Abstract
Objective
To assess whether early NT-ProBNP can identify the need for echocardiographic assessment of hemodynamically significant patent ductus arteriosus (HsPDA) in preterm infants.
Study design
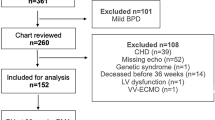
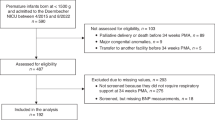
Prospective observational study of infants with a gestational age ≤32 weeks. Echocardiographic assessment and NT-proBNP measurement were performed at 48–96 h. ROC curves were generated to assess optimal cutoffs to detect HsPDA and predict the need for treatment.
Results
Eighty-five patients were included. HsPDA was present in 28 infants (37.6%), and 22 (25.8%) received treatment. The optimal NT-proBNP cutoff for the detection of HsPDA was 5099 pg/mL (sensitivity 94%, specificity 82%, area under the curve 0.941, P < 0.001). Only 1 child with NT-proBNP levels <5099 pg/mL was ultimately treated for PDA. NT-proBNP screening could have avoided 45 of 85 routine echocardiograms (53%).
Conclusion
NT-proBNP screening at 48–96 h of life may identify preterm infants at low risk for HsPDA, improving PDA management.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Hamrick SE, Hansmann G. Patent ductus arteriosus of the preterm infant. Pediatrics. 2010;125:1020–30.
Benitz WE and COMMITTEE ON FETUS AND NEWBORN. Patent Ductus Arteriosus in preterm infants. Pediatrics. 2016;137:e20153730.
Saldeño YP, Favareto V, Mirpuri J. Prolonged persistent patent ductus arteriosus: potential perdurable anomalies in premature infants. J Perinatol. 2012;32:953.
M Benitz WE. Treatment of persistent patent ductus arteriosus in preterm infants: time to accept the null hypothesis”. J Perinatol. 2010;30:241–52.
Clyman RI, Couto J, Murphy GM. Patent ductus arteriosus: are current neonatal treatment options better or worse than no treatment at all. Semin Perinatol. 2012;36:123–9.
Raval MV, Laughon MM, Bose CL, Phillips JD. Patent ductus arteriosus ligation in premature infants: Who really benefits, and at what cost? J Pediatr Surg. 2007;42:69–75.
Bose CL, Laughon M. Patent ductus arteriosus: lack evidence for common tratments. Arch Dis Child Fetal Neonatal Ed. 2007;92:498–502.
Benitz WE. Learning to live with patency of the ductus arteriosus in preterm infants. J Perinatol. 2011;31 Suppl 1:S42–S48.
Fortunato Visconti L, Saady Morhy S, D’Agostini Deutsch A, Penha Tavares GM, Jardim Mussi WT, et al. Clinical and echocardiographic characteristics associated with the evolution of the ductus arteriosus in the neonate with birth weight lower than 1,500g. Einstein. 2013;11:317–23.
McNamara PJ, Sehgal A. Towards rational management of the patent ductus arteriosus: the need for disease staging”. Arch Dis Child Fetal Neonatal Ed. 2007;92:F424–7.
Sanjeev S, Pettersen M, Lua J, Thomas R, Shankaran S, L’Ecuyer T. Role of plasma B- type natriuretic peptide in screening for hemodynamically significant patent ductus arteriosus in preterm neonates. J Perinatol. 2005;25:709–13.
Buddhe S, Dhuper S, Kim R, Weichbrod L, Mahdi E, Shah N, et al. NT-proBNP levels improve the ability of predicting a hemodynamically significant patent ductus arteriosus invery low-birth-weight infants. J Clin Neonatol. 2012;1 Issue 2. https://doi.org/10.4103/2249.
El Khuffash AF, Amoruso M, Culliton M, Molloy EJ. N-terminal pro-B-type natriuretic peptide as a marker of ductal haemodynamic significance in preterm infants: a prospective observational study. Arch Dis Child Fetal Neonatal Ed. 2007;92:F421–2.
Farombi-Oghuvbu I, Matthews T, Mayne PD, Guerin H, Corcoran JD. N-terminal pro-B-type natriuretic peptide: a measure of significant patent ductus arteriosus. Arch Dis Child Fetal Neonatal Ed. 2008;93:F257–F260.
Holmstrom H, Hall C, Thaulow E. Plasma levels of natriuretic peptides and hemodynamic assessment of patent ductus arteriosus in preterm infants. Acta Paediatr. 2001;90:184–91.
Barnes SC, Collinson PO, Galasko G, Lahiri A, Senior R. Evaluation of N-terminal pro-B type natriuretic peptide analysis on the Elecsys 1010 and 2010 analysers. Ann Clin Biochem. 2004;41:459–63.
Chen YY, Wang HP, Chang JT, Chiou YH, Huang YF, Hsieh KS, Premature Infant Development Collaborative Study Group. et al. Perinatal factors in patent ductus arteriosus in very low-birthweight infants. Pediatr Int. 2014;56:72–76.
El-Khuffash A, James AT, Corcoran JD, Dicker P, Franklin O, Elsayed YN, et al. A patent ductus arteriosus severity score predicts chronic lung disease or death before discharge. J Pediatr. 2015;167:1354–61.
Bagnoli F, Rossetti A, Casucci M, Mori A. Aminoterminal B-Type Natriuretic Peptido (NT-proBNP) in the therapy of patent ductus arteriosus. Minerva Pediatr. 2010;62:67–70.
Czernik C, Lemmer J, Metze B, Koehne PS, Mueller C, Obladen M. B-type natriuretic peptide to predict ductus intervention in infants <28 weeks. Pediatr Res. 2008;64:286–90.
Attridge JT, Kaufman DA, Lim DS. B-type natriuretic peptide concentrations to guide treatment of patent ductus arteriosus. Arch Dis Child Fetal Neonatal Ed. 2009;94:F178–82.
Hsu JH, Yang SN, Chen HL, Tseng HI, Dai ZK, Wu JR. B-type natriuretic peptide predicts responses to indomethacin in premature neonates with patent ductus arteriosus. J Pediatr. 2010;157:79–84.
Nuntnarumit P, Chongkongkiat P, Khositseth A. N-terminal-pro-brain natriuretic peptide: a guide for early targeted indomethacin therapy for patent ductus arteriosus in preterm Infants. Acta Paediatr. 2011;100:1217–21.
Czernik C, Metze B, Müller C, Bührer C. Urinary NT-proBNP and ductal closure in preterm infants. J Perinatol. 2013;33:212–7.
Choi BM, Lee KH, Eun BL, et al. Utility of rapid B-type natriuretic peptide assay for diagnosis of symptomatic patent ductus arteriosus in preterm infants. Pediatrics. 2005;115:e255–61.
Ramakrishnan S, Heung YM, Round J, Morris TP, Collinson P, Williams AF. Early N-terminal pro-brain natriuretic peptide measurements predict clinically significant ductus arteriosus in preterm infants. Acta Paediatr. 2009;98:1254–9.
Hall C. Essential biochemistry and physiology of NT-proBNP. Eur J Heart Fail. 2004;6:257–60.
Witthaut R. Science review: Natriuretic peptides in critical illness. Crit Care. 2004;8:342–9.
Cantinotti M, Walters HL, Crocetti M, Marotta M, Murzi B, Clerico A. BNP in children with congenital cardiac disease: is there now sufficient evidence for its routine use? Cardiol Young. 2015;25:424–37.
da Graca RL, Hassinger DC, Flynn PA, Sison CP, Nesin M, Auld PA. Longitudinal changes of brain- type natriuretic peptide in preterm neonates. Pediatrics. 2006;117:2183–9.
Cantinotti M, Law Y, Vittorini S, Crocetti M, Marco M, Murzi B, et al. The potential and limitations of plasma BNP measurement in the diagnosis, prognosis, and management of children with heart failure due to congenital cardiac disease: an update. Heart Fail Rev. 2014;19:727–42.
Rudiger A, Gasser S, Fischler M, Hornemann T, von EA, Maggiorini M. Comparable increase of B-type natriuretic peptide and amino-terminal pro-B-type natriuretic peptide levels in patients with severe sepsis, septic shock, and acute heart failure. Crit Care Med. 2006;34:2140–4.
Gonzalez A, Sosenko IR, Chandar J, Hummler H, Claure N, Bancalari E. Influence of infection on patent ductus arteriosus and chronic lung disease in premature infants weighing 1000 grams or less. J Pediatr. 1996;128:470–8.
Bertoldi EG, Stella SF, Rohde LE, Polanczyk CA. Long-term cost-effectiveness of diagnostic tests for assessing stable chest pain: modeled analysis of anatomical and functional strategies. Clin Cardiol. 2016;39:249–56.
Czernik C, Metze B, Muller C, Muller B, Buhrer C. Urinary N-terminal B-type natriuretic peptide predicts severe retinopathy of prematurity. Pediatrics. 2011;128:e545–e549.
Zhang Qian, Shi ZanYang, Luo ChengHan, Wang Li, Zhang ShanShan, Cheng XinRu, et al. Application of NT-proBNP in ventilator weaning for preterm infants with RDS. Pediatr Pulmonol. 2013;49:757–63.
Acknowledgements
We would like to thank all our colleagues at the NICU for their excellent day-to-day work and for believing in this project from the beginning. We would also like to particularly thank our patients and their families.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Rodriguez-Blanco, S., Oulego-Erroz, I., Gautreaux-Minaya, S. et al. Early NT-proBNP levels as a screening tool for the detection of hemodynamically significant patent ductus arteriosus during the first week of life in very low birth weight infants. J Perinatol 38, 881–888 (2018). https://doi.org/10.1038/s41372-018-0123-x
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-018-0123-x
This article is cited by
-
NT-PROBNP as a screening tool for low-risk patent ductus arteriousus: a follow-up validation study
European Journal of Pediatrics (2023)