impact of hypertension and ways to stop it. 2023. https://www.who.int/news/item/19-09-2023-first-who-report-details-devastating-impact-of-hypertension-and-ways-to-stop-it.
World Heart Federation. Hypertension. 2023. https://www.world-heart-federation.org/hypertension.
Alhyas L, McKay A, Balasanthiran A, Majeed A. Prevalences of overweight, obesity, hyperglycaemia, hypertension and dyslipidaemia in the gulf: systematic review. JRSM Short Rep. 2011;2:55. https://doi.org/10.1258/shorts.2011.011019.
Zare MG, Okati-Aliabad H, Ansari-Moghaddam A, Mohammadi M, Shahraki-Sanavi F. Prevalence and risk factors of pre-hypertension and hypertension among adults in Southeastern Iran: findings from the baseline survey of the Zahedan adult cohort study. PLoS ONE. 2023;18:e0295270. https://doi.org/10.1371/journal.pone.0295270.
Vo HK, Nguyen DV, Vu TT, Tran HB, Nguyen HTT. Prevalence and risk factors of prehypertension/hypertension among freshman students from the Vietnam National University: a cross-sectional study. BMC Public Health. 2023;23:1166. https://doi.org/10.1186/s12889-023-16118-4.
Hardy ST, Loehr LR, Butler KR, Chakladar S, Chang PP, Folsom AR, et al. Reducing the blood pressure-related burden of cardiovascular disease: impact of achievable improvements in blood pressure prevention and control. J Am Heart Assoc. 2015;4:e002276. https://doi.org/10.1161/JAHA.115.002276.
Wu J, Han X, Sun D, Zhang J, Li J, Qin G, et al. Age-specific association of stage of hypertension at diagnosis with cardiovascular and all-cause mortality among elderly patients with hypertension: a cohort study. BMC Cardiovasc Disord. 2023;23:270. https://doi.org/10.1186/s12872-023-03250-7.
Riley, L., Guthold, R., Cowan, M., Savin, S., Bhatti, L., & Armstrong, T. (2016). The World Health Organization STEPwise approach to noncommunicable disease risk factor surveillance: The WHO STEPS surveillance manual. Am J Public Health. 106(1), 166–168. https://doi.org/10.2105/AJPH.2015.302962.
Weir CB, Jan A. BMI classification percentile and cut off points. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023. https://www.ncbi.nlm.nih.gov/books/NBK541070/.
American Heart Association. (2024, May 17). Understanding blood pressure readings. American Heart Association. https://www.heart.org/en/health-topics/high-blood-pressure/understanding-blood-pressure-readings.
IBM Corp. IBM SPSS statistics for windows, version 25.0. Armonk, NY: IBM Corp; 2017.
Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/apha/ash/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:1269–324. https://doi.org/10.1161/hyp.0000000000000065.
Hujova Z. The prevalence of obesity and hypertension among first-year students at Trnava university in Slovakia. Int J Med Med Sci. 2013;5:Article ED2780D19. https://doi.org/10.5897/IJMMS2013.0925.
Karatzi K, Protogerou AD, Moschonis G, Tsirimiagou C, Androutsos O, Chrousos GP, et al. Prevalence of hypertension and hypertension phenotypes by age and gender among schoolchildren in Greece: the healthy growth study. Atherosclerosis. 2017;259:128–33. https://doi.org/10.1016/j.atherosclerosis.2017.01.027.
Ostchega Y, Fryar CD, Nwankwo T, Nguyen DT. Hypertension prevalence among adults aged 18 and over: United States, 2017-2018. NCHS Data Brief. 2020;364:1–8.
Al-Majed HT, Sadek AA. Pre-hypertension and hypertension in college students in Kuwait: a neglected issue. J Family Community Med. 2012;19:105–12. https://doi.org/10.4103/2230-8229.98296.
Abbas AH, Hamoud SS, Chabuk SK. Blood pressure assessment in undergraduate medical students: impact of gender, body mass index and family history of hypertension. Med J Babylon. 2016;13:307–15. https://www.iasj.net/iasj/article/113329.
Alhawari HH, Al-Shelleh S, Alhawari HH, Al-Saudi A, Aljbour Al-Majali D, Al-Faris L, et al. Blood pressure and its association with gender, body mass index, smoking, and family history among university students. Int J Hypertens. 2018;2018:4186496. https://doi.org/10.1155/2018/4186496.
Tadesse T, Alemu H. Hypertension and associated factors among university students in Gondar, Ethiopia: a cross-sectional study. BMC Public Health. 2014;14:937. https://doi.org/10.1186/1471-2458-14-937.
Gyamfi D, Obirikorang C, Acheampong E, Danquah KO, Asamoah EA, Liman FZ, et al. Prevalence of pre-hypertension and hypertension and its related risk factors among undergraduate students in a tertiary institution, Ghana. Alex J Med. 2018;54:475–80.
National Institutes of Health. (n.d.). International physical activity questionnaire (IPAQ) long form. National Institutes of Health Pain Consortium. https://www.painconsortium.nih.gov/sites/default/files/documents/IPAQ_Long_CRF_v1.0.docx.
Acknowledgements
We would like to thank the student participants in our study and the Family Medicine Department for their support and for providing the blood pressure devices used in this research.
Funding
No financial assistance was received to support the conduct of this study or the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
YAA, BMJ, KRS, RKA, SML, and TTS contributed to the design of the questionnaire, obtained ethical approval, and participated in data collection, extraction, analysis, and manuscript writing. AH and ABE provided feedback on questionnaire design, data analysis, and manuscript writing. ABE supervised the study process, conducted the final editing, and submitted the manuscript.
Corresponding author
Ethics declarations
Ethics
All methods were performed in accordance with the relevant guidelines and regulations. This study was approved by the University of Sharjah Research Ethics Committee (REC- 23-02-18-12-S). Informed consent was obtained from all participants prior to completing the questionnaire and having their blood pressure measurements taken.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Abd Alsamad, Y.A., Jaffal, B.M.S., Shuhait, K.R.I. et al. High prevalence of elevated blood pressure (prehypertension) and hypertension among undergraduate university students in the UAE: a serious health concern. J Hum Hypertens 39, 442–447 (2025). https://doi.org/10.1038/s41371-025-01015-7
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41371-025-01015-7