Abstract
Objectives
We assessed birth hospital level and neonatal outcomes within a model of regionalization featuring neonatologists at all levels of care, including well-baby nurseries without an accompanying neonatal intensive care unit.
Methods
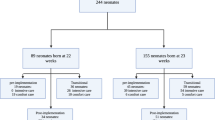
Data were analyzed by NY State adaptation of American Academy of Pediatrics defined levels of care; n = 998, 23–30 weeks gestational age, 400–1250 g birth weight, and admitted to the regional center (2006–2015). Primary outcomes were survival, neurologic survival, and intact survival.
Results
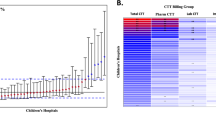
Level III hospitals transferred 82% of neonates ≥24 h of life compared to ≤2% at Level I or II hospitals (p < 0.05). Primary outcomes were equivalent for Levels I vs. II born neonates with similar postnatal age at transfer and similar to inborn rates (Levels I and II vs. IV).
Conclusions
When transferred within 24 h, Levels I or II born infants had equivalent outcomes to inborn Level IV infants in a model of neonatologist availability at all deliveries.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
American Academy of Pediatrics Committee on Fetus and Newborn. Levels of neonatal care. Pediatrics. 2012;130:587–97.
Jensen EA, Lorch SA. Effects of a birth hospital’s neonatal intensive care unit level and annual volume of very low-birth-weight infant deliveries on morbidity and mortality. JAMA Pediatr. 2015;169:e151906.
Lasswell SM, Barfield WD, Rochat RW, Blackmon L. Perinatal regionalization for very low-birth-weight and very preterm infants: a meta-analysis. JAMA. 2010;304:992–1000.
Phibbs CS, Baker LC, Caughey AB, Danielsen B, Schmitt SK, Phibbs RH. Level and volume of neonatal intensive care and mortality in very-low-birth-weight infants. N Engl J Med. 2007;356:2165–75.
Cifuentes J, Bronstein J, Phibbs CS, Phibbs RH, Schmitt SK, Carlo WA. Mortality in low birth weight infants according to level of neonatal care at hospital of birth. Pediatrics. 2002;109:745–51.
Verloove-Vanhorick SP, Verwey RA, Ebeling MC, Brand R, Ruys JH. Mortality in very preterm and very low birth weight infants according to place of birth and level of care: results of a national collaborative survey of preterm and very low birth weight infants in The Netherlands. Pediatrics. 1988;81:404–11.
Shlossman PA, Manley JS, Sciscione AC, Colmorgen GH. An analysis of neonatal morbidity and mortality in maternal (in utero) and neonatal transports at 24–34 weeks’ gestation. Am J Perinatol. 1997;14:449–56.
Lee SK, McMillan DD, Ohlsson A, Boulton J, Lee DS, Ting S, et al. The benefit of preterm birth at tertiary care centers is related to gestational age. Am J Obstet Gynecol. 2003;188:617–22.
Towers CV, Bonebrake R, Padilla G, Rumney P. The effect of transport on the rate of severe intraventricular hemorrhage in very low birth weight infants. Obstet Gynecol. 2000;95:291–5.
Lorch SA, Myers S, Carr B. The regionalization of pediatric health care. Pediatrics. 2010;126:1182–90.
Lorch SA, Baiocchi M, Ahlberg CE, Small DS. The differential impact of delivery hospital on the outcomes of premature infants. Pediatrics. 2012;130:270–8.
Profit J, Gould JB, Bennett M, Goldstein BA, Draper D, Phibbs CS, et al. The association of level of care with NICU quality. Pediatrics. 2016;137:1–9.
Kastenberg ZJ, Lee HC, Profit J, Gould JB, Sylvester KG. Effect of deregionalized care on mortality in very low-birth-weight infants with necrotizing enterocolitis. JAMA Pediatr. 2015;169:26–32.
Ashmeade TL, Haubner L, Collins S, Miladinovic B, Fugate K. Outcomes of a neonatal Golden Hour implementation project. Am J Med Qual. 2016;31:73–80.
Chien LY, Whyte R, Aziz K, Thiessen P, Matthew D, Lee SK, et al. Improved outcome of preterm infants when delivered in tertiary care centers. Obstet Gynecol. 2001;98:247–52.
Wyckoff MH. Initial resuscitation and stabilization of the periviable neonate: the Golden-Hour approach. Semin Perinatol. 2014;38:12–16.
Zecca E, de Luca D, Costa S, Marras M, de Turris P, Romagnoli C. Delivery room strategies and outcomes in preterm infants with gestational age 24–28 weeks. J Matern Fetal Neonatal Med. 2006;19:569–74.
Chung JH, Phibbs CS, Boscardin WJ, Kominski GF, Ortega AN, Needleman J. The effect of neonatal intensive care level and hospital volume on mortality of very low birth weight infants. Med Care. 2010;48:635–44.
Cooke S, Schwartz R, Gagnon DA. A study of the impact of recent developments in the health care environment on perinatal regionalization. Washington, DC: National Perinatal Information Center; 1988.
Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S, et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993–2012. JAMA. 2015;314:1039–51.
Vital Statistics of New York State. http://www.health.ny.gov/statistics/vital_statistics/. Accessed 9 April 2015.
NY State Perinatal Regulations. https://regs.health.ny.gov/content/part-721-perinatal-regionalization. Accessed 9 April 2015.
Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978;92:529–34.
Walsh MC, Kliegman RM. Necrotizing enterocolitis: treatment based on staging criteria. Pediatr Clin N Am. 1986;33:179–201.
Fierson WM, American Academy of Pediatrics Section on Ophthalmology, American Academy of Ophthalmology, American Association for Pediatric Ophthalmology and Strabismus, American Association of Certified Orthoptists. Screening examination of premature infants for retinopathy of prematurity. Pediatrics. 2013;131:189–95.
Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001;163:1723–9.
Warner B, Musial MJ, Chenier T, Donovan E. The effect of birth hospital type on the outcome of very low birth weight infants. Pediatrics. 2004;113 Part 1:35–41.
Fanaroff AA, Wright LL, Stevenson DK, Shankaran S, Donovan EF, Ehrenkranz RA, et al. Very-low-birth-weight outcomes of the National Institute of Child Health and Human Development Neonatal Research Network, May 1991 through December 1992. Am J Obstet Gynecol. 1995;173:1423–31.
McIntire DD, Bloom SL, Casey BM, Leveno KJ. Birth weight in relation to morbidity and mortality among newborn infants. N Engl J Med. 1999;340:1234–8.
Hohlagschwandtner M, Husslein P, Klebermass K, Weninger M, Nardi A, Langer M. Perinatal mortality and morbidity. Comparison between maternal transport, neonatal transport and inpatient antenatal treatment. Arch Gynecol Obstet. 2001;265:113–8.
Kempley ST, Sinha AK, Thames Regional Perinatal Group. Census of neonatal transfers in London and the South East of England. Arch Dis Child Fetal Neonatal Ed. 2004;89:F521–26.
Baschat AA, Cosmi E, Bilardo CM, Wolf H, Berg C, Rigano S, et al. Predictors of neonatal outcome in early-onset placental dysfunction. Obstet Gynecol. 2007;109 Part 1:253–61.
American Academy of Pediatrics Committee on Fetus And Newborn, American College of Obstetricians and Gynecologists Committee on Obstetric Practice. The Apgar score. Pediatrics. 2015;136:819–22.
Kidokoro H, Anderson PJ, Doyle LW, Woodward LJ, Neil JJ, Inder TE. Brain injury and altered brain growth in preterm infants: predictors and prognosis. Pediatrics. 2014;134:e444–53.
Schulman J, Stricof RL, Stevens TP, Holzman IR, Shields EP, Angert RM, et al. Development of a statewide collaborative to decrease NICU central line-associated bloodstream infections. J Perinatol. 2009;29:591–9.
Fenton TR, Kim JH. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 2013;13:59.
Mohamed MA, Aly H. Transport of premature infants is associated with increased risk for intraventricular haemorrhage. Arch Dis Child Fetal Neonatal Ed. 2010;95:F403–07.
Watson A. It is not the ride: inter-hospital transport is not an independent risk factor for intraventricular hemorrhage among very low birth weight infants. J Perinatol. 2013;33:366–70.
Kamath BD, Box TL, Simpson M, Hernandez JA. Infants born at the threshold of viability in relation to neonatal mortality: Colorado, 1991 to 2003. J Perinatol. 2008;28:354–60.
Bacak SJ, Baptiste-Roberts K, Amon E, Ireland B, Leet T. Risk factors for neonatal mortality among extremely-low-birth-weight infants. Am J Obstet Gynecol. 2005;192:862–7.
Howell EA, Hebert P, Chatterjee S, Kleinman LC, Chassin MR. Black/white differences in very low birth weight neonatal mortality rates among New York City hospitals. Pediatrics. 2008;121:e407–15.
Paneth N, Kiely JL, Wallenstein S, Marcus M, Pakter J, Susser M. Newborn intensive care and neonatal mortality in low-birth-weight infants: a population study. N Engl J Med. 1982;307:149–55.
Bartels DB, Wypij D, Wenzlaff P, Dammann O, Poets CF. Hospital volume and neonatal mortality among very low birth weight infants. Pediatrics. 2006;117:2206–14.
Johansson S, Montgomery SM, Ekbom A, Olausson PO, Granath F, Norman M, et al. Preterm delivery, level of care, and infant death in sweden: a population-based study. Pediatrics. 2004;113:1230–5.
Bode MM, O’Shea TM, Metzguer KR, Stiles AD. Perinatal regionalization and neonatal mortality in North Carolina, 1968–1994. Am J Obstet Gynecol. 2001;184:1302–7.
Watson SI, Arulampalam W, Petrou S, Marlow N, Morgan AS, Draper ES, et al. The effects of designation and volume of neonatal care on mortality and morbidity outcomes of very preterm infants in England: retrospective population-based cohort study. BMJ Open. 2014;4:e004856.
Lee HC, Chitkara R, Halamek LP, Hintz SR. A national survey of pediatric residents and delivery room training experience. J Pediatr. 2010;157:158–61 and 153.
Pinheiro JM, Furdon SA, Boynton S, Dugan R, Reu-Donlon C, Jensen S. Decreasing hypothermia during delivery room stabilization of preterm neonates. Pediatrics. 2014;133:e218–26.
Carter BS, Bhatia J. Comfort/palliative care guidelines for neonatal practice: development and implementation in an academic medical center. J Perinatol. 2001;21:279–83.
El Sayed MF, Chan M, McAllister M, Hellmann J. End-of-life care in Toronto neonatal intensive care units: challenges for physician trainees. Arch Dis Child Fetal Neonatal Ed. 2013;98:F528–33.
Maternal and Child Health Services Title V Block Grant FY 2016 Application/FY 2014 Annual Report. https://www.health.ny.gov/community/infants_children/maternal_and_child_health_services/docs/2016_application.pdf. Accessed 20 June 2016.
Nowakowski L, Barfield WD, Kroelinger CD, Lauver CB, Lawler MH, White VA, et al. Assessment of state measures of risk-appropriate care for very low birth weight infants and recommendations for enhancing regionalized state systems. Matern Child Health J. 2012;16:217–27.
Barfield WD. Improving systems in perinatal care: quality, not quantity. JAMA. 2012;307:1750–1.
Acknowledgements
We thank Sergio Golombek, MD, Yogangi Malhotra, MD, and James Hagadorn, MD, MS for their helpful discussions. We also acknowledge Donna Dozor, RN, MS who maintains quality control of the data from which this study was based. We appreciate the physicians and staff of the Maria Fareri Children’s Hospital Regional Perinatal Center who enable this system to function effectively. This project was funded in part by New York State Department of Health, Division of Family Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest
Rights and permissions
About this article
Cite this article
Aboudi, D., Shah, S.I., La Gamma, E.F. et al. Impact of neonatologist availability on preterm survival without morbidities. J Perinatol 38, 1009–1016 (2018). https://doi.org/10.1038/s41372-018-0103-1
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-018-0103-1
This article is cited by
-
Long-term outcomes of children with neonatal transfer: the Japan Environment and Children’s Study
European Journal of Pediatrics (2022)
-
The amniotic fluid cell-free transcriptome in spontaneous preterm labor
Scientific Reports (2021)