Abstract
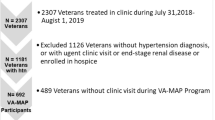
Neighborhood characteristics may influence patient and clinician management of blood pressure (BP) control. This study examined the association of the Area Deprivation Index (ADI) with uncontrolled BP ( ≥ 140/90 mmHg) at primary care visits and therapeutic inertia (TI) during visits with uncontrolled BP. Data included 52 750 visits among 8 434 patients aged ≥65 years across nine outpatient clinics in Chicago suburbs between January 1, 2017, and March 10, 2020. ADI represents national percentiles of census block group deprivation (0 = least, 100 = most deprived). TI was defined as no initiation or escalation of BP-lowering medication during visits with uncontrolled BP. Adjusted prevalence ratios (PRs) of uncontrolled BP and TI by ADI quartiles were estimated using generalized estimating equations. Mean age was 74.3 years (SD 7.8), 42.3% were male, 69.1% Non-Hispanic (NH) White, 15.9% NH Black, and 8.2% Hispanic. Uncontrolled BP occurred in 33.8% of visits. Of those, 73.4% experienced TI. There was no significant association between ADI and uncontrolled BP in adjusted models. Adjusted PRs of TI were higher in ADI Q2 (PR 1.03, 95% CI: 1.00-1.06) and Q3 (PR 1.04 (95% CI: 1.01-1.07), but not Q4 compared to Q1. ADI modeled continuously with splines showed modest increases in adjusted predicted prevalence of both outcomes, although confidence intervals widened at the extremes. Neighborhood deprivation may contribute to disparities in hypertension management but more studies with larger number of patient visits at the extremes of ADI distribution are needed.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to institutional policies and patient privacy protections but are available from the corresponding author upon reasonable request and with permission of the Loyola University Chicago Institutional Review Board.
References
Tsao CW, Aday AW, Almarzooq ZI, Anderson CAM, Arora P, Avery CL, et al. Heart Disease and Stroke Statistics-2023 Update: A Report From the American Heart Association. Circulation. 2023;147:e93–e621.
Phillips LS, Branch WT, Cook CB, Doyle JP, El-Kebbi IM, Gallina DL, et al. Clinical inertia. Ann Intern Med. 2001;135:825–34.
Hiura GT, Markossian TW, Probst BD, Tootooni MS, Wozniak G, Rakotz M, et al. Age and Comorbidities Are Associated With Therapeutic Inertia Among Older Adults With Uncontrolled Blood Pressure. Am J Hypertens. 2024;37:280–9.
Mu L, Mukamal KJ. Treatment Intensification for Hypertension in US Ambulatory Medical Care. J Am Heart Assoc. 2016;5.
Ali DH, Kilic B, Hart HE, Bots ML, Biermans MCJ, Spiering W, et al. Therapeutic inertia in the management of hypertension in primary care. J Hypertens. 2021;39:1238–45.
Faria C, Wenzel M, Lee KW, Coderre K, Nichols J, Belletti DA. A narrative review of clinical inertia: focus on hypertension. J Am Soc Hypertens. 2009;3:267–76.
Kershaw KN, Magnani JW, Diez Roux AV, Camacho-Rivera M, Jackson EA, Johnson AE, et al. Neighborhoods and Cardiovascular Health: A Scientific Statement From the American Heart Association. Circ Cardiovasc Qual Outcomes. 2024;17:e000124.
Arlington, VA: National Coalition on Aging; 2024 [Available from: https://www.ncoa.org/article/older-adult-poverty-continues-upward-trend-reaching-an-unacceptable-14-percent.
Pearson J, Jacobson C, Ugochukwu N, Asare E, Kan K, Pace N, et al. Geospatial analysis of patients’ social determinants of health for health systems science and disparity research. Int Anesthesiol Clin. 2023;61:49–62.
Commodore-Mensah Y, Turkson-Ocran RA, Foti K, Cooper LA, Himmelfarb CD. Associations Between Social Determinants and Hypertension, Stage 2 Hypertension, and Controlled Blood Pressure Among Men and Women in the United States. Am J Hypertens. 2021;34:707–17.
Vintimilla R, Seyedahmadi A, Hall J, Johnson L, O’Bryant S. Team H-HS. Association of Area Deprivation Index and hypertension, diabetes, dyslipidemia, and Obesity: A Cross-Sectional Study of the HABS-HD Cohort. Gerontol Geriatr Med. 2023;9:23337214231182240.
Xu J, Lawrence KG, O’Brien KM, Jackson CL, Sandler DP. Association between neighbourhood deprivation and hypertension in a US-wide Cohort. J Epidemiol Community Health. 2022;76:268–73.
McDoom MM, Palta P, Vart P, Juraschek SP, Kucharska-Newton A, Diez Roux AV, et al. Late life socioeconomic status and hypertension in an aging cohort: the Atherosclerosis Risk in Communities Study. J Hypertens. 2018;36:1382–90.
Claudel SE, Adu-Brimpong J, Banks A, Ayers C, Albert MA, Das SR, et al. Association between neighborhood-level socioeconomic deprivation and incident hypertension: A longitudinal analysis of data from the Dallas heart study. Am Heart J. 2018;204:109–18.
Muntner P, Shimbo D, Carey RM, Charleston JB, Gaillard T, Misra S, et al. Measurement of Blood Pressure in Humans: A Scientific Statement From the American Heart Association. Hypertension. 2019;73:e35–e66.
Brokamp C, Wolfe C, Lingren T, Harley J, Ryan P. Decentralized and reproducible geocoding and characterization of community and environmental exposures for multisite studies. J Am Med Inform Assoc. 2018;25:309–14.
Kind AJH, Buckingham WR. Making Neighborhood-Disadvantage Metrics Accessible - The Neighborhood Atlas. N Engl J Med. 2018;378:2456–8.
Kind AJH BWAUoWSoMaPH. 2015 Area Deprivation Index v2.0.: University of Wisconsin School of Medicine and Public Health; 2018 [Available from: https://www.neighborhoodatlas.medicine.wisc.edu/.
Højsgaard S, Halekoh U, Yan J. The R Package geepack for Generalized Estimating Equations. Journal of Statistical Software. 2006;15:1–11.
Buys DR, Howard VJ, McClure LA, Buys KC, Sawyer P, Allman RM, et al. Association between neighborhood disadvantage and hypertension prevalence, awareness, treatment, and control in older adults: results from the University of Alabama at Birmingham Study of Aging. Am J Public Health. 2015;105:1181–8.
Cho KH, Lee SG, Nam CM, Lee EJ, Jang SY, Lee SH, et al. Disparities in socioeconomic status and neighborhood characteristics affect all-cause mortality in patients with newly diagnosed hypertension in Korea: a nationwide cohort study, 2002-2013. Int J Equity Health. 2016;15:3.
Chandrabose M, Rachele JN, Gunn L, Kavanagh A, Owen N, Turrell G, et al. Built environment and cardio-metabolic health: systematic review and meta-analysis of longitudinal studies. Obes Rev. 2019;20:41–54.
Mujahid MS, Diez Roux AV, Morenoff JD, Raghunathan TE, Cooper RS, Ni H, et al. Neighborhood characteristics and hypertension. Epidemiology. 2008;19:590–8.
Jimenez MP, Wellenius GA, Subramanian SV, Buka S, Eaton C, Gilman SE, et al. Longitudinal associations of neighborhood socioeconomic status with cardiovascular risk factors: A 46-year follow-up study. Soc Sci Med. 2019;241:112574.
Makhlouf MHE, Motairek I, Chen Z, Nasir K, Deo SV, Rajagopalan S, et al. Neighborhood Walkability and Cardiovascular Risk in the United States. Curr Probl Cardiol. 2023;48:101533.
Diez Roux AV, Chambless L, Merkin SS, Arnett D, Eigenbrodt M, Nieto FJ, et al. Socioeconomic disadvantage and change in blood pressure associated with aging. Circulation. 2002;106:703–10.
Muntner P, Hardy ST, Fine LJ, Jaeger BC, Wozniak G, Levitan EB, et al. Trends in Blood Pressure Control Among US Adults With Hypertension, 1999-2000 to 2017-2018. JAMA. 2020;324:1190–200.
Akinyelure OP, Jaeger BC, Oparil S, Carson AP, Safford MM, Howard G, et al. Social Determinants of Health and Uncontrolled Blood Pressure in a National Cohort of Black and White US Adults: the REGARDS Study. Hypertension. 2023;80:1403–13.
Freund DMP. Colored Property: State policy and white racial politics in suburban America. Chicago, IL: University of Chicago; 2007.
Lenoir KM, Paul R, Wright E, Palakshappa D, Pajewski NM, Hanchate A, et al. The Association of Frailty and Neighborhood Disadvantage with Emergency Department Visits and Hospitalizations in Older Adults. J Gen Intern Med. 2024;39:643–51.
Abdalla M, Bolen SD, Brettler J, Egan BM, Ferdinand KC, Ford CD, et al. Implementation Strategies to Improve Blood Pressure Control in the United States: A Scientific Statement From the American Heart Association and American Medical Association. Hypertension. 2023;80:e143–e57.
Moss JL, Johnson NJ, Yu M, Altekruse SF, Cronin KA. Comparisons of individual- and area-level socioeconomic status as proxies for individual-level measures: evidence from the Mortality Disparities in American Communities study. Popul Health Metr. 2021;19:1.
Petterson S. Deciphering the Neighborhood Atlas Area Deprivation Index: the consequences of not standardizing. Health affairs scholar. 2023;1:qxad063.
Hannan EL, Wu Y, Cozzens K, Anderson B. The neighborhood atlas area deprivation index for measuring socioeconomic status: an overemphasis on home value: study examines the neighborhood atlas area deprivation index as a tool to measure socioeconomic status. Health Affairs. 2023;42:702–9.
Rothbaum J, Eggleston J, Bee A, Klee M, Mendez-Smith B. Addressing nonresponse bias in the american community survey during the pandemic using administrative data. American Community Survey Research and Evaluation Report Memorandum Series ACS21-RER-05, US Census Bureau, Washington. 2021.
Acknowledgements
None
Funding
Loyola University Chicago Center for Health Outcomes and Informatics Research.
Author information
Authors and Affiliations
Contributions
All authors meet the ICMJE authorship criteria. Conceptualization: HK, ST, TWM. Methodology: MTS, ST, AW, HK. Data curation: GTH. Formal analysis: MTS, AW. Visualization: MTS. Investigation/Resources: MTS, BP, TM, HK. Writing – original draft: MTS. Writing – review & editing: All authors. Supervision: HK, ST, TWM.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was reviewed by the Loyola University Chicago Institutional Review Board and deemed exempt from human subjects review. All methods were carried out in accordance with relevant guidelines and regulations. Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Saban, M.T., Tootooni, S., Markossian, T.W. et al. The association of area deprivation index and blood pressure control and therapeutic inertia among older adults with hypertension. J Hum Hypertens 39, 748–754 (2025). https://doi.org/10.1038/s41371-025-01067-9
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41371-025-01067-9