Abstract
Objectives
To conduct a systematic review of clinical trials comparing automated versus manual fraction of inspired oxygen (FiO2) control to target oxygen saturation (SpO2) in preterm infants.
Design
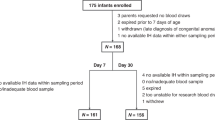
The authors searched MEDLINE, Embase, CENTRAL, and CINAHL from inception upto December 2016, reviewed conference proceedings and sought results of unpublished trials. Studies were included if automated FiO2 control was compared to manual control in preterm infants on positive pressure respiratory support. The primary outcome was percentage of time spent within the target SpO2 range. Summary mean differences (MD) were computed using random effects model.
Results
Out of 276 identified studies 10 met the inclusion criteria. Automated FiO2 control significantly improved time being spent within the target SpO2 range [MD: 12.8%; 95% CI: 6.5–19.2%; I2 = 90%]. Periods of hyperoxia (MD:–8.8%; 95% CI: –15 to –2.7%), severe hypoxia(SpO2 < 80%)(MD: –0.9%;95%CI: –1.5 to –0.4%) and hypoxic events (MD: –5.6%; 95% CI: –9.1 to –2.1%) were significantly reduced with automated control.
Conclusion
Automated FiO2 adjustment provides significant improvement of time in target saturations, reduces periods of hyperoxia, and severe hypoxia in preterm infants on positive pressure respiratory support.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Cristea AI, Carroll AE, Davis SD, Swigonski NL, Ackerman VL. Outcomes of children with severe bronchopulmonary dysplasia who were ventilator dependent at home. Pediatrics. 2013;132:727–34.
Claure N, Bancalari E. Automated respiratory support in newborn infants. Semin Fetal Neonatal Med. 2009;14:35–41.
Bancalari E, Claure N. Control of oxygenation during mechanical ventilation in the premature infant. Clin Perinatol. 2012;39:563–72.
Claure N, Bancalari E. Automated closed loop control of inspired oxygen concentration. Respir Care. 2013;58:151–61.
Van Zanten HA, Tan RNGB, van den Hoogen A, Lopriore E, te Pas AB. Compliance in oxygen saturation targeting in preterm infants: a systematic review. Eur J Pediatr. 2015;174:1561–72.
Hummler H, Fuchs H, Schmid M. Automated adjustments of inspired fraction of oxygen to avoid hypoxemia and hyperoxemia in neonates—a systematic review on clinical studies. Klin Padiatr. 2014;226:204–10.
Poets CF, Franz AR. Automated FiO2 control: nice to have, or an essential addition to neonatal intensive care? Arch Dis Child Fetal Neonatal Ed. 2017;102:5–6.
Higgins JPT, Altman DG, Sterne JAC (editors). Assessing risk of bias in included studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.handbook.cochrane.org.
Ding H, Hu GL, Zheng XY, Chen Q, Threapleton DE, Zhou ZH. The method quality of cross-over studies involved in Cochrane Systematic Reviews. PLoS ONE. 2015;10:e0120519.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction—GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64:383–94.
GRADEpro GDT: GRADEpro Guideline Development Tool [Software]. McMaster University, 2015 (developed by Evidence Prime, Inc.). Available from gradepro.org.
Claure N, D’Ugard C, Bancalari E. Automated adjustment of inspired oxygen in preterm infants with frequent fluctuations in oxygenation: a pilot clinical trial. J Pediatr. 2009;155:640–5.
Claure N, Gerhardt T, Everett R, Musante G, Herrera C, Bancalari E. Closed-loop controlled inspired oxygen concentration for mechanically ventilated very low birth weight infants with frequent episodes of hypoxemia. Pediatrics. 2001;107:1120–4.
Hallenberger A, Poets CF, Horn W, Seyfang A, Urschitz MS, CLAC Study Group. Closed-loop automatic oxygen control (CLAC) in preterm infants: a randomized controlled trial. Pediatrics. 2014;133:379–85.
Urschitz MS, Horn W, Seyfang A, Hallenberger A, Herberts T, Miksch S, et al. Automatic control of the inspired oxygen fraction in preterm infants: a randomized crossover trial. Am J Respir Crit Care Med. 2004;170:1095–100.
Lal M, Tin W, Sinha S. Automated control of inspired oxygen in ventilated preterm infants: crossover physiological study. Acta Paediatr. 2015;104:1084–9.
Claure N, Bancalari E, D’Ugard C, Nelin L, Stein M, Ramanathan R, et al. Multicenter crossover study of automated control of inspired oxygen in ventilated preterm infants. Pediatrics. 2011;127:76–83.
van Kaam AH, Hummler HD, Wilinska M, Swietlinski J, Lal MK, te Pas AB, et al. Automated versus manual oxygen control with different saturation targets and modes of respiratory support in preterm infants. J Pediatr. 2015;167:545–50.
Waitz M, Schmid MB, Fuchs H, Mendler MR, Dreyhaupt J, Hummler HD. Effects of automated adjustment of the inspired oxygen on fluctuations of arterial and regional cerebral tissue oxygenation in preterm infants with frequent desaturations. J Pediatr. 2015;166:240–4. e1
Zapata J, Gómez JJ, Araque Campo R, Matiz Rubio A, Sola A. A randomized controlled trial of an automated oxygen delivery algorithm for preterm neonates receiving supplemental oxygen without mechanical ventilation. Acta Paediatr. 2014;103:928–33.
Plottier GK, Wheeler KI, Ali SK, Fathabadi OS, Jayakar R, Gale TJ, et al. Clinical evaluation of a novel adaptive algorithm for automated control of oxygen therapy in preterm infants on non-invasive respiratory support. Arch Dis Child Fetal Neonatal Ed. 2017;102:37–43.
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13.
SUPPORT Study Group of the Eunice Kennedy Shriver NICHD Neonatal Research Network, Carlo WA, Finer NN, Walsh MC, Rich W, Gantz MG, Laptook AR, et al. Target ranges of oxygen saturation in extremely preterm infants. N Engl J Med. 2010;362:1959–69.
BOOST II United Kingdom Collaborative Group, BOOST II Australia Collaborative Group, BOOST II New Zealand Collaborative Group, Stenson BJ, Tarnow-Mordi WO, Darlow BA, Simes J, Juszczak E, Askie L, et al. Oxygen saturation and outcomes in preterm infants. N Engl J Med. 2013;368:2094–104.
Schmidt B, Whyte RK, Asztalos EV, Moddemann D, Poets C, Rabi Y, et al. Effects of targeting higher vs lower arterial oxygen saturations on death or disability in extremely preterm infants: a randomized clinical trial. JAMA. 2013;309:2111–20.
Manja V, Saugstad OD, Lakshminrusimha S. Oxygen saturation targets in preterm infants and outcomes at 18-24 months: a systematic review. Pediatrics. 2017;139:e20161609.
Oxygen in the Delivery Room: Evidence from Systematic Reviews. (n.d.). https://media.vtoxford.org/multimedia/Cochrane/03102017/index.htm. Accessed 10 April 2017.
Askie LM, Henderson-Smart DJ, Irwig L, Simpson JM. Oxygen-saturation targets and outcomes in extremely preterm infants. N Engl J Med. 2003;349:959–67.
Vento M, Moro M, Escrig R, Arruza L, Villar G, Izquierdo I, et al. Preterm resuscitation with low oxygen causes less oxidative stress, inflammation, and chronic lung disease. Pediatrics. 2009;124:439–49.
Poets CF, Roberts RS, Schmidt B, Whyte RK, Asztalos EV, Bader D, et al. Association between intermittent hypoxemia or bradycardia and late death or disability in extremely preterm infants. JAMA. 2015;314:595–603.
Poets CF, Franz AR. Automated FiO2 control: nice to have, or an essential addition to neonatal intensive care? Arch Dis Child Fetal Neonatal Ed. 2017;102:5–6.
Acknowledgements
The authors would like to thank Dr P Dargaville, Associate Professor of Pediatrics and Child Health, University of Tasmania, Australia for providing additional information on unpublished research work which was subsequently published during the course of the systematic review. The authors would also like to thank Darlene Chapman, librarian, IWK Health Sciences Library, Halifax, NS, Canada for providing expert help in building the electronic search strategy.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Mitra, S., Singh, B., El-Naggar, W. et al. Automated versus manual control of inspired oxygen to target oxygen saturation in preterm infants: a systematic review and meta-analysis. J Perinatol 38, 351–360 (2018). https://doi.org/10.1038/s41372-017-0037-z
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-017-0037-z
This article is cited by
-
Pulse oximetry signal loss during hypoxic episodes in preterm infants receiving automated oxygen control
European Journal of Pediatrics (2024)
-
Occurrence of hyperoxia during iNO treatment for persistent pulmonary hypertension of the newborn: a cohort study
European Journal of Pediatrics (2024)
-
Statistical analysis plan for the FiO2-C trial: effects of closed-loop automatic control of the inspiratory fraction of oxygen (FiO2-C) on outcomes of extremely preterm infants—a randomized-controlled parallel group multicentre trial for safety and efficacy
Trials (2024)
-
Does closed-loop automated oxygen control reduce the duration of supplementary oxygen treatment and the amount of time spent in hyperoxia? A randomised controlled trial in ventilated infants born at or near term
Trials (2023)
-
Frequency and duration of extreme hypoxemic and hyperoxemic episodes during manual and automatic oxygen control in preterm infants: a retrospective cohort analysis from randomized studies
BMC Pediatrics (2022)