Abstract
Objective
To determine the relative effects of patient and hospital factors on a hospital’s postpartum readmission rate.
Study design
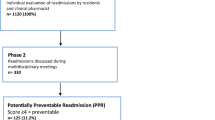
This retrospective cohort study was conducted using State Inpatient Databases from California, Florida, and New York between 2004 and 2013. We compared patient and hospital characteristics among hospitals with low and high readmission rates using χ2 tests. Risk-adjusted 30-day readmission rates were calculated for patient, delivery, and hospital characteristics to understand factors affecting readmission using fixed and random effects models.
Results
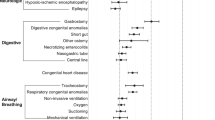
Patients in hospitals with low readmission rates were more likely to be white, to have private insurance and higher incomes, and to have fewer comorbidities. The patient comorbidities with the highest risk-adjusted readmission rates included hypertension (range, 2.14–3.04%), obesity (1.78–2.94%), preterm labor/delivery (2.50–2.60%), and seizure disorder (1.78–3.35%). Delivery complications were associated with increased risk-adjusted readmission rates. Compared to patient characteristics, hospital characteristics did not have a profound impact on readmission risk.
Conclusion
Obstetric readmissions were more attributable to patient and demographic characteristics than to hospital characteristics. Readmission metric-based incentives may ultimately penalize hospitals providing high-quality care due to patient characteristics specific to their catchment area.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Jha AK, Orav EJ, Epstein AM. Public reporting of discharge planning and rates of readmissions. N Engl J Med. 2009;361:2637–45.
Tsai TC, Joynt KE, Orav EJ, Gawande AA, Jha AK. Variation in surgical-readmission rates and quality of hospital care. N Engl J Med. 2013;369:1134–42.
Epstein AM, Jha AK, Orav EJ. The relationship between hospital admission rates and rehospitalizations. N Engl J Med. 2011;365:2287–95.
Centers for Medicare and Medicaid Services. Readmissions Reduction Program [Internet]. 2016. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html. Accessed 17 Sept 2016.
Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, observation, and the hospital readmissions reduction program. N Engl J Med. 2016;374:1543–51.
Joynt KE, Jha AK. Characteristics of hospitals receiving penalties under the hospital readmissions reduction program. JAMA. 2013;309:342–3.
Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA. 2011;305:675–81.
Joynt KE, Jha AK. A path forward on Medicare readmissions. N Engl J Med. 2013;368:1175–7.
Bailit JL, Gregory KD, Srinivas S, Westover T, Grobman WA, Saade GR. Society for maternal-fetal medicine (SMFM) special report: current approaches to measuring quality of care in obstetrics. Am J Obstet Gynecol. 2016;215:B8–16.
Clapp MA, Little SE, Zheng J, Robinson JN. A multi-state analysis of postpartum readmissions in the United States. Am J Obstet Gynecol. 2016;215:113.e1–113.e10.
Kuklina EV, Whiteman MK, Hillis SD, Jamieson DJ, Meikle SF, Posner SF, et al. An enhanced method for identifying obstetric deliveries: implications for estimating maternal morbidity. Matern Child Health J. 2008;12:469–77.
Kozhimannil KB, Law MR, Virnig BA. Cesarean delivery rates vary tenfold among US hospitals; reducing variation may address quality and cost issues. Health Aff. 2013;32:527–35.
Armstrong JC, Kozhimannil KB, McDermott P, Saade GR, Srinivas SK, Society for Maternal-Fetal Medicine Health Policy Committee. Comparing variation in hospital rates of cesarean delivery among low-risk women using 3 different measures. Am J Obstet Gynecol. 2016;214:153–63.
Little SE, Orav EJ, Robinson JN, Caughey AB, Jha AK. The relationship between variations in cesarean delivery and regional health care use in the United States. Am J Obstet Gynecol. 2016;214:735.e1–8.
Clapp MA, Little SE, Zheng J, Kaimal AJ, Robinson JN. Hospital-level variation in postpartum readmissions. JAMA. 2017;317:2128–9.
Healthcare Cost and Utilization Project. HCUP methods series: overview of key readmission measures and methods [Internet]. Rockville, MD: Agency for Healthcare Research and Quality; 2012.
Wasfy JH, Strom JB, Waldo SW, O’Brien C, Wimmer NJ, Zai AH, et al. Clinical preventability of 30-day readmission after percutaneous coronary intervention. J Am Heart Assoc. 2014;3:e001290.
Auerbach AD, Kripalani S, Vasilevskis EE, Sehgal N, Lindenauer PK, Metlay JP, et al. Preventability and causes of readmissions in a national cohort of general medicine patients. JAMA Intern Med. 2016;176:484–93.
Rathore SS, Foody JM, Wang Y, Smith GL, Herrin J, Masoudi FA, et al. Race, quality of care, and outcomes of elderly patients hospitalized with heart failure. JAMA. 2003;289:2517–24.
Acknowledgements
This work was supported by an institutional grant awarded to the authors by the Center of Expertise in Health Policy and Management from the Partners Healthcare Office of Graduate Medical Education.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Clapp, M.A., Little, S.E., Zheng, J. et al. The relative effects of patient and hospital factors on postpartum readmissions. J Perinatol 38, 804–812 (2018). https://doi.org/10.1038/s41372-018-0125-8
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41372-018-0125-8
This article is cited by
-
Providing and Measuring Quality Postpartum Care
Current Obstetrics and Gynecology Reports (2022)