Abstract
Objective
The objective of this study is to measure delivery length of stay (LOS) and cost as proxies for infant morbidity in assisted reproductive technology (ART) and subfertile deliveries.
Study Design
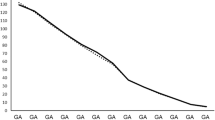
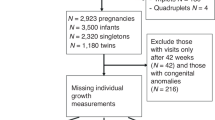
Massachusetts singleton births, ≥ 23 weeks gestational age (GA) between 2004 and 2010, were linked with ART data, vital records, and hospital discharges. LOS and costs (2010 US dollars) of infants born to fertile (no ART or indicators of infertility), subfertile (indicators of infertility but no ART), and ART-treated (linked to ART data) deliveries were compared. Least-square means and SE were calculated.
Results
Of 345,756 singletons (fertile n = 332,481, subfertile n = 4987, and ART-treated n = 8288), overall LOS was 3.79 ± 0.01, 4.32 ± 0.15, and 4.90 ± 0.04 days, and costs were $2980 ± 6, $3217 ± 58, and $4483 ± 62, respectively. GA and birthweight predicted much of the intergroup difference.
Conclusion
Maternal fertility group was not an independent predictor of infant LOS and costs. Prematurity and birthweight were driving factors in resource utilization.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Fineberg HV. Shattuck lecture. A successful and sustainable health system--how to get there from here. N Engl J Med. 2012;366:1020–7.
Porter ME, Lee TH. Why strategy matters now. N Engl J Med. 2015;372:1681–4.
Chambers GM, Sullivan EA, Ishihara O, Chapman MG, Adamson GD. The economic impact of assisted reproductive technology: a review of selected developed countries. Fertil Steril. 2009;91:2281–94.
Lee MS, Evans BT, Stern AD, Hornstein MD. Economic implications of the Society for Assisted Reproductive Technology embryo transfer guidelines: healthcare dollars saved by reducing iatrogenic triplets. Fertil Steril. 2016;106:189–95 e3.
Group ECW. Economic aspects of infertility care: a challenge for researchers and clinicians. Hum Reprod. 2015;30:2243–8.
Luke B, Stern JE, Kotelchuck M, Declercq ER, Cohen B, Diop H. Birth outcomes by infertility diagnosis analyses of the Massachusetts Outcomes Study of Assisted Reproductive Technologies (MOSART). J Reprod Med. 2015;60:480–90.
Messerlian C, Maclagan L, Basso O. Infertility and the risk of adverse pregnancy outcomes: a systematic review and meta-analysis. Hum Reprod. 2013;28:125–37.
Carpinello OJ, Casson PR, Kuo CL, Raj RS, Sills ES, Jones CA. Cost implications for subsequent perinatal outcomes after IVF stratified by number of embryos transferred: a five year analysis of vermont data. Appl Health Econ Health Policy. 2016;14:387–95.
Chambers GM, Hoang VP, Lee E, Hansen M, Sullivan EA, Bower C, et al. Hospital costs of multiple-birth and singleton-birth children during the first 5 years of life and the role of assisted reproductive technology. JAMA Pediatr. 2014;168:1045–53.
Raju TNK, Buist AS, Blaisdell CJ, Moxey-Mims M, Saigal S. Adults born preterm: a review of general health and system-specific outcomes. Acta Paediatr. 2017; 106:1409–437.
Chambers GM, Chapman MG, Grayson N, Shanahan M, Sullivan EA. Babies born after ART treatment cost more than non-ART babies: a cost analysis of inpatient birth-admission costs of singleton and multiple gestation pregnancies. Hum Reprod. 2007;22:3108–15.
Williams MA, Goldman MB, Mittendorf R, Monson RR. Subfertility and the risk of low birth weight. Fertil Steril. 1991;56:668–71.
Declercq E, Luke B, Belanoff C, Cabral H, Diop H, Gopal D, et al. Perinatal outcomes associated with assisted reproductive technology: the Massachusetts Outcomes Study of Assisted Reproductive Technologies (MOSART). Fertil Steril. 2015;103:888–95.
Luke B, Stern JE, Kotelchuck M, Declercq ER, Anderka M, Diop H. Birth outcomes by infertility treatment: analyses of the population-based cohort: Massachusetts Outcomes Study of Assisted Reproductive Technologies (MOSART). J Reprod Med. 2016;61:114–27.
Sunderam S, Kissin DM, Crawford SB, Folger SG, Jamieson DJ, Warner L, et al. Assisted reproductive technology surveillance - United States, 2012. MMWR Surveill Summ. 2015;64:1–29.
Declercq E, Barger M, Cabral HJ, Evans SR, Kotelchuck M, Simon C, et al. Maternal outcomes associated with planned primary cesarean births compared with planned vaginal births. Obstet Gynecol. 2007;109:669–77.
Derrington TM, Kotelchuck M, Plummer K, Cabral H, Lin AE, Belanoff C, et al. Racial/ethnic differences in hospital use and cost among a statewide population of children with Down syndrome. Res Dev Disabil. 2013;34:3276–87.
Weiss J, Kotelchuck M, Grosse SD, Manning SE, Anderka M, Wyszynski DF, et al. Hospital use and associated costs of children aged zero-to-two years with craniofacial malformations in Massachusetts. Birth Defects Res A Clin Mol Teratol. 2009;85:925–34.
Zegers-Hochschild F, Adamson GD, Dyer S, Racowsky C, de Mouzon J, Sokol R, et al. The International Glossary on Infertility and Fertility Care, 2017. Fertil Steril. 2017;108:393–406.
Thompson SG, Nixon RM, Grieve R. Addressing the issues that arise in analysing multicentre cost data, with application to a multinational study. J Health Econ. 2006;25:1015–28.
Hwang SS, Dukhovny D, Gopal D, Cabral H, Missmer S, Diop H, et al. Health of Infants After ART-Treated, Subfertile, and Fertile Deliveries. Pediatrics. 2018; 142: pii: e20174069.
Phibbs CS, Schmitt SK. Estimates of the cost and length of stay changes that can be attributed to one-week increases in gestational age for premature infants. Early Hum Dev. 2006;82:85–95.
Chambers GM, Lee E, Hoang VP, Hansen M, Bower C, Sullivan EA. Hospital utilization, costs and mortality rates during the first 5 years of life: a population study of ART and non-ART singletons. Hum Reprod. 2014;29:601–10.
Association of Women’s Health O, Neonatal N. Infertility treatment as a covered health insurance benefit. Nurs Women’s Health. 2014;18:175–6.
Mowitz ME, Zupancic JA, Millar D, Kirpalani H, Gaulton JS, Roberts RS, et al. Prospective economic evaluation alongside the non-invasive ventilation trial. J Perinatol. 2017;37:61–6.
Patel AL, Johnson TJ, Robin B, Bigger HR, Buchanan A, Christian E, et al. Influence of own mother’s milk on bronchopulmonary dysplasia and costs. Arch Dis Child Fetal Neonatal Ed. 2017;102:F256–F61.
Henderson J, Hockley C, Petrou S, Goldacre M, Davidson L. Economic implications of multiple births: inpatient hospital costs in the first 5 years of life. Arch Dis Child Fetal Neonatal Ed. 2004;89:F542–5.
Diop H, Gopal D, Cabral H, Belanoff C, Declercq ER, Kotelchuck M, et al. Assisted reproductive technology and early intervention program enrollment. Pediatrics. 2016;137:e20152007.
Acknowledgements
Society for Assisted Reproductive Technology (SART) wishes to thank all of its members for providing clinical information to the SART CORS database for the use by patients and researchers. Without the efforts of our members, this research would not have been possible.
Funding
This study was supported by the National Institutes of Health R01HD067270.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interests.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Dukhovny, D., Hwang, S.S., Gopal, D. et al. Length of stay and cost of birth hospitalization: effects of subfertility and ART. J Perinatol 38, 1457–1465 (2018). https://doi.org/10.1038/s41372-018-0205-9
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41372-018-0205-9