Abstract
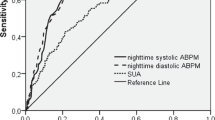
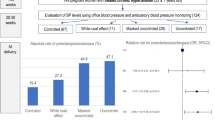
To investigate the relationship between blood pressure (BP) components (daytime vs. nocturnal BP and systolic vs. diastolic BP) and preeclampsia (PE) across gestational stages. We conducted a historical cohort study involving 1363 high-risk pregnant women (mean age, 30 ± 7 years). Ambulatory BP monitoring (ABPM) was performed at 12–19 weeks (n = 389), 20–27 weeks (n = 798), and 28–36 weeks (n = 1176); 59.9, 25.0, and 15.1% of the participants underwent one, two, and three ABPM evaluations, respectively. PE occurred in 15.4, 18.9, and 20.2% of the women evaluated at 12–19, 20–27, and 28–36 weeks, respectively. In the second half of pregnancy, sustained (daytime and nighttime) and isolated nocturnal hypertension were strong predictors of PE. Conversely, before the 20th week of gestation, only sustained hypertension (but not isolated nocturnal hypertension) increased PE risk, with lower odds ratios (ORs). Moreover, the areas under the curve (AUCs) for all ABPM components increased markedly after the 20th week of gestation. In late pregnancy, systolic and diastolic ABPM levels as well as all forms of nocturnal hypertension (isolated systolic, isolated diastolic, and combined systodiastolic) were significantly associated with PE risk, with ORs remaining significant after adjusting for daytime ABPM and maternal covariates. Patients with systodiastolic nocturnal hypertension had the highest risk. Conversely, neither daytime hypertension nor daytime ABPM levels remained statistically significant after adjusting for nocturnal ABPM levels. In conclusion, the association between PE and systolic, diastolic, and systodiastolic nocturnal hypertension emerges in the second half of pregnancy, suggesting a relationship with abnormal placentation.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Data of this study are available from the corresponding author on reasonable request.
References
Magee LA, Brown MA, Hall DR, Gupte S, Hennessy A, Karumanchi SA, et al. The 2021 International Society for the study of hypertension in pregnancy classification, diagnosis & management recommendations for international practice. Pregnancy Hypertens. 2022;27:148–69.
Salazar MR, Espeche WG, Leiva Sisnieguez BC, Balbín E, Leiva Sisnieguez CE, Stavile RN, et al. Significance of masked and nocturnal hypertension in normotensive women coursing a high-risk pregnancy. J Hypertens. 2016;34:2248–52.
Salazar MR, Espeche WG, Leiva Sisnieguez CE, Juliano PL, Vulcano MV, Sanchez Caro L, et al. Masked hypertension and neonatal outcome in high-risk pregnancies. J Hum Hypertens. 2023;37:36–41.
Scott G, Gillon TE, Pels A, von Dadelszen P, Magee LA. Guidelines-similarities and dissimilarities: a systematic review of international clinical practice guidelines for pregnancy hypertension. Am J Obstet Gynecol. 2022;226:S1222–36.
Sugulle M, Fiskå BS, Jacobsen DP, Fjeldstad HE, Staff AC. Placental senescence and the two-stage model of preeclampsia. Am J Reprod Immunol. 2024;92:e13904.
Oney T, Meyer-Sabellek W. Variability of arterial blood pressure in normal and hypertensive pregnancy. J Hypertens Suppl. 1990;8:77–81.
Ayala DE, Hermida RC, Mojon A, Fernandez JR, Iglesias M. Circadian blood pressure variability in healthy and complicated pregnancies. Hypertension. 1997;30:603–10.
Bouchlariotou S, Liakopoulos V, Dovas S, Giannopoulou M, Kiropoulos T, Zarogiannis S, et al. Nocturnal hypertension is associated with an exacerbation of the endothelial damage in preeclampsia. Am J Nephrol. 2008;28:424–30.
Salazar MR, Espeche WG, Leiva Sisnieguez CE, Minetto J, Balbín E, Soria A, et al. Nocturnal hypertension and risk of developing early-onset preeclampsia in high-risk pregnancies. Hypertens Res. 2021;44:1633–40.
O’Brien E, Mee F, Atkins N, Halligan A, O’Malley K. Accuracy of the SpaceLabs 90207 ambulatory blood pressure measuring system in normotensive pregnant women determined by the British Hypertension Society protocol. J Hypertens Suppl. 1993;11:S282–3.
Shennan AH, Kissane J, de Swiet M. Validation of the SpaceLabs 90207 ambulatory blood pressure monitor for use in pregnancy. Br J Obstet Gynaecol. 1993;100:904–8.
Natarajan P, Shennan AH, Penny J, Halligan AW, de Swiet M, Anthony J. Comparison of auscultatory and oscillometric automated blood pressure monitors in the setting of preeclampsia. Am J Obstet Gynecol. 1999;181:1203–10.
Mancia G, Kreutz R, Brunström M, Burnier M, Grassi G, Januszewicz A, et al. 2023 ESH guidelines for the management of arterial hypertension the task force for the management of arterial hypertension of the European Society of Hypertension: endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA). J Hypertens. 2023;41:1874–2071. https://doi.org/10.1097/HJH.0000000000003480
Kim JH. Multicollinearity and misleading statistical results. Korean J Anesthesiol. 2019;72:558–69.
The jamovi project. jamovi (Version 2.3) [Computer Software]. 2022. https://www.jamovi.org.
R Core Team. R: a language and environment for statistical computing (Version 4.1) [Computer software]. R packages retrieved from MRAN snapshot. 2021. https://cran.r-project.org Accessed 1 Jan 2022.
Redman CW, Beilin LJ, Bonnar J. Reversed daytime blood pressure rhythm in hypertensive pregnancies. Clin Sci Mol Med Suppl. 1976;3:687s–9s.
Brown MA, Davis GK, McHugh L. The prevalence and clinical significance of nocturnal hypertension in pregnancy. J Hypertens. 2001;19:1437–44.
Redman CW. Current topic: pre-eclampsia and the placenta. Placenta. 1991;12:301–8. https://doi.org/10.1016/0143-4004(91)90339-h
Maynard S, Epstein FH, Karumanchi SA. Preeclampsia and angiogenic imbalance. Annual review of medicine. 2008;59:61–78.
Flint AC, Conell C, Ren X, Banki NM, Chan SL, Rao VA, et al. Effect of systolic and diastolic blood pressure on cardiovascular outcomes. N Engl J Med. 2019;381:243–51. https://doi.org/10.1056/NEJMoa1803180
Li Y, Wei FF, Thijs L, Boggia J, Asayama K, Hansen TW, et al. International Database on Ambulatory blood pressure in relation to Cardiovascular Outcomes (IDACO) investigators. ambulatory hypertension subtypes and 24-h systolic and diastolic blood pressure as distinct outcome predictors in 8341 untreated people recruited from 12 populations. Circulation. 2014;130:466–74. https://doi.org/10.1161/CIRCULATIONAHA.113.004876
de la Sierra A, Ruilope LM, Staplin N, Stergiou GS, Williams B. Mortality risks in different subtypes of masked hypertension in the Spanish ambulatory blood pressure monitoring registry. J Hypertens. 2025;43:642–8. https://doi.org/10.1097/HJH.0000000000003950
Lv LJ, Ji WJ, Wu LL, Miao J, Wen JY, Lei Q, et al. Thresholds for ambulatory blood pressure monitoring based on maternal and neonatal outcomes in late pregnancy in a southern Chinese population. J Am Heart Assoc. 2019;8:e012027.
Funding
This research did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
MS, WE, and JM conceived and designed the study, performed the statistical analysis, interpreted the results, and drafted and revised the manuscript. JM, GC, JT, LR, and RR acquired and analyzed the ABPM data and supervised blood pressure treatment. ST, FG, CS, and RT collected obstetric data, identified high-risk pregnancies, and defined the timing of delivery. HC contributed to the study conception and design and approved the final version of the manuscript. This work has not been published previously, either in whole or in part. All authors have reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
The CMDU protocol for ABPM evaluation during pregnancy was approved by the Medical Bioethics Committee of the Faculty of Medical Sciences, National University of La Plata (UNLP), Buenos Aires, Argentina (COBIMED 0/27). This observational study posed no risk to participants and was conducted in accordance with the Declaration of Helsinki.
Conflict of interest
The authors declare that they have no affiliations with or involvement in any organization or entity with any financial interest in the subject matter or materials discussed in this manuscript.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Salazar, M.R., Espeche, W.G., Minetto, J. et al. Nocturnal systolic and diastolic blood pressure across gestational periods and the risk of preeclampsia. J Hum Hypertens 39, 541–548 (2025). https://doi.org/10.1038/s41371-025-01046-0
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41371-025-01046-0
This article is cited by
-
JHH Young Investigator Award 2025: Interview with the winner Julian Minetto
Journal of Human Hypertension (2026)