Abstract
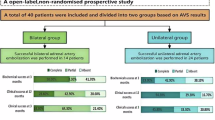
Although unilateral adrenal artery embolization (AAE) has emerged as an alternative treatment for patients with primary aldosteronism (PA), it may be insufficient for treating patients with idiopathic hyperaldosteronism (IHA) due to the bilateral nature of their condition. This study aimed to investigate the safety and efficacy of alcohol-mediated bilateral adrenal artery embolization (Bi-AAE) in patients with idiopathic hyperaldosteronism (IHA). A total of 72 patients were randomly assigned in a (1:1) ratio to receive either Bi-AAE or spironolactone (20–60 mg/day). The primary endpoint was the change in office systolic blood pressure (SBP) from baseline to 6 months. Key secondary endpoints included changes in 24 h blood pressure, aldosterone levels, aldosterone-to-renin ratio (ARR), and serum potassium. At 6 months, Bi-AAE significantly reduced office SBP compared to spironolactone (−18.9 ± 16.4 mmHg vs. −11.6 ± 9.3 mmHg; treatment difference: −7.4 mmHg; P = 0.03), with a greater proportion of Bi-AAE patients achieving target SBP (<140 mmHg; 77.1% vs. 51.5%; P = 0.027). Bi-AAE also resulted in significantly greater reductions in 24 h and home SBP at 1, 3, and 6 months (all P < 0.05). Furthermore, Bi-AAE was more effective in correcting biochemical abnormalities, including hyperaldosteronism and renin suppression (all P < 0.05). Importantly, Bi-AAE preserved zona fasciculata function, as evidenced by normal morning serum cortisol levels and intact responses to ACTH stimulation post-procedure. No serious adverse events occurred during the perioperative or 6-month follow-up period. These findings support Bi-AAE as a safe, minimally invasive, and highly effective alternative to medical therapy for managing IHA. Although the findings support Bi-AAE as a safe, minimally invasive, and highly effective alternative to medical therapy for managing IHA, the need for long-term data before drawing definitive conclusions is emphasized. Future studies with extended follow-up are necessary to confirm its long-term benefits and risks. Trial registration: The trial has been registered at ClinicalTrials.gov (NCT05262660).

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
Data availability
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
References
Pilz S, Grübler MR, Theiler-Schwetz V, Malle O, Trummer C. The unrecognized prevalence of primary aldosteronism. Ann Intern Med. 2020;173:681–2.
Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, et al. The management of primary aldosteronism: case detection, diagnosis, and treatment: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2016;101:1889–916.
Tetti M, Brüdgam D, Burrello J, Udager AM, Riester A, Knösel T, et al. Unilateral primary aldosteronism: long-term disease recurrence after adrenalectomy. Hypertension. 2024;81:936–45.
Tang F, Loh LM, Foo RS, Loh WJ, Lim DST, Zhang M, et al. Tolerability and efficacy of long-term medical therapy in primary aldosteronism. J Endocr Soc. 2021;5:bvab144.
Hundemer GL, Leung AA, Kline GA, Brown JM, Turcu AF, Vaidya A. Biomarkers to guide medical therapy in primary aldosteronism. Endocr Rev. 2024;45:69–94.
Fowler AM, Burda JF, Kim SK. Adrenal artery embolization: anatomy, indications, and technical considerations. AJR Am J Roentgenol. 2013;201:190–201.
Hokotate H, Inoue H, Baba Y, Tsuchimochi S, Nakajo M. Aldosteronomas: experience with superselective adrenal arterial embolization in 33 cases. Radiology. 2003;227:401–6.
Dong H, Zou Y, He J, Deng Y, Chen Y, Song L, et al. Superselective adrenal arterial embolization for idiopathic hyperaldosteronism: 12-month results from a proof-of-principle trial. Catheter Cardiovasc Interv. 2021:976–81. https://doi.org/10.1002/ccd.29554.
Zhang H, Li Q, Liu X, Zhao Z, He H, Sun F, et al. Adrenal artery ablation for primary aldosteronism without apparent aldosteronoma: an efficacy and safety, proof-of-principle trial. J Clin Hypertens. 2020;22:1618–26.
Zhou Y, Wang X, Hou J, Wan J, Yang Y, Liu S, et al. A controlled trial of percutaneous adrenal arterial embolization for hypertension in patients with idiopathic hyperaldosteronism. Hypertens Res. 2024;47:311–21.
Wang J, Yin Y, Lu C, Lu Z, Hu J, Wang Y, et al. Efficacy and safety of sympathetic mapping and ablation of renal nerves for the treatment of hypertension (SMART): 6-month follow-up of a randomised, controlled trial. EClinicalMedicine. 2024;72:102626.
Rossi GP, Maiolino G, Seccia TM. Adrenal venous sampling: where do we stand? Endocrinol Metab Clin North Am. 2019;48:843–58.
Zhou Y, Liu Q, Wang X, Wan J, Liu S, Luo T, et al. Adrenal ablation versus mineralocorticoid receptor antagonism for the treatment of primary aldosteronism: a single-center prospective cohort study. Am J Hypertens. 2022;35:1014–23.
Bornstein SR, Allolio B, Arlt W, Barthel A, Don-Wauchope A, Hammer GD, et al. Diagnosis and treatment of primary adrenal insufficiency: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2016;101:364–89.
Alpert B, McCrindle B, Daniels S, Dennison B, Hayman L, Jacobson M, et al. Recommendations for blood pressure measurement in human and experimental animals; part 1: blood pressure measurement in humans. Hypertension. 2006;48:e3.
JCS Joint Working Group. Guidelines for the clinical use of 24 h ambulatory blood pressure monitoring (ABPM) (JCS 2010). Circ J. 2012;76:508–19.
Park SS, Ahn CH, Kim SW, Koh JM, Lee SH, Kim JH. Temporal trends in clinical features of patients with primary aldosteronism over 20 years. Hypertens Res. 2024;47:2019–28.
Samnani S, Cenzer I, Kline GA, Lee SJ, Hundemer GL, McClurg C, et al. Time to benefit of surgery vs targeted medical therapy for patients with primary aldosteronism: a meta-analysis. J Clin Endocrinol Metab. 2024;109:e1280–89.
Meng Z, Dai Z, Huang K, Xu C, Zhang YG, Zheng H, et al. Long-term mortality for patients of primary aldosteronism compared with essential hypertension: a systematic review and meta-analysis. Front Endocrinol. 2020;11:121.
Inoue K, Naito T, Fuji R, Sonehara K, Yamamoto K, Baba R, et al. Primary aldosteronism and risk of cardiovascular outcomes: genome-wide association and mendelian randomization study. J Am Heart Assoc. 2024;13:e034180.
Lu YC, Liu KL, Wu VC, Wang SM, Lin YH, Chueh SJ, et al. Unilateral adrenalectomy in bilateral adrenal hyperplasia with primary aldosteronism. J Formos Med Assoc. 2023;122:393–9.
Williams TA, Gong S, Tsurutani Y, Tezuka Y, Thuzar M, Burrello J, et al. Adrenal surgery for bilateral primary aldosteronism: an international retrospective cohort study. Lancet Diabetes Endocrinol. 2022;10:769–71.
Szabo YT, Shariq OA, Foster TR, Lyden ML, Dy BM, Young WF Jr., et al. Unilateral adrenalectomy for primary aldosteronism due to bilateral adrenal disease can result in resolution of hypokalemia and amelioration of hypertension. World J Surg. 2023;47:314–8.
Pinto D, Parameswaran R. Adrenal insufficiency post unilateral adrenalectomy in non-cortisol secreting tumours. Gland Surg. 2023;12:1328–31.
Verma S, Pandey A, Pandey AK, Butler J, Lee JS, Teoh H, et al. Aldosterone and aldosterone synthase inhibitors in cardiorenal disease. Am J Physiol Heart Circ Physiol. 2024;326:H670–h688.
Mulatero P, Wuerzner G, Groessl M, Sconfienza E, Damianaki A, Forestiero V, et al. Safety and efficacy of once-daily dexfadrostat phosphate in patients with primary aldosteronism: a randomised, parallel group, multicentre, phase 2 trial. EClinicalMedicine. 2024;71:102576.
Inoue H, Nakajo M, Miyazono N, Kanetsuki I, Miyake S, Hokotate H, et al. Treatment of aldosteronoma with superselective intraarterial injection of absolute ethanol. Nihon Igaku Hoshasen Gakkai Zasshi. 1994;54:154–62.
Kometani M, Yoneda T, Demura M, Karashima S, Mori S, Oe M, et al. The long-term effect of adrenal arterial embolization for unilateral primary aldosteronism on cardiorenovascular protection, blood pressure, and the endocrinological profile. Intern Med. 2016;55:769–73.
Acknowledgements
None.
Funding
This work was supported by grants from Key Project of Sichuan Natural Science Foundation (No.2024NSFSC0051), National Natural Science Foundation of China (No. 82300333), the CMC Excellent-talent Program (No. 2024kjTzn05), Central Funds Guiding the Local Science and Technology Development of Sichuan Province (No. 2024ZYD0148), Innovation Team Project of Sichuan Provincial Health Commission (No. 24CXTD01), National Key Clinical Specialties Construction (No. 2024GXNKG002), and Sichuan Science and Technology Program (No.24PYXM0578).
Author information
Authors and Affiliations
Contributions
YZ, SL, and GJ contributed equally to the study design, data analysis, and interpretation of the results. CY, LZ, and TL were responsible for patient recruitment and management. FH and ZC provided technical support for the Bi-AAE procedures. HX and PW supervised the study, ensured data integrity, and provided critical revisions to the manuscript. All authors reviewed and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was approved by the First Affiliated Hospital of Chengdu Medical College Ethics Committee. Informed consent was obtained from all participants.
Consent for publication
Consent for publication was obtained from all participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhou, Y., Liu, S., Ji, G. et al. Safety and efficacy of alcohol-mediated bilateral adrenal artery embolization in patients with idiopathic hyperaldosteronism: a 6-month follow-up of a randomized controlled trial. J Hum Hypertens 39, 489–499 (2025). https://doi.org/10.1038/s41371-025-01032-6
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41371-025-01032-6