Abstract
Objective
To evaluate the neurodevelopmental outcomes of preterm very-low birth weight (PT/VLBW) infants at 2 years and identify risk factors associated with significant developmental delay or neurodevelopmental impairment (NDI).
Study design
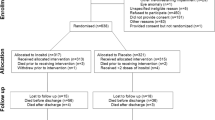
We evaluated 165 PT/VLBW infants born between January 2010 and December 2011, using the Bayley Scales of Infant and Toddler Development 3rd Edition (Bayley-III). NDI was defined as the presence of neurosensory impairment or significant delay with Bayley-III score < 70 in any domain and risk factors for delay/NDI were assessed using logistic regressions.
Results
Median Bayley-III composite scores in the cognitive, language and motor domains were 95, 89 and 94, respectively. NDI was present in 20% of the children, with 5–18% having significant delay in either cognitive, language or motor domain, seven (4%) children had cerebral palsy, three (2%) were deaf and none were blind. Regression models identified significant positive associations of delayed cognitive skills with male gender (Odds ratio (OR) 22.4, 95% confidence interval (CI) 1.5–341.1; P = 0.025), lack of anntenatal steroids (ANS) (OR 41.5, 95% CI 3.5–485.7; P = 0.003), and hypotension needing inotropes (OR 36.0, 95% CI 2.6–506.0; P = 0.008); delayed language skills with lower maternal education (OR 3.8, 95% CI 1.4–10.3; P = 0.10), lack of ANS (OR 2.8, 95% CI 1.1–7.4; P = 0.04), and 5 minute Apgar Score ≤ 5 (OR 7.4, 95% CI 1.4–38.4; P = 0.017) and delayed motor skills with chronic lung disease at 36 weeks (OR 38.3, 95% CI 2.4–603.4; P = 0.010). NDI was associated with lack of ANS (OR 2.91, 95% CI 1.21–7.00; P = 0.02) and use of postnatal steroids (OR 3.36, 95% CI 1.07–10.54; P = 0.0374).
Conclusion
Risk factors for both NDI and individual domain delay were identified and will be helpful in planning of specific and targeted early intervention services.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Agarwal P, Sriram B, Rajadurai V. Neonatal outcome of extremely preterm Asian infants ≤28 weeks over a decade in the new millennium. J Perinatol. 2015;35:297–303.
Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics. 2010;126:443–56.
Patel RM. Short-and long-term outcomes for extremely preterm infants. Am J Perinatol. 2016;33:318–28.
Rogers EE,Hintz SR, Early neurodevelopmental outcomes of extremely preterm infants. Semin Perinatol. 2016;40:497–509.
Schmidt B, Asztalos EV, Roberts RS, Robertson CM, Sauve RS, Whitfield MF, et al. Impact of bronchopulmonary dysplasia, brain injury, and severe retinopathy on the outcome of extremely low-birth-weight infants at 18 months: results from the trial of indomethacin prophylaxis in preterms. JAMA. 2003;289:1124–9.
Bassler D, Stoll BJ, Schmidt B, Asztalos EV, Roberts RS, Robertson CM, et al. Using a count of neonatal morbidities to predict poor outcome in extremely low birth weight infants: added role of neonatal infection. Pediatrics. 2009;123:313–8.
Kumar P, Shankaran S, Ambalavanan N, Kendrick DE, Pappas A, Vohr BR, et al. Characteristics of extremely low-birth-weight infant survivors with unimpaired outcomes at 30 months of age. J Perinatol. 2013;33:800–5.
Ong L, Boo N, Chandran V. Predictors of neurodevelopmental outcome of Malaysian very low birthweight children at 4 years of age. J Paediatr Child Health. 2001;37:363–8.
Daniel L, Lim S, Clarke L. Eight-year outcome of very-low-birth-weight infants born in KK hospital. Ann Acad Med Singap. 2003;32:354–61.
Bayley N. Bayley scales of infant and toddler development. United States: Pearson; 2006.
Stephens BE, Walden RV, Gargus RA, Tucker R, McKinley L, Mance M, et al. First-week protein and energy intakes are associated with 18-month developmental outcomes in extremely low birth weight infants. Pediatrics. 2009;123:1337–43.
Serenius F, Källén K, Blennow M, Ewald U, Fellman V, Holmström G, et al. Neurodevelopmental outcome in extremely preterm infants at 2.5 years after active perinatal care in Sweden. JAMA. 2013;309:1810–20.
Synnes A, Luu TM, Moddemann D, Church P, Lee D, Vincer M, et al. Determinants of developmental outcomes in a very preterm Canadian cohort. Arch Dis Child Fetal Neonatal Ed. 2017;102:F235–F4.
Doyle LW, Roberts G, Anderson PJ, Group VICS. Outcomes at age 2 years of infants 28 weeks’ gestational age born in Victoria in 2005. J Pediatr. 2010;156:49–53.
Anderson PJ, De Luca CR, Hutchinson E, Roberts G, Doyle LW. Underestimation of developmental delay by the new Bayley-III Scale. Arch Pediatr Adolesc Med. 2010;164:352–6.
Aylward GP. Continuing issues with the Bayley-III: where to go from here. J Dev Behav Pediatr. 2013;34:697–701.
Vohr BR, Stephens BE, Higgins RD, Bann CM, Hintz SR, Das A, et al. Are outcomes of extremely preterm infants improving? Impact of Bayley assessment on outcomes. J Pediatr. 2012;161:222–8. e3
Vohr BR. Neurodevelopmental outcomes of extremely preterm infants. Clin Perinatol. 2014;41:241–55.
Kilbride H, Aylward G, Doyle L, Singer L, Lantos J. Prognostic neurodevelopmental testing of preterm infants: do we need to change the paradigm? J Perinatol. 2017;37:475–9.
Spittle A, Treyvaud K. The role of early developmental intervention to influence neurobehavioral outcomes of children born preterm. Semin Perinatol. 2016;40:542–48.
Linsell L, Malouf R, Morris J, Kurinczuk JJ, Marlow N. Prognostic factors for poor cognitive development in children born very preterm or with very low birth weight: a systematic review. JAMA Pediatr. 2015;169:1162–72.
Sotiriadis A, Tsiami A, Papatheodorou S, Baschat AA, Sarafidis K, Makrydimas G. Neurodevelopmental outcome after a single course of antenatal steroids in children born preterm: a systematic review and meta-analysis. Obstet & Gynecol. 2015;125:1385–96.
Chawla S, Natarajan G, Shankaran S, Pappas A, Stoll BJ, Carlo WA, et al. Association of neurodevelopmental outcomes and neonatal morbidities of extremely premature infants with differential exposure to antenatal steroids. JAMA Pediatr. 2016;170:1164–72.
Wong D, Abdel-Latif M, Kent A. Antenatal steroid exposure and outcomes of very premature infants: a regional cohort study. Arch Dis Child Fetal Neonatal Ed. 2014;99:F12–F20.
Stonestreet BS, Petersson KH, Sadowska GB, Pettigrew KD, Patlak CS. Antenatal steroids decrease blood-brain barrier permeability in the ovine fetus. Am J Physiol Regul Integr Comp Physiol. 1999;276:R283–R9.
Kent AL, Wright IM, Abdel-Latif ME. Mortality and adverse neurologic outcomes are greater in preterm male infants. Pediatrics. 2012;129:124–31.
DiPietro J, Voegtline K. The gestational foundation of sex differences in development and vulnerability. Neuroscience. 2015;342:4–20.
Wong HS, Edwards P. Nature or nurture: a systematic review of the effect of socioeconomic status on the developmental and cognitive outcomes of children born preterm. Matern Child Health J. 2013;17:1689–700.
Vohr BR. Language and hearing outcomes of preterm infants. Semin Perinatol. 2016;40:510–19.
Luu TM, Vohr BR, Allan W, Schneider KC, Ment LR. Evidence for catch-up in cognition and receptive vocabulary among adolescents born very preterm. Pediatrics. 2011;128:313-22.
Doyle LW, Anderson PJ, editors. Long-term outcomes of bronchopulmonary dysplasia. Semin Fetal Neonatal Med. 2009;14:391–5.
Singer L, Yamashita T, Lilien L, Collin M, Baley J. A longitudinal study of developmental outcome of infants with bronchopulmonary dysplasia and very low birth weight. Pediatrics. 1997;100:987–93.
Gagliardi L, Bellù R, Zanini R, Dammann O. Bronchopulmonary dysplasia and brain white matter damage in the preterm infant: a complex relationship. Paediatr Perinat Epidemiol. 2009;23:582–90.
Laughon M, O’Shea MT, Allred EN, Bose C, Kuban K, Van Marter LJ, et al. Chronic lung disease and developmental delay at 2 years of age in children born before 28 weeks’ gestation. Pediatrics. 2009;124:637–48.
Wood N, Costeloe K, Gibson A, Hennessy E, Marlow N, Wilkinson A. The EPICure study: associations and antecedents of neurological and developmental disability at 30 months of age following extremely preterm birth. Arch Dis Child Fetal Neonatal Ed. 2005;90:F134–F40.
Doyle LW, Halliday HL, Ehrenkranz RA, Davis PG, Sinclair JC. Impact of postnatal systemic corticosteroids on mortality and cerebral palsy in preterm infants: effect modification by risk for chronic lung disease. Pediatrics. 2005;115:655–61.
Soh S-E, Tint MT, Gluckman PD, Godfrey KM, Rifkin-Graboi A, Chan YH, et al. Cohort profile: growing up in singapore towards healthy outcomes (GUSTO) birth cohort study. Int J Epidemiol. 2013;43:1401–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Agarwal, P.K., Shi, L., Rajadurai, V.S. et al. Factors affecting neurodevelopmental outcome at 2 years in very preterm infants below 1250 grams: a prospective study. J Perinatol 38, 1093–1100 (2018). https://doi.org/10.1038/s41372-018-0138-3
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41372-018-0138-3
This article is cited by
-
Association of low hemoglobin at birth and neurodevelopmental outcomes in preterm neonates ≤28 weeks’ gestation: a retrospective cohort study
Journal of Perinatology (2024)
-
Effect of medically assisted reproduction (MAR) and pregnancy planning on Bayley-III Screening Test subscales in preterm infants at 12 months of corrected age: a cross-sectional study
Italian Journal of Pediatrics (2022)
-
A prospective cohort study of the association between the Apgar score and developmental status at 3 years of age: the Japan Environment and Children’s Study (JECS)
European Journal of Pediatrics (2022)
-
Quality improvement project designed to reduce disproportionate growth in extremely low gestational age neonates: cognitive neurodevelopmental outcome at 18–41 months
Journal of Perinatology (2021)