Abstract
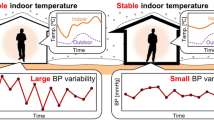
Extreme temperature events related to climate change may impact blood pressure (BP). African American populations are disproportionately affected by temperature extremes due to structural inequities. We examined the association between ambient outdoor temperature and BP among participants in JHS, a cohort of African American adults residing in the tri-county area of Jackson, Mississippi. Our primary hypothesis is that daily higher outdoor ambient temperatures would be associated with lower BP. We used a linear-mixed effects model to determine the relationship between temperature and systolic and diastolic blood pressure (SBP and DBP) at three visits (N = 5296). Participants had BP readings across three visits: Visit 1 (2000–2004), Visit 2 (2005–2008), Visit 3 (2009–2013). Cardiovascular disease (CVD), diabetes, BP medication, sex, age, and visit number were included as adjustment variables. For every 1-degree Celsius higher average temperature from the mean, SBP was 0.11 mm Hg lower (95% CI: −0.14, −0.07, p < 0.001) in adjusted models. Similarly, for every 1-degree Celsius higher average temperature from the mean, DBP was 0.06 mm Hg lower (95% CI: −0.08, −0.04) in adjusted models. The associations were weakly curvilinear (inverted U-shape) with significant quadratic terms. This relationship was not modified by markers of socioeconomic status. This is the first study in the Jackson Heart Study (JHS) to investigate the association between temperature and blood pressure. Further research is needed to explore this relationship in vulnerable populations living in areas prone to extreme temperatures.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the Jackson Heart Study but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of the Jackson Heart Study.
Code availability
The code used for this paper is available upon request from the author.
References
Wilson B. Urban heat management and the legacy of redlining. J Am Plan Assoc. 2020;86:443–57.
Agency EP Climate Change and Social Vulnerability in the United States: A Focus on Six Impacts.; 2021.
Liu J, Varghese BM, Hansen A, Zhang Y, Driscoll T, Morgan G, et al. Heat exposure and cardiovascular health outcomes: a systematic review and meta-analysis. Lancet Planet Health. 2022;6:e484–e95.
Loop MS, Howard G, de Los Campos G, Al-Hamdan MZ, Safford MM, Levitan EB, et al. Heat maps of hypertension, diabetes mellitus, and smoking in the continental United States. Circulation: Cardiovascular Qual Outcomes. 2017;10:e003350.
Hansen A, Bi L, Saniotis A, Nitschke M. Vulnerability to extreme heat and climate change: is ethnicity a factor? Glob Health Action. 2013;6:21364.
Kawada T. Socioeconomic status and cardiovascular disease. Int J Cardiol. 2019;274:378.
He J, Zhu Z, Bundy JD, Dorans KS, Chen J, Hamm LL. Trends in cardiovascular risk factors in US adults by race and ethnicity and socioeconomic status, 1999–2018. JAMA. 2021;326:1286–98.
Peters A, Schneider A. Cardiovascular risks of climate change. Nat Rev Cardiol. 2021;18:1–2.
Wang Q, Li C, Guo Y, Barnett AG, Tong S, Phung D, et al. Environmental ambient temperature and blood pressure in adults: a systematic review and meta-analysis. Sci Total Environ. 2017;575:276–86.
Kent ST, Howard G, Crosson WL, Prineas RJ, McClure LA. The association of remotely-sensed outdoor temperature with blood pressure levels in REGARDS: a cross-sectional study of a large, national cohort of African-American and white participants. Environ Health. 2011;10:1–12.
Barnett AG, Sans S, Salomaa V, Kuulasmaa K, Dobson AJ, Project ftWM. The effect of temperature on systolic blood pressure. Blood Press Monit. 2007;12:195–203.
Sim JJ, Zhou H, Bhandari S, Wei R, Brettler JW, Tran-Nguyen J, et al. Low systolic blood pressure from treatment and association with serious falls/syncope. Am J Preventive Med. 2018;55:488–96.
Modesti PA. Season, temperature and blood pressure: a complex interaction. Eur J Intern Med. 2013;24:604–7.
Cuspidi C, Ochoa JE, Parati G. Seasonal variations in blood pressure: a complex phenomenon. J Hypertens. 2012;30:1315–20.
Guo Y, Gasparrini A, Armstrong BG, Tawatsupa B, Tobias A, Lavigne E, et al. Temperature variability and mortality: a multi-country study. Environ Health Perspect. 2016;124:1554–9.
Taylor HA, Wilson JG, Jones DW, Sarpong DF, Srinivasan A, Garrison RJ, et al. Toward resolution of cardiovascular health disparities in African Americans. Ethnicity Dis. 2005;15:4–17.
Fuqua SR, Wyatt SB, Andrew ME, Sarpong DF, Henderson FR, Cunningham MF, et al. Recruiting African-American Research Participation in the Jackson Heart Study. Ethnicity Dis. 2005;15:18–29.
Butler MJ, Tanner RM, Muntner P, Shimbo D, Bress AP, Shallcross AJ, et al. Adherence to antihypertensive medications and associations with blood pressure among African Americans with hypertension in the Jackson Heart Study. J Am Soc Hypertens. 2017;11:581–8.e5.
Seals SR, Colantonio LD, Tingle JV, Shimbo D, Correa A, Griswold ME, et al. Calibration of blood pressure measurements in the Jackson Heart Study. Blood Press Monit. 2019;24:130–6.
Thornton MM, Shrestha R, Wei Y, Thornton PE, Kao S-C, Wilson BE. Daymet: Daily Surface Weather Data on a 1-km Grid for North Americ. Oak Ridge, Tennessee, USA: ORNL DAAC; 2022. R1 V, editor.
Fan P, Xue X, Hu J, Qiao Q, Yin T, Yang X, et al. Ambient temperature and ambulatory blood pressure: an hourly–level, longitudinal panel study. Sci Total Environ. 2023;864:160854.
Halonen JI, Zanobetti A, Sparrow D, Vokonas PS, Schwartz J. Relationship between outdoor temperature and blood pressure. Occup Environ Med. 2011;68:296–301.
Alpérovitch A, Lacombe J-M, Hanon O, Dartigues J-F, Ritchie K, Ducimetière P, et al. Relationship between blood pressure and outdoor temperature in a large sample of elderly individuals: the Three-City study. Arch Intern Med. 2009;169:75–80.
Bouchama A, Knochel JP. Heat stroke. N Engl J Med. 2002;346:1978–88.
Narita K, Hoshide S, Kario K. Seasonal variation in day-by-day home blood pressure variability and effect on cardiovascular disease incidence. Hypertension. 2022;79:2062–70.
Watts N, Amann M, Arnell N, Ayeb-Karlsson S, Belesova K, Boykoff M, et al. The 2019 report of The Lancet Countdown on health and climate change: ensuring that the health of a child born today is not defined by a changing climate. Lancet. 2019;394:1836–78.
van Hateren KJ, Kleefstra N, Blanker MH, Ubink-Veltmaat LJ, Groenier KH, Houweling ST, et al. Orthostatic hypotension, diabetes, and falling in older patients: a cross-sectional study. Br J Gen Pract. 2012;62:e696–e702.
Carr D, Falchetta G, Sue Wing I. Population aging and heat exposure in the 21st century: which US regions are at greatest risk and why? Gerontologist. 2024;64:gnad050.
Baniassadi A, Lipsitz LA, Sailor D, Pascual-Leone A, Manor B. Heat Waves, Climate Change, and Implications for an Aging Population. Oxford University Press US; 2023. p. 2304–6.
Chang AY, Tan AX, Nadeau KC, Odden MC. Aging hearts in a hotter, more turbulent world: the impacts of climate change on the cardiovascular health of older adults. Curr Cardiol Rep. 2022;24:749–60.
Khatana SAM, Werner RM, Groeneveld PW. Association of extreme heat with all-cause mortality in the contiguous US, 2008-2017. JAMA Netw Open. 2022;5:e2212957.
Yang L, Li L, Lewington S, Guo Y, Sherliker P, Bian Z, et al. Outdoor temperature, blood pressure, and cardiovascular disease mortality among 23 000 individuals with diagnosed cardiovascular diseases from China. Eur Heart J. 2015;36:1178–85.
Monahan KD. Effect of aging on baroreflex function in humans. Am J Physiol-Regul, Integr Comp Physiol. 2007;293:R3–R12.
Zhu W, Liu Y, Zhang L, Shi G, Zhang X, Wang M, et al. Ambient temperature variability and blood pressure in a prospective cohort of 50,000 Chinese adults. J Hum Hypertens. 2023;37:818–27.
Acknowledgements
AX Tan would like to thank Paul Muntner, PhD for his prior contributions to this project. The authors also wish to thank the staffs and participants of the JHS. A prior version of this abstract was published at the American Heart Association Epi Lifestyle 2024 conference held in March 2024. The abstract is available here: https://www.ahajournals.org/doi/abs/10.1161/circ.149.suppl_1.MP74.
Funding
AX Tan and MC Odden are funded by R01-AG071019. The Jackson Heart Study (JHS) is supported and conducted in collaboration with Jackson State University (HHSN268201800013I), Tougaloo College (HHSN268201800014I), the Mississippi State Department of Health (HHSN268201800015I) and the University of Mississippi Medical Center (HHSN268201800010I, HHSN268201800011I and HHSN268201800012I) contracts from the National Heart, Lung, and Blood Institute (NHLBI) and the National Institute on Minority Health and Health Disparities (NIMHD).
Author information
Authors and Affiliations
Contributions
Annabel X. Tan: Conceptualization, Methodology, Figure preparation, Writing – original draft, Writing – review and editing. Andrew Y. Chang: Writing - review & editing. Daichi Shimbo: Methodology, writing - review & editing. Adam Bress: Writing – review & editing. Mario Sims: Investigation, Resources, Writing – review & editing. Michelle C. Odden: Conceptualization, Methodology, Writing – original draft, review & editing, Supervision, Funding acquisition.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tan, A.X., Chang, A.Y., Shimbo, D. et al. Association of ambient temperature and blood pressure in the Jackson Heart Study. J Hum Hypertens 39, 415–421 (2025). https://doi.org/10.1038/s41371-025-01026-4
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41371-025-01026-4